Bone pain in cancer patients is usually caused by tumor cells that have invaded the bone, in other words, metastases. Bone pain is often the first sign of bone metastases, which is why it is necessary to verify or reject this assumption.
The treatment of such bone injuries itself is aimed at reducing pain, reducing the risk of fractures, and preventing or slowing down the development of other complications.
Cause
So, a very common cause of bone pain is metastatic cancer. That is, the doctor and the patient are no longer faced with primary, but with secondary oncology. Atypical cells of a primary disease of any organ can damage bone and cause pain.
Moreover, it is the bones that are most susceptible to metastasis of atypical cells into them, which often penetrate there with the bloodstream, attaching to the vascular wall of the network of capillaries located in the bone tissue.
Another way (this happens much less frequently) of penetration of atypical cells into the bone is ingrowth from a tumor localized in the immediate vicinity.
The cause of pain is the disruption of the normal functioning of bone cells by cancer cells. This changes the structure of bone tissue.
When a bone is healthy, it constantly undergoes the process of destruction of old tissue and the formation of new one. Once in the bone, atypical cells disrupt this balance. The attacked periosteum (bone membrane) and nerves react to the invasion, causing pain.
Non-pathological causes of joint pain
Arthromyalgia can be non-pathological in nature. They often occur against the background of routine effects on the body and the musculoskeletal system:
- Excessive physical activity. Workouts of various types can cause muscle hypertonicity, which causes the latter to become denser and begin to adhere more tightly to the joints. As a result, the articular surfaces are compressed and the nutrition in them is disrupted, which provokes the autonomous development of a spontaneous pain symptom. Thus, pain in the joints occurs due to metabolic disorders, and in the muscles due to increased tone and soreness.
- Poor nutrition. The activity of the entire body depends on nutrition, and the musculoskeletal system is no exception. If the body does not receive enough of certain substances and microelements, conductivity in muscle structures is disrupted and regeneration processes are inhibited. Against the backdrop of all this, pain appears. In addition, with poor nutrition, patients often experience dysfunction of the visceral organs, which worsens the condition of the skin and its derivatives.
- Meteor dependence. For many people (most often older people), pain appears due to changing weather conditions. The painful sensations are twisting and aching in nature.
- Menstrual period. During menstruation, some women experience arthromyalgia. This is due to the degree of pain threshold and the intensity of the hormonal surge.
- Childhood and adolescence. Patients of this age group experience pain quite often and there is nothing strange about it. Their occurrence is explained by the process of skeletal growth and active division in bone tissue. In many children, bones grow very quickly and the muscles cannot keep up with them, which is why pain appears.
- Pregnancy. The main cause of pain is again hormonal changes. If a woman is already in later stages, when the fetus has reached a noticeable size, pain in the muscles and joints appears due to overload. A woman carries additional weight on herself every day, as a result of which the same soreness occurs.
- Injuries. This can be either microtrauma or more extensive damage. Bursa rupture, sprains, bruises and other injuries always lead to disruption of blood supply to the joints and muscles, which is why they begin to hurt. The intensity of pain depends on the degree of tissue damage.
Pain in joints and muscles caused by such factors can resolve on its own. It is enough to reduce the intensity of training, revise your diet, heal injuries or wait out some specific periods and the pain will go away by itself.
Diagnosis of metastases
As a rule, bone metastases are found in the central region of the skeleton, but, of course, they can damage absolutely any bone.
To detect bone metastases, fluoroscopy or a bone scan is performed. This helps to understand what caused the pain syndrome.
During the scan, the patient is injected intravenously with a special radioactive substance that circulates throughout the body and enters the bones. If the substance is too concentrated in a certain location, this indicates the presence of atypical cells.
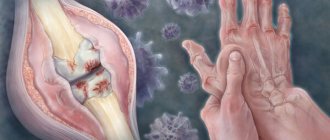
Of course, pain can be caused by other pathologies, for example, arthritis. The thing is that if the pain is caused by an oncological process, it has one quality - permanence. Bone pain that lasts a week or two is a good reason to visit a doctor.
TREATMENT METHODS FOR BONE ONCOLOGY
Treatment is aimed at relieving pain, treating fractures, and preventing possible complications.
There are different types of treatment for bone cancer depending on the type and extent of its spread in the body.
These include:
- Surgery: In case of surgery, the cancerous tumor is removed from the bone. If possible, the doctor will repair the bone after surgery, but there are cases in which the doctor will be forced to amputate part of the bone.
- Chemotherapy: A cancer treatment that uses drugs to kill harmful cells and tissue.
- Radiotherapy: A method that uses radiation to kill cancer cells.
- Mifamurtide: a medicine used to treat osteosarcoma, a special type of bone cancer. It stimulates the immune system to attack cancer cells.
Clinical manifestations
Once it occurs, the pain syndrome provoked by metastases is moderate in nature. It intensifies after physical activity or at night.
As the tumor process develops, the symptoms also intensify. The pain syndrome becomes pronounced and painful.
There are other “signals” indicating the presence of bone metastases:
- Spinal cord compression. It happens quite rarely, but it makes life quite difficult. The thoracic spine or the lumbar and cervical sections are subject to compression.
- Hypercalcemia. The level of calcium in the blood increases, which ultimately leads to a malfunction of many body systems. The complication is very common.
- Pathological fractures. The femur in the area of the diaphysis or neck often suffers.
Patients with late stages of cancer also exhibit symptoms such as:
- Temperature increase;
- Exhaustion;
- Weakness, etc.
Elderly patient with pain in bones, joints and muscles
Figure 1 shows the main causes of pain, which is based on pathological processes in various structures of the joint-musculoskeletal system in elderly and senile patients. Bone pain. The decrease in bone mass and loss of bone density that occurs with age underlie the development of osteopenia and osteoporosis. with the occurrence of bone fractures. The most common locations of fractures are the spine, femoral neck and radius. One of the causes of spinal pain in the elderly is compression fractures of the spine, which patients do not always associate with trauma, and doctors often interpret as a manifestation of osteochondrosis and spondylosis. In this regard, these fractures are detected either by chance or during an X-ray examination of the spine due to severe pain that does not fit into the picture of degenerative lesions of the spine. Not all bone fractures are due to osteoporosis. The latter must be differentiated from such pathological processes as primary and metastatic tumors, osteomalacia, Paget's disease, peripheral neuropathy. Osteomalacia is characterized by impaired mineralization of the bone matrix associated with a deficiency of vitamin D (impaired consumption, synthesis, metabolism) and phosphate (impaired transport, intake of phosphate-binding antacids such as Almagel). Osteomalacia should be suspected if there is a decrease in the level of calcium in the blood and urine, phosphate in the serum, or an increase in the activity of alkaline phosphatase and parathyroid hormone. Osteoporosis with or without pathological vertebral fractures can be observed in multiple myeloma, which should be suspected in the presence of anemia, an increase in ESR, as well as changes in urine in the form of proteinuria. The diagnosis is confirmed by bone marrow examination (presence of myeloma cells over 20%) and detection of monoclonal protein in the blood or urine by serum or urine protein electrophoresis. Paget's disease (osteitis deformans) is characterized by local lesions of the skeleton and is caused by impaired remodeling of the bone tissue. In this case, increased resorption by osteoclasts and a compensatory increased formation of new bone tissue occur. The processes of resorption and neoplasm lead to disruption of the architectonics of bone tissue. The main clinical manifestations of Paget's disease are the following: • pain in the affected bones; • bone deformities (lower limbs, spine); • secondary osteoarthritis; • fractures; • neurological disorders (compression neuropathies, deafness, dizziness); • radiological signs (restructuring of the bone pattern, deformations, thickening of the affected parts of the bones); • increased activity of alkaline phosphatase in the blood. One of the causes of pain in bones and joints in old people may be the infectious nature of bone lesions (in particular, tuberculosis and osteomyelitis). Tuberculosis is most often localized in the vertebrae and is, as a rule, the result of dissemination of tuberculosis infection from old foci, often the lungs. Osteomyelitis is hematogenous in nature, often accompanied by fever, changes in the blood (anemia, neutrophilic leukocytosis). Suspicion of osteomyelitis may be based on anamnestic indications of traumatic episodes preceding the development of clinical symptoms. X-rays do not always reveal bone lesions. Bone scanning using radioisotopes can provide diagnostic assistance. Figure 2 shows a diagnostic algorithm for bone pain. Joint pain. Joint pain in the elderly and elderly have different origins and are associated with inflammatory, degenerative and metabolic disorders in various structures of the articular apparatus. The most common joint pathology in this age group is osteoarthritis, which occurs in 60–70% of patients over 65 years of age (more often in women) and is characterized by a chronic progressive course, pain syndrome with the gradual development of functional disorders of the joints. Criteria for osteoarthritis of the knee joints: • mechanical pain; • pain on palpation; • crepitation; • osteophytes; • radiological signs (narrowing of the joint space, subchondral sclerosis, osteophytosis); • limitation of mobility. Criteria for osteoarthritis of the hip joints: • pain when moving; • narrowing of the joint space, osteophytes. Most often it is necessary to make a differential diagnosis between osteoarthritis and rheumatoid arthritis (Table 1, Fig. 3). Muscle pain The sensation of muscle pain is observed in various diseases, syndromes and pathological conditions. Myalgia can be a manifestation of both rheumatic diseases themselves (polymyositis, rheumatoid arthritis, etc.) and diseases of another origin (infections, traumatic lesions, tumors). The most typical pathology in elderly and senile patients, manifested by sensations of muscle pain, is polymyalgia rheumatica. The disease belongs to systemic vasculitis with predominant damage to periarticular tissues (capsule, ligamentous apparatus, tendons). There is no actual muscle damage in polymyalgia rheumatica, despite this designation of the disease. The main criteria for polymyalgia rheumatica are the following: • pain in the proximal parts of the shoulder and pelvic girdle; • fever not inferior to antibiotics; • significant increase in ESR; • pronounced and rapid effect of small doses of glucocorticoids. The presence of the above clinical and laboratory signs in an elderly patient requires, first of all, the exclusion of the paraneoplastic nature of the symptoms, for which an oncological search is carried out to exclude a tumor process. Polymyalgia rheumatica can be combined with temporal arteritis (Horton's disease), which should be suspected in patients with complaints of severe, sometimes unbearable headaches that are poorly controlled by analgesics, swelling and severe pain in the temporal region, blurred vision, as well as an unexplained significant increase in ESR. Below are the main differential diagnostic signs of polymyalgia rheumatica and primary fibromyalgia, although the latter occurs much less frequently in old age and is essentially one of the somatoform manifestations of depression (Table 2). Figure 4 shows the diagnostic algorithm for muscle pain. Side effects and safety of NSAID therapy The effectiveness and tolerability of NSAIDs is determined by the effect of drugs on the synthesis of prostaglandins. There are two isoforms of cyclooxygenase (COX) – COX-1 and COX-2. COX-1 regulates the synthesis of prostaglandins, which ensure the physiological activity of gastric mucus, platelets, and renal epithelium. COX-2 is involved in the production of prostaglandins in the area of inflammation. It is believed that the anti-inflammatory and analgesic effects of NSAIDs are determined by the inhibition of COX-1, while the most common side effects are due to the inhibition of COX-2. Numerous clinical studies have shown that the effectiveness of non-selective and selective COX-2 inhibitors is approximately the same, while side effects occur less frequently with the use of selective COX-2 inhibitors. Risk factors for side effects associated with the use of NSAIDs include the following: • Arterial hypertension • Heart failure • History of peptic ulcer disease • Bronchial asthma • Liver failure • Nephropathy • Thrombocytopathies • Concomitant use of certain medications (glucocorticoids, anticoagulants, acetylsalicylic acid) • Taking high doses NSAIDs • H. pylori infection. Elderly and senile patients are the most vulnerable group with regard to the development of side effects during treatment with NSAIDs. The range of drug complications is quite wide and includes damage to the gastrointestinal tract, cardiovascular system, kidneys, central nervous system, hematopoietic tissue, and hypersensitivity reactions. The main target of adverse reactions when using NSAIDs is the gastrointestinal tract, which is due to both local and systemic inhibition of prostaglandin synthesis. In this case, damage to the esophagus (esophagitis), superficial erosions and peptic ulcers of the stomach (usually prepyloric and antral), damage to the mucous membranes of the small and large intestines, and hepatotoxicity are noted. The most common and prognostically unfavorable complication when prescribing NSAIDs in the elderly is erosive and ulcerative processes in the stomach (NSAID-gastropathy) with the development of bleeding and perforation. A feature of the above medicinal pathology is the erased clinical symptoms or the absence thereof, which is generally typical for elderly and senile patients. Attention should be paid to the negative dynamics of hemoglobin levels in the form of the appearance of hypochromic anemia along with a decrease in serum iron levels, which in patients receiving NSAIDs should be regarded as a consequence of hidden chronic blood loss from erosions or gastric ulcers. Often the first manifestation of NSAID gastropathy is the development of life-threatening complications (bleeding, perforation). Elderly patients constitute a special group at high risk of developing gastric bleeding during treatment with NSAIDs. Additional risk factors for gastric bleeding when using NSAIDs in the elderly may be a history of peptic ulcer disease, taking small doses of acetylsalicylic acid for secondary prevention of coronary artery disease, the use of indirect anticoagulants, treatment with glucocorticoids (bronchial asthma, rheumatoid arthritis, etc.). Different NSAIDs have varying toxicity to the gastrointestinal tract. At the same time, the most powerful COX-1 inhibitors, such as indomethacin and piroxicam, more often cause side effects compared to drugs with more balanced activity (Voltaren, ibuprofen, ketoprofen). Among the side effects during treatment with NSAIDs, the most prognostically dangerous are gastric bleeding, and the risk of bleeding is different for each of the following NSAIDs used [Garcia-Rodriguez LA, 1998]. Ibuprofen 2.1 Diclofenac 2.7 Ketoprofen 3.2 Naproxen 4.3 Nimesulide 4.4 Indomethacin 5.5 Piroxicam 9.5 Ketorolac trimethamine 24.7 Ketoprofen has relative safety, somewhat inferior to Voltaren and ibuprofen. According to a multicenter study of the effectiveness and safety of the use of ketoprofen in elderly patients with osteoarthritis for 12 months, the incidence of gastrointestinal tract damage was lower than during treatment with other non-selective NSAIDs (1.7 and 4%, respectively), and none of the patients had Severe adverse reactions and deaths have been reported [3,4]. Significantly reduce the incidence of such dangerous complications as bleeding and perforation, mainly selective COX-2 inhibitors (meloxicam, nimesulide), as well as specific COX-2 inhibitors (celecoxib), which makes it possible to increase the safety of treatment and consider them the drugs of choice in elderly patients with factors high risk of complications. It should be noted, however, that despite the relative safety of selective COX-2 inhibitors, severe complications have also been described with their use [5]. For the prevention of NSAID gastropathy in elderly patients with a high risk of their development, along with the preference for the choice of combined NSAIDs (diclofenac + misoprostol) and selective COX-2 inhibitors, it is recommended to prescribe the proton pump inhibitor omeprazole. It has been shown that omeprazole significantly reduces the incidence of ulceration in the stomach and duodenum compared to placebo and ranitidine. At the same time, H2-histamine receptor blockers are effective for the prevention of duodenal ulcers only. Taking into account the likelihood of the risk of developing erosive and ulcerative processes in the stomach in patients with a high risk of NSAID gastropathy while taking selective COX-2 inhibitors, the prevention of complications in the form of prescribing proton pump inhibitors and misoprostol is also justified. Parenteral (intramuscular) use of NSAIDs does not reduce the risk of damage to the gastrointestinal tract, since this creates a high concentration of the drug in the blood serum, which is accompanied by a systemic effect on the body. At the same time, local use of NSAIDs in the form of ointments, creams, and gels ensures maximum concentration at the sites of their application without entering the systemic bloodstream. In this regard, the risk of side effects with local use of NSAIDs is minimized. Among the cardiovascular complications in the treatment of NSAIDs, the most relevant for elderly patients is an increase in blood pressure (especially in the presence of arterial hypertension), as well as a decrease in the effectiveness of some antihypertensive drugs. Taking into account the above, the optimal drug should be considered to be one that, while maintaining analgesic activity, had a lesser effect on blood pressure levels. For patients with osteoarthritis with concomitant arterial hypertension, it may be preferable to prescribe ketoprofen, which, unlike other NSAIDs (diclofenac, piroxicam, indomethacin), causes an increase in blood pressure less frequently and to a lesser extent, and also does not reduce the effect of antihypertensive drugs [6]. In the treatment of elderly and senile patients with selective and non-selective NSAIDs, most of whom suffer from concomitant cardiovascular pathology (coronary artery disease, arterial hypertension, diabetes mellitus) and receive acetylsalicylic acid (ASA) for preventive purposes, the problem of possible inhibition and antiplatelet effect of acetylsalicylic acid has emerged. . To the greatest extent, such “cancellation” of the antiplatelet effect is characteristic of indomethacin and ibuprofen, while diclofenac and ketoprofen can be used in patients with risk factors for thrombosis due to their lack of an inhibitory effect on the ASA-dependent antiplatelet effect. Along with an increase in blood pressure during the use of NSAIDs, signs of heart failure may appear or intensify due to fluid retention, which is less pronounced when using selective COX-2 inhibitors. Equally important is the prevention of the development of nephropathies with long-term use of NSAIDs or other analgesics such as acetylsalicylic acid, and the risk of nephropathy in the elderly is much higher. A decrease in glomerular filtration can be caused by both non-selective and selective NSAIDs. Increased blood pressure and functional impairment of the kidneys, up to the development of chronic renal failure, while taking NSAIDs may be especially unfavorable for patients with gout, who already have a high incidence of arterial hypertension and nephropathy. Drug interactions of NSAIDs When prescribing drugs with analgesic activity (and especially NSAIDs), the possibility of their interaction with other drugs prescribed to patients for concomitant diseases should be taken into account. Due to polymorbidity in the elderly and often forced polypharmacy, the risk of drug interactions in this category of patients is much higher, which requires consideration and careful monitoring during the treatment process. NSAIDs from the group of non-selective COX-1 inhibitors may weaken the effect of some antihypertensive drugs (in particular, ACE inhibitors and b-blockers). Medications with which NSAIDs may interact include digoxin, thiazide diuretics, indirect anticoagulants, and anticonvulsants (Table 3). Ensuring effective and safe NSAID therapy in the elderly • Assess the state of the gastrointestinal tract, cardiovascular system, and kidneys before prescribing. • Prescribing selective COX-2 inhibitors, combined NSAIDs, a combination of NSAIDs with proton pump inhibitors (omeprazole) to patients with risk factors. • Avoid prescribing non-selective NSAIDs for renal failure. • Careful monitoring of treatment (serum creatinine, gastroscopy, hemoglobin level, liver transaminase activity). • Ensuring patient compliance (training, creating motivation for treatment, informing about possible side effects, cooperation with the doctor, etc.).
Literature 1. Nasonova V.A. Geriatric problems of non-steroidal anti-inflammatory therapy. Clinical Gerontology, 1998, 2, 39–42. 2. Shekshina E.V., Balabanova R.M. Combined analgesics in the symptomatic treatment of pain in rheumatology. RMJ, 2004, 6, 422–424. 3. Nasonov E.L., Chichasova N.V., Shmidt E.I. Prospects for the use of non-selective non-steroidal anti-inflammatory drugs (using the example of ketoprofen) as selective COX-2 inhibitors in clinical practice. RMJ, 2002, 22, 1014–1017. 4. Schattenkircher M. Long-term safety of ketoprofen in an elderly population of arthritis patients. Scand.J.Rheumatol.1991,91(Suppl.), 27–36. 5. Simon LS, Smolen GS, Abramson SB et al. Controversies in COX–2 selective inhibition. J Rheumatology 2002, 29, 1501–1510. 6. Marusenko I.M., Vezikova N.N., Ignatiev V.K. Advantages of ketonal in the treatment of elderly patients with osteoarthritis and concomitant arterial hypertension. RMJ 2004, 6, 415–417. 7. Nasonov E.L., Nasonova V.A. Pharmacotherapy of pain: the view of a rheumatologist. Consilium 2001.
Primary tumors
Primary occurrence of bone cancer is rare. Among such diseases are sarcomas. The primary lesion can be caused by active growth of bone tissue, this occurs in people under the age of twenty.
Symptoms of the primary disease:
- Pain in the focal area. At first, the pain syndrome is mild or moderate. He may disappear, but then appears again. At later stages it is constant and pronounced.
- General symptoms that are characteristic of any cancer disease, for example, weight loss, weakness, etc.
- Manifestations characteristic of bone damage - lameness, pathological fractures, etc.
Primary and secondary diseases are united by a number of manifestations, which is why in making a diagnosis you should not rely only on the patient’s complaints. Diagnostics required.
Measures to strengthen bones
To prevent bone and joint diseases, it is important to follow 3 basic principles. These include a healthy diet, moderate physical activity and regular examination by a doctor. To maintain musculoskeletal health, it is important to consume plenty of calcium. It is found in fish, cheese, cabbage, and sesame seeds. It is also important to maintain a balance of vitamins .
Vitamins A, B, D and E will be especially beneficial for bones. When there is a deficiency, you can take vitamin complexes (Aevit).
What other preventive measures will help maintain bone health:
- regular jogging and exercise on an exercise bike;
- walking in the fresh air;
- eating more greens, vegetables and fruits;
- performing a warm-up during prolonged sedentary work;
- quitting smoking, alcohol and energy drinks.
Daily exercise, a healthy diet, a good mood and careful attention to your well-being are the key to healthy bones, joints and muscles that withstand high loads every day. It is important to consult a doctor promptly when unpleasant symptoms begin to bother you.
Painkillers
In almost ninety percent of cases, pain can be significantly reduced with painkillers. But often this is not enough, because as the tumor develops it can become insensitive to them. The question of choosing a drug remains relevant.
There are WHO recommendations regarding the reduction of pain caused by cancer. In these recommendations, the choice of drug should be based on the intensity of the patient's pain. This intensity is graded on a special scale.
- Points 1-3 are given to pain syndrome of mild and moderate severity. Drugs – non-opioids, for example, paracetamol;
- Points 4-6 – moderate pain syndrome. Drugs – opioids (analgesic drugs containing narcotic substances);
- Points 7-10 – the pain syndrome is severe. The drugs are strong opioids. In some cases, drugs that enhance pain relief.
Speaking about painkillers, one cannot fail to note the side effects associated with them, including:
- Feeling drowsy;
- Stool imbalance;
- Dizziness, etc.
And once again about what we noted above: it is better to start using painkillers when the pain syndrome just begins to manifest itself.