Golden autumn is a great time to enjoy the last warm days. But, unfortunately, the transition from summer heat to autumn cold and rain is not always gradual. And if weather conditions change very sharply, then in terms of well-being for many people this does not go unnoticed.
In autumn, many diseases worsen: from asthma and peptic ulcers to rheumatism. Seasonal pain affects people of different ages and with different health conditions. But most often in the fall they complain of joint pain. Why does this happen and how do we explain seasonal ailments?
Primary joint pain:
Arthritis
The most common joint disease. Arthritis develops against the background of advanced trauma, infectious and autoimmune diseases. There are two subgroups of arthritis: acute and chronic. In acute arthritis, pain in the joints is sharp, accompanied by severe swelling, redness and increased temperature of the joint. In chronic cases, the joint constantly aches, but there is no severe swelling or redness. The patient quickly gets used to it and stops paying attention to the pain until the joint completely collapses. With arthritis, the joints often hurt constantly, and over time, problems with flexion and extension appear.
Arthrosis
Wear and destruction of joint cartilage. With arthrosis, cartilage loses its elasticity, becomes thinner, and metabolism in the cartilage tissue is disrupted. Most often it affects the knee joints. Arthrosis is characterized by aching pain, weaker after sleep and intensifying during the day. The intensity of the pain increases with tension in the leg and pressure on the joint. With advanced arthrosis, the pain does not subside even after rest. Other symptoms of arthrosis are clicking and crunching sounds in the joint.
Bursitis
Inflammation of the mucous membranes of the joints most often occurs as a complication of injuries. Bursitis is characterized by painful swelling due to abnormal enlargement of the joint sac. The pain varies depending on the stage of development of the disease, it can be aching, severe, shooting and throbbing, and can radiate beyond the joint. Often worsens at night.
The problem of pain in osteoarthritis
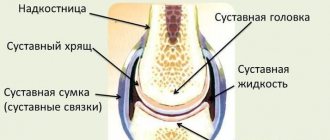
Osteoarthritis deformans is a disease that affects a significant portion of the population. About 80% of all patients with joint diseases are patients with osteoarthritis [1]. The twentieth century was marked by many technical innovations that greatly changed people's lives. On the one hand, the ease of physical labor has reduced the load on human joints, but on the other hand, it was the emergence of many technical devices that led to an increase in the number of cases of arthrosis in people of certain professions: drillers, miners, people working on vibration installations, etc. Development transportation has led to a decrease in physical activity of a significant part of the population, an increase in material well-being has led to an increase in body weight in more than half of the world's population. For many years, it was believed that osteoarthritis was a consequence of age-related “wear and tear” of cartilage. However, the pathogenesis of the disease is much more complex (Fig. 1). As shown in Figure 1, there are a very large number of factors influencing the development and progression of the main links in pathogenesis: cartilage destruction, synovial inflammation, subchondral bone rigidity. Osteoarthritis occurs as a result of the interaction of mechanical and biological factors. This process occurs either due to changes in cartilage or subchondral bone, or as a result of disease within these tissues themselves (for example, gene defects of type 11 collagen, ochronosis), or as a result of exposure to external abnormal mechanical stress (joint instability, increased load, injuries). As the disease progresses, changes in cartilage in osteoarthritis become more pronounced (Fig. 2).
| Figure 2. Progression of cartilage destruction |
The main clinical manifestations of osteoarthritis are pain and gradual loss of function. According to the modern classification, the nature of pain is determined depending on the main pathogenetic mechanism: nociceptive, neuropathic, functional (or dysfunctional).
In osteoarthritis, the main mechanism of pain development is nociceptive, although patients may also experience neuropathic pain, which should be taken into account when developing therapeutic tactics. It is the pain syndrome that becomes a factor that limits the activity of patients and leads to the formation of “painful behavior” (Fig. 3). Although the pain syndrome in osteoarthritis, especially at the onset of the disease, is not as severe as in chronic inflammatory arthrological diseases, the doctor’s efforts should be aimed at maximizing the suppression of chronic pain. Chronic pain syndrome is a significant medical problem. The development of pain leads to functional disorders of the cardiovascular system, respiratory system, digestion, etc. [2]. According to a telephone survey of 46,394 respondents from 16 European countries (Fig. 4), 19% of people suffer from severe chronic pain [3] with an intensity of at least 5 points on a 10-point visual analogue scale (VAS). And the most common cause of chronic pain is osteoarthritis (Fig. 5). It is known that the development of the disease in women leads to a decrease in life expectancy by an average of 10–15 years [4]. However, it has been shown that a decrease in life expectancy in older people depends to a greater extent on the intensity of pain (Fig. 6) than on the presence or absence of life-threatening diseases (for example, coronary artery disease, arterial hypertension, etc.) [5]. When assessing the survival of 1525 patients, of whom 370 suffered from osteoarthritis (24%), 246 from cardiovascular diseases (16%), and 109 had a combination of osteoarthritis and cardiovascular diseases, it turned out that the relative risk (95% CI) of death for The 5-year period among patients with osteoarthritis who had pain intensity > 40 mm, compared with those who had pain intensity < 40 mm, was 4.2, with no differences in age and gender [5].
Thus, the problem of pain in osteoarthritis is not only medical, but also social in nature and affects the functional ability of patients, their social activity and life expectancy.
The variety of pathogenetic mechanisms involved in the formation and progression of osteoarthritis also leads to the development of pain syndromes of different origins. Pain in this case can be due to various reasons. The main mechanism leading to the development of pain syndrome is considered to be gradual degradation and reduction in the synthesis of the cartilage matrix, loss of its shock-absorbing properties, imbalance of bone metabolism in the underlying bone with the development of osteophytes (Fig. 7). Mechanical pressure on the exposed bone leads to pain during physical activity, even small ones. In addition, with osteoarthritis, inflammation develops in the synovium (secondary synovitis), which leads to morning stiffness and inflammatory pain. Secondary synovitis is an almost obligatory sign of the disease and the most common cause of pain. Although it is believed that synovitis in osteoarthritis is secondary to cartilage degradation, the pathogenetic site of inflammation is not fully understood. An inflammatory component may be present (at least in some patients) during certain phases of advanced disease. For example, there may be clear synovial hyperplasia and mononuclear cell infiltration, a pattern indistinguishable from rheumatoid arthritis. This inflammation is local, most pronounced at the junction of the synovium and cartilage. But synovitis also influences cartilage loss through the production of inflammatory cytokines such as interleukin-1 (IL-1), which in turn causes the release of matrix metalloproteinases such as collagenases and stromelysin, prostaglandins and plasminogen activators. It is known that in dogs, intra-articular administration of IL-1 receptor antagonists reduces the expression of collagenase and inhibits the subsequent development of the disease.
Pain in osteoarthritis may be caused by increased intramedullary pressure in the subchondral bone. Changes in subchondral bone visible on radiographs in patients with established disease suggest an important role in the development of this disease rather than being considered a consequence of cartilage damage. It is known, for example, that the integrity of cartilage depends on the mechanical properties of the underlying bone. Thus, changes in the subchondral bone (possibly after repeated microfractures) cause a lack of pressure absorption. The role of subchondral bone turnover in osteoarthritis has been supported by various methods. In vivo studies in guinea pig models showed distinct measurements in subchondral bone before the development of cartilage pathology. In prospective studies, scintigraphic bone changes preceded radiographic progression in the knee and hand joints, which was accompanied by increased bone expression of matrix metalloproteinases and alkaline phosphatase in human coxarthrosis.
The association of pain with a certain type of movement indicates damage to the tissues surrounding the joint, for example, due to spasm of the periarticular muscles or due to fibrosis of the joint capsule in osteoarthritis. Mostly night pain in the area of large joints or in the entire limb is most often caused by either vascular disorders (venous hyperemia) or neuropathies (tunnel, radicular syndromes). Sudden sharp pain when walking with the rapid development of synovitis (joint block) can occur with osteoarthritis due to the sudden penetration of an osteophyte into the soft tissue or when a fragment of osteophyte or cartilage enters the joint cavity.
It should be noted that in osteoarthritis there is no correlation between the radiological stage and the clinical manifestations of the disease, the leading among which is pain: radiological manifestations of osteoarthritis are observed in approximately 30% of the adult population, and pain develops in 10–12% [6].
Currently, it is believed that osteoarthritis affects all the structures that make up the joint, as well as the periarticular tissues. This means that treating the disease is a difficult, complex task that requires the combined efforts of doctors from various specialties: rheumatologists, orthopedists, neurologists, and surgeons. The social significance of this pathology is reflected in Table 1.
Treatment of articular damage in deforming osteoarthritis has its own characteristics, which is associated with the variety of causes that cause pain in the joint or in its area with this disease, as well as with the elderly age of patients, often suffering from concomitant cardiovascular, gastroenterological, endocrinological and other diseases. The main areas of treatment for osteoarthritis are the following.
- Suppression of inflammatory factors: secretion of proinflammatory cytokines; increased secretion of prostaglandin E2 (PGE2); increased activity of synovial enzymes.
- Suppression of destructive factors: synthesis of metalloproteinases, degradation of collagen fibers, proteolytic activity; increased synthesis of glycosaminoglycans (GAGs).
- Suppression of subchondral bone rigidity.
- Improving lubrication (lubrication) of the joint, since with osteoarthritis, the viscosity and elasticity of the synovial fluid decreases, not only playing the role of “lubricant”, but also providing nutrition to the cartilage, since cartilage does not have blood vessels.
For a long time, treatment of osteoarthritis was limited to the use of painkillers and anti-inflammatory drugs. The use of drugs from other groups, possibly influencing the pathogenesis of the disease, was limited by the lack of convincing evidence of their effectiveness. Expansion and deepening of ideas about the nature of the disease and the subtle mechanisms of its development have led to a revision of the point of application and assessment of the pathogenetic significance of most drugs used in the treatment of osteoarthritis. Currently, there is a wide range of anti-arthrosis drugs, the classification of which is presented in Table 2.
Considering that in osteoarthritis pain is most often caused by the development of synovitis, nonsteroidal anti-inflammatory drugs (NSAIDs) are most often used for this disease. Treatment of secondary synovitis in osteoarthritis places certain demands on NSAIDs - good tolerability and the ability to combine them with other drugs. It is known that long-term use of non-selective NSAIDs is associated with the risk of developing serious side effects - gastropathy, nephropathy, worsening arterial hypertension and cardiovascular failure, especially in elderly patients [7, 8]. In addition, when using NSAIDs, there is an undesirable interaction with a number of drugs (anticoagulants, antiepileptics, antihypertensive drugs, cardiac glycosides (digoxin), diuretics) often used in the treatment of concomitant pathologies. The emergence in recent years of NSAIDs, which predominantly or selectively suppress the synthesis of cyclooxygenase (COX) type 2, can improve the safety of treatment for this group of patients [9]. If long-term use is necessary, as well as in persons with a history of ulcerative-erosive lesions of the gastrointestinal tract, prescribe movalis (7.5–15 mg/day) [10], nimesulide (100–200 mg/day) or Celebrex (100–200 mg/day) provides sufficient analgesic and anti-inflammatory effect with minimal risk of adverse reactions.
The advent of the injectable form of meloxicam for intramuscular administration provided significant advantages to using the drug in terms of rapid development of the effect (the onset of therapeutic action within 30 minutes after administration), as well as the possibility of using the method of “step therapy”: administration of movalis in the first 3–6 days in /m for quick relief of exacerbation, then continuing therapy with the same drug in the same dose (15 mg), but in tablet form.
The presence of a new form of nimesulide in the form of a granulate makes it possible to increase the effectiveness of the drug due to better bioavailability of this form and achieving a higher concentration of this drug in the blood serum compared to the tablet form. Considering the fact that COX-2 is practically absent in the interstitial tissue of the kidneys, located mainly in the renal tubules, specific COX-2 inhibitors (meloxicam, celecoxib) can be used in the initial and moderate stages of renal failure without reducing the daily dose.
Non-COX-selective NSAIDs aggravate the severity of osteoarthritis with long-term use, so they should be used in low doses and in short courses. It has been shown that in osteoarthritis, cartilage is most negatively affected by indoleacetic acid derivatives (indomethacin) (Fig. 8), although propionic acid derivatives (ibuprofen, naproxen, etc.) also accelerate the progression of the disease by ~30%, according to radiography. [eleven]. All non-selective NSAIDs reduce the synthesis of GAGs necessary for cartilage regeneration (Fig. 9). In addition to the fact that selective COX-2 inhibitors (meloxicam, nimesulide, celecoxib) are better tolerated by elderly patients with osteoarthritis due to a real reduction in the incidence of side effects from the gastrointestinal tract, kidneys, and liver [10], they do not affect the synthesis of GAGs (Fig. 10), and by suppressing COX-2, they can have a positive effect on bone tissue remodeling, since activation of osteoclasts occurs with the active participation of COX-2.
If the mechanical type of joint pain predominates in destructive osteoarthritis, analgesics such as paracetamol (500–2000 mg/day) or tramadol (50–150 mg/day) should be used. Night pain associated with vascular disorders is well relieved with the use of Trental and peripheral vasodilators. Treatment of neuropathic pain is carried out using vitamin therapy. Local therapy with diprospan is widely used to relieve tunnel syndromes, paravertebral and neural blockades of diprospan with novocaine are used for radicular syndromes and lesions of large nerve trunks.
Slow-acting structure-modifying drugs used in the treatment of osteoarthritis are cartilage matrix components derived from animal cartilage or synthetically produced. Having a complex mechanism of action and tropism for cartilage, chondroitin sulfate and glucosamine sulfate are integrated into the structures of cartilage tissue, stimulating its synthesis and inhibiting destruction [15]. The main criterion for the effectiveness of slow-acting drugs is the reduction of pain and the need for NSAIDs, as well as the improvement of the patient’s functional abilities [16]. The most studied drugs used in the treatment of osteoarthritis are chondroitin sulfate and glucosamine - natural components of cartilage. Chondroitin sulfate is a high molecular weight polysaccharide from the group of proteoglycans and is an integral part of the aggrecan molecule of cartilage. Glucosamine is a substrate for the synthesis of proteoglycans and is produced during the hydrolysis and deacetylation of crustacean chitin. Medicines registered in Russia include two glucosamine salts - hydrochloride (artra, teraflex) and sulfate (dona, chondro).
Both chondroitin sulfate and glucosamine have their own analgesic and anti-inflammatory effects, which are realized not by suppressing the synthesis of prostaglandins, but by suppressing the activity of lysosomal enzymes and inhibiting superoxide radicals. Their positive effect on cartilage is due to the suppression of catabolic processes and stimulation of anabolic processes in cartilage. It should be noted that the final positive effect of these drugs on the course of osteoarthritis is very difficult to assess. For the drugs structum and don, long-term controlled studies showed a slowdown in the radiographic progression of the disease, which was assessed by the rate of narrowing of the joint space of the knee joint [17, 18, 19]. Structural-modifying properties and improvement of clinical symptoms of osteoarthritis of the hip joints are detected with the use of piascledine 300 [20], and of the knee joints with diacerin (an IL-1 inhibitor), which is being prepared for registration in the Russian Federation. It is interesting that in the studies of Reginster [17] and Pavelka [18], which showed a significantly lower rate of narrowing of the joint space during three years of treatment of gonarthrosis with the drug Dona, there was no correlation between pain reduction and a slowdown in the progression of osteoarthritis. Therefore, the main criterion for the effectiveness of slow-acting drugs for osteoarthritis remains the reduction of pain and, accordingly, the need for painkillers, as well as the improvement of the patient’s functional ability. An important aspect of the action of chondroprotectors is the preservation of the positive effect after completion of the full course of treatment, while after the withdrawal of fast-acting drugs, pain and a decrease in the patient’s functionality quickly increase.
Hyaluronic acid and hyaluronan (preparations alflutop, ostenil, fermatron) play a major role in the normal functioning of cartilage. They perform shock-absorbing and lubricating functions, are a substrate for the synthesis of proteoglycans, protect pain receptors of the synovial membrane from irritation, improving the properties of synovial fluid, and facilitate the penetration of nutrients and substances necessary for the construction of the cartilage matrix. The drug alflutop has pronounced analgesic and anti-inflammatory activity in the treatment of patients with different localizations of the pathological process. It should be noted that patients already after the first intra-articular injection of the drug note a clear decrease in pain. According to Professor N.I. Korshunov and co-authors [21], alflutop has a positive effect on articular cartilage. An undoubted increase in the height of cartilage, an increase in the density of cartilage in a number of patients, and even the appearance of visualization of cartilage in a patient with its absence on the femur before the start of treatment with alflutop have been proven, which can be explained either by reparative processes or an increase in the hydrophilicity of the cartilage. Research on the ability of alflutop to have a regenerative effect on cartilage is ongoing. The development of a rapid clinical effect, its persistence for several months, and the absence of radiological progression of osteoarthritis during 3 years of observation can be considered proven. There is no data on the development of any adverse reactions during the use of alflutop.
Hyaluronan preparations of different molecular weights are administered intra-articularly for osteoarthritis - 1.2–1.4 million daltons (Fermatron, Ostenil), 6 million daltons (containing synvisc, hylan). The introduction of hyaluronan derivatives into the joint leads to rapid pain relief and normalization of the properties of synovial fluid [22]. It is necessary to strictly follow the rules for introducing such drugs into the joint cavity. The doctor must have sufficient qualifications, since hyaluronan preparations must be injected exactly into the joint cavity; anesthetics should not be used, since their entry into the joint cavity leads to the disintegration of the drug and a decrease in the therapeutic effect.
In accordance with the recommendations of the European League Against Rheumatism [23], patients with osteoarthritis are shown a combination of pharmacological and non-pharmacological (patient education, weight loss, joint protection, exercise) treatment methods; the location of the lesion, the severity of pain and inflammation, and risk factors for the development of adverse reactions should be taken into account. Pharmacological treatment is carried out with the following drugs:
- paracetamol;
- local therapy agents;
- NSAIDs in the absence of effect from paracetamol, COX-2 inhibitors in the presence of risk factors for adverse reactions;
- opioid analgesics;
- chondroprotectors;
- intra-articular glucocorticosteroids.
In addition, orthopedic and surgical treatment may be prescribed.
It should be noted the importance of orthopedic measures in the management of patients with osteoarthritis. Any violation of the statics of the musculoskeletal system contributes to earlier development and progression of the disease. Correcting flat feet, wearing knee pads, and using orthoses for instability of periarticular tissues can reduce pain and slow down the progression of the disease. Severe joint deformities warrant consultation of the patient with an orthopedic surgeon.
Thus, pain syndrome in osteoarthritis is a significant medical problem, which is associated with the high prevalence of the disease (~12% of the population), the variety of causes of pain, predominantly elderly patients, the presence of many groups of pharmacological agents, the place of which in the treatment of pathology the clinician must take into account, the slow development of the structure-modifying effect of drugs and the difficulties associated with assessing the degree of progression of osteoarthritis, with the need to carry out orthopedic and rehabilitation measures during the complex treatment of the disease.
Literature
- Rational pharmacotherapy of rheumatic diseases: a guide for practitioners. T. III. Ch. 12. M.: Litterra, 2003.
- Bonica JJ The Management of Pain. 2nd ed. Vol. 1; 1990.
- Breivik H., Collett B., Ventafridda V. et al. Eur J Pain. 2005; .
- Smith M.M., Ghosh P. Osteoarthritis: Current status and future directions // APLAR J. Rheum. 1998; V. 2: 27–53.
- Pincus T., Sokka T. Abstract presented during the American College of Rheumatology 2005 Scientific Sessions. San Diego, California.
- Smith M.M., Ghosh P. Osteoarthritis: Current status and future directions // APLAR J. Rheum. 1998; V. 2: 27–53.
- Ruoff G. Management of pain in patients with multiple health problems: a guide for the practicing physician // Amer. J. Med. 1998; 105(1B):53–60.
- Janssen M., Dijkmans B., van der Sluijs FA Upper gastrointestinal complaints and complication in chronic rheumatic patients in comparison with other chronic diseases // Br. J. Rheum. 1992; Vol. 31: 747–752.
- Ruoff G. Management of pain in patients with multiple health problems: a guide for the practicing physician // Amer. J. Med. 1998; 105(1B):53–60.
- Garcia Rodriguez LA, Hernandez-Diaz S. The relative risk of upper gastrointestinal complications among users of acetaminophen and non-steroidal anti-inflammatory drugs // Epidemiology. 2001; 12:570–576.
- Ostensen M. Cartilage changes in arthritis do non-steroidal antiphlogistics have positive or negative effects? // Tiddsskr-Nor-Laegeforen. 1991; V. 111: 838–840.
- Haskinsson E.C., Berry H., Gishen P. et al. Effects of anti-inflammatory drugs on the progression of osteoarthritis of the knee// J. Rheum. 1995; 22: 1941–1946.
- Rashad S., Revell P., Hemingway A. et. al. Effect of non-steroidal anti-inflammatory drugs on the course of osteoarthritis // Lancet. 1989; i: 519–522.
- Hajjal HEL, Marcelis A., Devogelaer JP, Manicourt DH Celecoxib has a positive effect on the overall metabolism of hyaluronan and proteoglycans in human osteoarthritic cartilage // J. Rheum. 2003; 30:2444–2451.
- Rational pharmacotherapy of rheumatic diseases: a guide for practitioners. T. III. Ch. 12. M.: Litterra, 2003.
- Lequesne M., Brandt K., Bellamy N. et al. Guidelines for testing slow acting drugs in osteoarthritis // J. Rheum. 1994; V. 21: 65–73.
- Reginster JY, Deroisy R, Rovati LC et al. Long-term effects of glucosamine sulphate on osteoarthritis progression: a randomized, placebo-controlled clinical trial// Lancet. 2001; V. 357: 251–256.
- Pavelka K., Gatterova J., Olejarova M. et al. Glucosamine Sulfate use and delay of progression of knee osteoarthritis // Arch. Int. Med. 2002; V. 162: 2113–2122.
- Alekseeva L.I. Modern approaches to the treatment of osteoarthritis // Breast cancer. 2003. T. 11. No. 4. pp. 201–205.
- Lequesne M., Maheu E., Cadet C. et al. Structural effect of Avocado/Soybean Unsaponifables on joint space loss in osteoarthritis of the hip // Arth.Care Res. 2002; 47:50–58.
- Korshunov N.I., Baranova E.Ya., Parusova N.I. et al. Alflutop in the treatment of patients with osteoarthritis // Russian Rheumatology. 1998. No. 2. P. 26–31.
- Mensitieri M., Ambrosio L., Iannace S. et al. Viscosoelastic evaluation of different knee osteoarthritis therapies// J. Mat. Med. 1995; 6 (3): 130–130.
- Jardan KM, Arden NK, Bonnwarta B. et al. EULAR recommendations 2003: an evidence based approach to the report of Task force of the standing Committee for International Clinical Studies including therapeutic trials // Ann. Rheum. Dis., 2003. P. 1–13.
N.V. Chichasova , Doctor of Medical Sciences, Professor of MMA named after. I. M. Sechenova, Moscow
Secondary joint pain:
Tendinitis
inflammation of the ligaments and tendons of the legs. The joints of the legs are fixed by a large number of ligaments and tendons, so with tendinitis, both the ligaments and the joints themselves hurt. Typically, pain appears when moving and pressing on the tendon, accompanied by redness and increased temperature of the skin. With tendinitis, the strength of the tendons decreases, which causes the mobility of the legs to be impaired, and painful tendon ruptures and joint dislocations can occur.
Diseases of the lumbosacral spine
The sciatic nerve, which is responsible for the sensitivity of the legs, is attached to the sacral spine, so diseases of the sacrum and lower back cause pain in the legs. The appearance and mobility of the joints remain normal, but pain occurs simultaneously in all joints, more intense in the hip and weaker in the joints of the feet. Pain in diseases of the spine is constant, does not subside during rest and intensifies with prolonged sitting. In this case, there are sensations of numbness and “goosebumps” on the skin, coldness of the limb, a feeling of weakness and heaviness in the legs.
Why does an exacerbation of joint diseases occur in the fall?
There are several reasons for autumn joint pain.
1. Decreased physical activity. With the arrival of cold weather, rainy weather, the appearance of the first frosts and ice, our physical activity inevitably decreases. The joints work less, they do not “warm up”, blood circulation slows down, and the joint fluid lubricates the joint less well. A joint that does not receive enough nutrition begins to wear out and hurt.
2. Cold. With autumn comes the first cold weather. Moreover, if we are already mentally prepared for the winter cold and dress warmly, then in the fall we carelessly forget to warm ourselves. A decrease in temperature causes spasm of the muscles located around the joint. The result is impaired blood flow and metabolism, lack of nutrition to the joint. In addition, autumn weather provokes a decrease in immunity, which means it increases the risk of infectious diseases. The infection causes inflammatory processes, including in the joints. Chronic inflammation also makes itself felt.
3. Stress. Temperature changes become an inevitable shock for the body. Stress weakens all body systems, including immune, metabolic, and muscle systems. All this, one way or another, provokes an exacerbation of diseases. And joint diseases are no exception.
Dmitry Raevsky, head of the international center for psychosomatics “Zdravnitsa,” suggests looking at autumn joint ailments as a whole: “From the perspective of integrative medicine, the cause of autumn pain in the joints is a burdened constitution. Previous illnesses and illnesses of parents do not allow a person to feel good during periods of weather changes. Modern medicine offers painkillers and physical therapy without addressing the cause. What can be done here and now: protect yourself from cold and dampness, sleep on the most comfortable bed, avoid unusual stress, as well as spicy, pickled, spicy foods.”
Treatment of pain in the joints of the legs
If you have pain in your leg joints, do not self-medicate under any circumstances. Due to improper treatment, complications can arise, which are much more difficult to cure than the primary disease. Make an appointment with a neurologist or orthopedic traumatologist. The doctor will listen to complaints, perform palpation, and prescribe additional examinations: ultrasound, MRI, arthroscopy and laboratory tests.
Once the diagnosis is made, the doctor will create a treatment plan. Treatment of joints includes taking various medications: anti-inflammatory, antibiotics, chondroprotectors or hormonal. Almost all patients are prescribed physical therapy and physiotherapy. In advanced cases, prosthetic surgery is performed.
What are the benefits of sea water?
The chemical composition contained almost the entire periodic table. Water procedures improve the health of the entire body:
- Under the influence of water, the skin is strengthened and rejuvenated.
- The functioning of the endocrine system is stabilized.
- During swimming, all muscle groups work and joints are developed.
- The processes of skin regeneration are accelerated.
- Toxins are removed.
- The iodine contained in water actively burns fat deposits.
- The respiratory system is restored.
- Hair and nails are strengthened.
Sea water has a positive effect on joints. During water procedures, salt deposits are broken down and motor activity is developed. Doctors recommend that patients with disorders of the musculoskeletal system undergo joint treatment at least once a year, making trips to the sea.
Joints hurt after the sea
Our readers successfully use Artreid to treat joints. Seeing how popular this product is, we decided to bring it to your attention. Read more here...
It is very important that the patient promptly seek medical help when all the joints of the body hurt; the cause and treatment can only be determined by a specialist. Your doctor will analyze your symptoms and tell you where to go. With age, a person's joints begin to gradually wear out.
Is it possible to sunbathe with a problem thyroid gland?
It is unrealistic to give a specific answer without knowing the details of the diagnosis and condition. In any case, you should be careful and not get carried away with tanning, especially in hot countries.
Before the arrival of the summer season, it is imperative to consult an endocrinologist, and perhaps do a hormonal blood test.
This will allow you to find the multifunctional state of the thyroid gland. The doctor can give some advice on whether it is possible to go to the sea if you have a thyroid problem and sunbathe or whether you should not do this.
Is it possible to go to the sea with arthritis?
- Rudnitskaya L. Arthritis and Arthrosis. Prevention and healing. - SPb.: Peter. 2012. - 224 p. series “Home Doctor” ISBN 978-5-459-01123-4
- O. N. Rodionova. Arthritis ( collective designation for diseases (damages) of joints of inflammatory etiology
). Favorite methods of recovery and prevention.© “Vector”, 2013
Have you been trying to heal your JOINTS for many years?
Head of the Institute for the Treatment of Joints: “You will be amazed at how easy it is to cure your joints by taking the product every day for 147 rubles .
Our readers successfully use Sustalaif to treat joints. Seeing how popular this product is, we decided to bring it to your attention. Read more here...
Special Recommendations
A doctor selects a sanatorium for the treatment of joints. This is due to the fact that each sea contains different amounts of salts and minerals. For example, the concentration is:
- Dead Sea - 270g/l;
- Red - 42g/l:
- Mediterranean - 38g/l;
- Black Sea - 18g/l;,
- Caspian - 14g/l;
- Azov Sea - 11g/l;
- Baltic - 7g/l.
The oceans contain 35g/l of salt. Concentration is important for arthrosis and other pathologies, if there are concomitant diseases for which sea water with a significant salt content is contraindicated. Domestic resorts are suitable, where the patient will not feel a sharp change in climate, which will have a beneficial effect on the general condition of the body and provide maximum comfort.
Is it possible to sunbathe with arthritis?
Before choosing a vacation destination, you should consult your doctor. The use of sunbathing for rheumatoid arthritis is strictly contraindicated. And in case of psoriatic disease, the ultraviolet rays of the sun help to heal. Already on the 3rd day of tanning, improvements are noticeable. In order for your stay at the resort and tanning to have a beneficial effect on your joints, you need to consider the following recommendations:
- The climate cannot be changed abruptly; the disease may worsen.
- It is advisable to be in the sun in the morning and evening, increasing the time of insolation gradually.
- During the day you need to be at home when the sun is active.
- To reduce the negative impact of ultraviolet rays, you need to stay in the shade longer, wear closed, light-colored clothing, and use sunscreen sprays and creams.
- The time spent in water and sunbathing should begin with 10-12 minutes, gradually increasing.
- During the rest period, you need to take into account acclimatization.
A patient with arthritis must find the best option for himself, in which sunbathing will not aggravate the disease. Mud therapy can be used as an auxiliary therapy to water and solar procedures. The procedure helps strengthen muscles, increase the range of motion of joints and improves the overall condition of the body.