Voltaren Patch for pain in the back, muscles and joints, transdermal patch 15 mg/day No. 2
A country
Greece, Japan
The country of production may vary depending on the batch of goods. Please check with the operator for detailed information when confirming your order.
Description
Voltaren is the only therapeutic patch.* The components of the patch are continuously delivered to the source of pain, eliminating pain and inflammation.
Used for: - Back pain due to inflammatory and degenerative diseases of the spine - Joint pain - Muscle pain - Inflammation and swelling of soft tissues and joints due to injuries and rheumatic diseases. It is enough to apply only 1 patch for 24 hours**. Advantages of the Voltaren patch: • Applied once a day • Invisible under clothing (ultra-thin, flesh-colored) • Does not stain hands and clothes * Among Voltaren products in Russia ** Instructions for medical use, RU No. LP-001089
Compound
Each transdermal patch 15 mg/day (70 cm2) contains: Active ingredient: 15 mg diclofenac sodium (1%). Excipients: levomenthol 22.5 mg, methylpyrrolidone 60.0 mg, propylene glycol esters of fatty acids 30.0 mg, citric acid 6.0 mg, isoprene styrene copolymer 536.1 mg, polyisobutylene 30.0 mg, esterified gum 300.0 mg , mercaptobenzimidazole 3.7 mg, butylated hydroxytoluene 3.7 mg, liquid paraffin up to 1500.00 mg; base made of polyester fibers (50 den) 70 cm2; protective film made of polyester (thickness 75 microns) 70 cm2.
Product description
Rectangular patches with rounded edges, consisting of a beige polyester base with a uniformly applied adhesive layer from colorless to pale yellow with a faint aromatic odor. The adhesive surface is covered with a transparent protective film of polyethylene with two transverse cuts, one of which has a wavy line. A drawing is applied to the transparent protective film showing how to remove the film from the surface of the patch. The size of the patch is 70 x 100 mm.
pharmachologic effect
Voltaren® in the form of a transdermal patch is a base with an applied adhesive layer containing diclofenac, which has pronounced analgesic and anti-inflammatory properties.
The mechanisms of action of diclofenac are based on inhibition of prostaglandin synthesis. The Voltaren® patch provides anti-inflammatory and analgesic effects at the site of application, eliminating pain and reducing swelling associated with the inflammatory process. Pharmacokinetics Absorption and distribution in the body: The amount of diclofenac absorbed systemically from the Voltaren® patch over 24 hours is similar to that when using an equivalent amount of Voltaren® Emulgel® (gel for external use 1%). 99.7% of diclofenac is bound to serum proteins, mainly to albumin (99.4%). Elimination: The total systemic clearance of diclofenac from plasma is 263 ± 56 ml/min. The terminal half-life in plasma is 1-2 hours. Four metabolites, including two active ones, also have a short half-life of 1-3 hours. One metabolite, 3`-hydroxy-4`-methoxydiclofenac, has a longer half-life, however, is inactive. Diclofenac and its metabolites are excreted mainly in the urine. In patients with impaired renal function, accumulation of diclofenac and its metabolites does not occur. In patients suffering from chronic hepatitis or undecompensated cirrhosis, the kinetics and metabolism of diclofenac follow the same pattern as in patients without liver disease. Preclinical studies have shown the safety of using the drug.
Indications for use
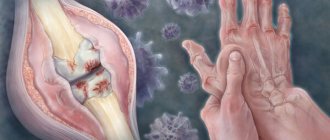
Back pain due to inflammatory and degenerative diseases of the spine (sciatica, osteoarthritis, lumbago, sciatica). Pain in the joints (fingers, knees, etc.) with osteoarthritis. Muscle pain (due to sprains, strains, bruises, injuries). Inflammation and swelling of soft tissues and joints due to injuries and rheumatic diseases (tenosynovitis, bursitis, lesions of periarticular tissues).
Contraindications
Hypersensitivity to diclofenac or other components of the drug; tendency to develop attacks of bronchial asthma, skin rashes or acute rhinitis when using acetylsalicylic acid or other NSAIDs; pregnancy (III trimester); breast-feeding; children's age (up to 15 years); violation of the integrity of the skin at the site where the patch is supposed to be applied. With caution: hepatic porphyria (exacerbation), erosive and ulcerative lesions of the gastrointestinal tract, severe dysfunction of the liver and kidneys, chronic heart failure, bronchial asthma, old age.
Use during pregnancy and lactation
The use of the drug in pregnant women has not been studied, therefore the Voltaren® patch should not be used during pregnancy, especially in the third trimester due to the possibility of decreased uterine tone and/or premature closure of the fetal ductus arteriosus. Animal studies have not revealed any direct or indirect negative effects on pregnancy, childbirth, embryonic or post-embryonic development. There is no data on the penetration of the drug into breast milk, therefore the Voltaren® patch is not recommended for use during breastfeeding.
Directions for use and doses
Externally in the form of applications to the skin. Adults and adolescents over 15 years of age: The Voltaren® patch is applied to the skin over the painful area for 24 hours. Only 1 patch is allowed to be used per day. When treating soft tissue injuries, the Voltaren® patch is used for no more than 14 days, and when treating diseases of muscles and joints - no more than 21 days, unless there are special recommendations from a doctor. If there is no improvement after 7 days and if your health worsens, you should consult a doctor. Children: The use of Voltaren® patch in children under 15 years of age is not recommended. Elderly: Similar to the method of administration and doses for adults
Side effect
Adverse reactions are mainly characterized by moderate and transient skin manifestations at the site of application of the patch. Very rare manifestations (Overdose) The extremely low systemic absorption of the active components and the dosage form of the drug when used externally makes an overdose almost impossible.
Interaction with other drugs
Voltaren® patch may enhance the effect of drugs that cause photosensitivity. Clinically significant interactions with other drugs have not been described.
special instructions
The Voltaren® patch should only be applied to intact skin, avoiding contact with open wounds. The drug should not come into contact with the eyes and mucous membranes. When using the Voltaren® patch for too long a time, the possibility of developing systemic adverse reactions cannot be excluded. When additionally using other dosage forms of diclofenac, its quantitative content in the patch should be taken into account so as not to exceed the maximum daily dose of diclofenac (150 mg/day).
Release form
Transdermal patch 15 mg/day (area 70 cm2). 2 patches in an aluminum foil bag. Text or label is applied directly to the package. The package along with instructions for use is placed in a cardboard box.
Storage conditions
Store at a temperature not exceeding 25 C in the original packaging. Keep out of the reach of children.
Best before date
2 years. Do not use after expiration date.
Voltaren
VOLTAREN® Representation: ATX code: M01AB05 Marketing authorization holder: NOVARTIS CONSUMER HEALTH, SA produced by DOJIN IYAKU-KAKO CO. LTD, packaging and packing FAMAR, SA diclofenac
Release form, composition and packaging
Transdermal patch 30 mg/, rectangular in shape with rounded edges, consisting of a beige polyester base with a uniformly applied adhesive layer from colorless to pale yellow with a faint aromatic odor, the adhesive surface is covered with a transparent protective film of polyethylene with two transverse cuts, one of which has a wavy line, a drawing is applied to the transparent protective film showing how to remove the film from the surface of the patch, the size of the patch is 100x140 mm.
1 patch diclofenac sodium 30 mg
Excipients: levomenthol - 45 mg, methylpyrrolidone - 120 mg, propylene glycol esters of fatty acids - 60 mg, citric acid - 12 mg, isoprene styrene copolymer - 1072.2 mg, polyisobutylene - 60 mg, esterified gum - 600 mg, mercaptobenzimidazole - 7.4 mg, butylated hydroxytoluene - 7.4 mg, liquid paraffin - up to 3000 mg, base made of polyester fibers (50 den) - 140 cm2, protective film made of polyester (thickness 75 microns) - 140 cm2.
2 - aluminum foil bags (1) with Zip-Lock fastener - cardboard packs. 5 - aluminum foil bags (1) with Zip-Lock fastener - cardboard packs. 7 - aluminum foil bags (1) with Zip-Lock fastener - cardboard packs. 10 - aluminum foil bags (1) with Zip-Lock fastener - cardboard packs.
Registration No.: •transdermal patch 30 mg/: 2, 5, 7 or 10 - LP-000978, 10/18/11. Active.
Pharmacological action of NSAIDs, a derivative of phenylacetic acid. It has a pronounced anti-inflammatory, analgesic and moderate antipyretic effect. The mechanism of action is associated with inhibition of the activity of COX, the main enzyme in the metabolism of arachidonic acid, which is a precursor of prostaglandins, which play a major role in the pathogenesis of inflammation, pain and fever. The analgesic effect is due to two mechanisms: peripheral (indirectly, through suppression of prostaglandin synthesis) and central (due to inhibition of prostaglandin synthesis in the central and peripheral nervous system). Inhibits proteoglycan synthesis in cartilage. For rheumatic diseases, it reduces pain in the joints at rest and during movement, as well as morning stiffness and swelling of the joints, and helps to increase range of motion. Reduces post-traumatic and postoperative pain, as well as inflammatory swelling. Suppresses platelet aggregation. With long-term use it has a desensitizing effect. When applied topically in ophthalmology, it reduces swelling and pain during inflammatory processes of non-infectious etiology.
Pharmacokinetics
After oral administration, it is absorbed from the gastrointestinal tract. Eating slows down the rate of absorption, but the degree of absorption does not change. About 50% of the active substance is metabolized during the “first pass” through the liver. When administered rectally, absorption occurs more slowly. The time to reach Cmax in plasma after oral administration is 2-4 hours depending on the dosage form used, after rectal administration - 1 hour, intramuscular administration - 20 minutes. The concentration of the active substance in plasma is linearly dependent on the dose applied. Does not accumulate. Plasma protein binding is 99.7% (mainly with albumin). Penetrates into synovial fluid, Cmax is reached 2-4 hours later than in plasma. It is extensively metabolized to form several metabolites, of which two are pharmacologically active, but to a lesser extent than diclofenac. Systemic clearance of the active substance is approximately 263 ml/min. T1/2 from plasma is 1-2 hours, from synovial fluid - 3-6 hours. Approximately 60% of the dose is excreted in the form of metabolites by the kidneys, less than 1% is excreted unchanged in the urine, the rest is excreted in the form of metabolites in bile.
Indications: Articular syndrome (rheumatoid arthritis, osteoarthritis, ankylosing spondylitis, gout), degenerative and chronic inflammatory diseases of the musculoskeletal system (osteochondrosis, osteoarthritis, periarthropathy), post-traumatic inflammation of soft tissues and the musculoskeletal system (sprains, bruises). Pain in the spine, neuralgia, myalgia, arthralgia, pain and inflammation after operations and injuries, pain with gout, migraine, algodismenorrhea, pain with adnexitis, proctitis, colic (bilious and renal), pain with infectious and inflammatory diseases of the ENT -organs For local use: inhibition of miosis during cataract surgery, prevention of cystoid macular edema associated with removal and implantation of the lens, inflammatory processes of the eye of a non-infectious nature, post-traumatic inflammatory process in penetrating and non-penetrating wounds of the eyeball.
Dosage regimen For oral administration for adults, a single dose is 25-50 mg 2-3 times. The frequency of administration depends on the dosage form used, the severity of the disease and is 1-3 times, rectally - 1 time. For the treatment of acute conditions or relief of exacerbation of a chronic process, it is used in /m at a dose of 75 mg. For children over 6 years of age and adolescents, the daily dose is 2 mg/kg. Externally applied in a dose of 2-4 g (depending on the area of the painful area) to the affected area 3-4 When used in ophthalmology, the frequency and duration of administration are determined individually. The maximum daily dose for adults when taken orally is 150 mg/day
Side effects From the digestive system: nausea, vomiting, anorexia, pain and discomfort in the epigastric region, flatulence, constipation, diarrhea, in some cases - erosive and ulcerative lesions, bleeding and perforation of the gastrointestinal tract, rarely - liver dysfunction. When administered rectally, in isolated cases, inflammation of the colon with bleeding and exacerbation of ulcerative colitis were observed. From the central nervous system and peripheral nervous system: dizziness, headache, agitation, insomnia, irritability, fatigue, rarely - paresthesia, visual impairment (blurredness, diplopia), tinnitus, sleep disorders, convulsions, irritability, tremor, mental disorders, depression. From the hematopoietic system: rarely - anemia, leukopenia, thrombocytopenia, agranulocytosis. From the urinary system: rarely - impaired renal function, swelling is possible in predisposed patients. Dermatological reactions: rarely - hair loss. Allergic reactions: skin rash, itching, when used in the form of eye drops - itching, redness, photosensitivity.
Local reactions: a burning sensation is possible at the site of intramuscular injection, in some cases - the formation of infiltrate, abscess, necrosis of adipose tissue; with rectal administration, local irritation, the appearance of mucous secretions mixed with blood, painful defecation are possible, with external use in rare cases - itching , redness, rash, burning; when applied topically in ophthalmology, a transient burning sensation and/or temporary blurred vision is possible immediately after instillation.
With prolonged external use and/or application to large surfaces of the body, systemic side effects are possible due to the resorptive effect of diclofenac.
Contraindications: Erosive and ulcerative lesions of the gastrointestinal tract in the acute phase, “aspirin triad”, hematopoietic disorders of unknown etiology, hypersensitivity to diclofenac and components of the dosage form used, or other NSAIDs. Use during pregnancy and lactation Use during pregnancy and lactation is possible in cases where the potential benefit to the mother outweighs the potential risk to the fetus or newborn. Use for liver dysfunction Use with extreme caution if you have a history of liver disease. Use for impaired renal function Use with extreme caution in patients with a history of kidney disease.
Use in elderly patients Use with extreme caution in elderly patients.
Use in children under 12 years of age Not recommended for use in children under 6 years of age.
Special instructions Use with extreme caution for diseases of the liver, kidneys, gastrointestinal tract in history, dyspeptic symptoms, bronchial asthma, arterial hypertension, heart failure, immediately after major surgical interventions, as well as in elderly patients. If there is a history of allergic reactions to NSAIDs and sulfites, diclofenac is used only in emergency cases. During treatment, systematic monitoring of liver and kidney function and peripheral blood patterns is necessary. Rectal use is not recommended in patients with diseases of the anorectal region or a history of anorectal bleeding. It should be used externally only on undamaged areas of the skin. Avoid contact of diclofenac with the eyes (except for eye drops) or mucous membranes. Patients using contact lenses should use eye drops no earlier than 5 minutes after removing the lenses. Not recommended for use in children under 6 years of age. During treatment with dosage forms for systemic use, alcohol consumption is not recommended. Effect on the ability to drive vehicles and operate machinery. During the treatment period, the speed of psychomotor reactions may decrease. If your vision becomes blurred after using eye drops, you should not drive a car or engage in other potentially hazardous activities.
Drug interactions When antihypertensive drugs are used simultaneously with diclofenac, their effect may be weakened. There are isolated reports of the occurrence of seizures in patients taking NSAIDs and quinolone antibacterial drugs simultaneously. When used simultaneously with GCS, the risk of side effects from the digestive system increases. With simultaneous use of diuretics, the diuretic effect may be reduced. When used simultaneously with potassium-sparing diuretics, it is possible to increase the concentration of potassium in the blood. When used simultaneously with other NSAIDs, the risk of side effects may increase. There are reports of the development of hypoglycemia or hyperglycemia in patients with diabetes mellitus who used diclofenac simultaneously with hypoglycemic drugs. When used simultaneously with acetylsalicylic acid, the concentration of diclofenac in the blood plasma may decrease. Although clinical studies have not established the effect of diclofenac on the action of anticoagulants, isolated cases of bleeding have been described with the simultaneous use of diclofenac and warfarin. With simultaneous use, it is possible to increase the concentration of digoxin, lithium and phenytoin in the blood plasma. The absorption of diclofenac from the gastrointestinal tract is reduced when used simultaneously with cholestyramine, and to a lesser extent with colestipol. With simultaneous use, it is possible to increase the concentration of methotrexate in the blood plasma and increase its toxicity. With simultaneous use, diclofenac may not affect the bioavailability of morphine, however, the concentration of the active metabolite of morphine may remain elevated in the presence of diclofenac, which increases the risk of developing side effects of the morphine metabolite, incl. respiratory depression. When used simultaneously with pentazocine, a case of the development of a grand mal seizure has been described; with rifampicin, a decrease in the concentration of diclofenac in the blood plasma is possible; with ceftriaxone, the excretion of ceftriaxone in bile increases; with cyclosporine, the nephrotoxicity of cyclosporine may increase.