Knee arthroplasty is a modern method of surgical treatment of the knee using high technology. In some cases, when a person suffers from pain in this area and is severely limited in mobility due to knee pathologies, knee replacement surgery becomes the only effective solution for improving the quality of life and getting rid of pain.
Indications
Knee replacement surgery is called arthroplasty. Like any other serious invasion, it is carried out only when indicated.
The latter include:
- severe limitations in knee mobility due to wear and tear or injury;
- severe pain in the knee area, felt even in a stationary position;
- irreversible changes in the joint caused by osteoarthritis;
- knee damage as a result of injury;
- deformations;
- diagnosed death of bone tissue as a complication of impaired blood supply;
- deformations or destruction resulting from a number of diseases (gout, rheumatoid arthritis, hemophilia);
- disorders that provoke abnormal bone growth of the lower limb.
Installation of a knee joint prosthesis is an operation of a fairly high level of complexity. This is a radical treatment method. Replacement is usually done if the disease progresses despite best efforts with therapy.
Postoperative complications
Despite all the measures taken to prevent complications, there is still a risk of their occurrence. They can develop due to incomplete preoperative examination of the patient or errors by the operating doctor. However, more often, improper postoperative care and non-compliance with the physical activity regimen outside the hospital are to blame for the occurrence of complications.
One of the most common complications is dislocation of the implant head. It is characterized by pain that intensifies with movement, muscle spasm around the hip joint, and forced positioning of the operated leg. Characteristic symptoms of this complication after hip replacement are lameness and shortening of the affected limb.
In the presence of an untreated chronic inflammatory process in the patient’s body, there is a possibility of developing paraprosthetic infection in the tissues surrounding the endoprosthesis. In the future, it can lead to the formation of a purulent fistula and the development of osteomyelitis. The inflammatory process is characterized by severe pain, swelling and redness in the area of the operated joint. The skin becomes hot to the touch, and the patient develops a fever.
Severe complications include periprosthetic fracture of the femur. It is characterized by acute, sharp pain, rapidly increasing swelling, redness, crunching when moving and palpating the operated area, deformation of the leg and the impossibility of active movements.
During the operation, there is a risk of damage to the fibular nerve, resulting in the development of neuropathy. It is characterized by intermittent pain of various localizations, weakness of the ankle joint, and a feeling of numbness in the toes and feet.
The most dangerous complication is pulmonary embolism, when a blood clot that breaks off during surgery clogs its lumen. The patient suddenly develops shortness of breath, weakness, and suffocation. The patient loses consciousness. If urgent resuscitation measures are not provided, death occurs. This complication is quite rare.
Knee replacement surgeries
Knee replacement can be done entirely (total) or partially. In the first case, the endoprosthesis replaces both parts of the joint, in the second - only one of its sides (less time in the hospital, better results in terms of restoring mobility, surgery is sufficient for approximately 25% of patients with osteoarthritis).
There are alternatives to arthroplasty, but practice shows that in the long term their results are inferior to knee replacement . Alternative treatments include:
- Osteotomy is an operation to straighten the leg bone so that the load shifts from the damaged part of the knee to the healthy one.
- Mosaicplasty is the transfer of healthy hard cartilage tissue along with the underlying bone (partially) from another part of the knee to the affected area in order to restore it.
- Arthroscopy - washing and treating the affected area to remove pathological formations from pieces of bone and cartilage.
Preparing for surgery
Knee replacement involves a series of procedures - preoperative preparation, medical consultations and physical examination usually begin one month before the scheduled date of surgery.
Preparatory and diagnostic tests will include blood tests, an electrocardiogram (ECG), and urine tests.
Surgery is usually performed under general, spinal or epidural anesthesia.
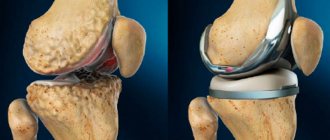
During the procedure, an orthopedic surgeon will remove damaged cartilage and bone and then install a new metal-plastic implant to restore the alignment and function of the knee joint.
Knee endoprosthesis
What is a knee prosthesis? This is a complex design that follows the anatomy and dimensions of the joint being replaced. In other words, an endoprosthesis is the same knee joint, only artificial.
Today, many companies offer a wide range of knee and hip prostheses of various types and configurations. Their designs are constantly being improved to extend their service life after installation and increase the likelihood of normal healing in the knee.
The specific type of prosthesis is selected for each clinical case individually. Only a qualified specialist, after diagnosis and examination, can decide which knee joint prostheses are suitable for restoring the mobility of the patient’s lower limb.
Moreover, all modern endoprostheses (Diamond, Freedom, Lotus, Optimus, Oprtma, Titan) must meet a number of general requirements, including:
- biocompatibility (lack of rejection by the natural tissues of the knee and allergic reactions to the implanted knee joint endoprosthesis );
- load capacity (not lower than that of a real joint);
- the ability to maintain its original shape (during the entire service life, the prosthesis and its components should not be deformed);
- sufficient functionality (knee joint replacement is carried out, among other things, with the aim of restoring normal mobility; accordingly, the endoprosthesis must provide a good range of motion in the lower limb);
- anatomical shape (the knee joint prosthesis must repeat the structural features of the prototype, correspond to the natural dimensions and bends of the leg bone).
Tibial insert FREEDOM
More details
All knee replacements
Classification of endoprostheses
Materials for the manufacture of a knee joint prosthesis to replace the latter: ceramics, metal alloys, polyethylene. Depending on the design features, endoprostheses are divided into models with a movable and fixed platform.
Prostheses with a movable platform have an insert that can rotate in the metal part. This gives additional amplitude when moving the knee after surgery in the medial, lateral direction. In endoprostheses with a fixed platform, the elements - part of the tibial element and the metal component - are firmly connected to each other.
Another classification divides knee replacements into 3 types.
- Unilateral or unicondylar endoprosthesis. It is used for partial replacement of the knee joint in its upper part (prosthetic replacement of an area on one of the femoral condyles).
- Total or bilateral knee replacement (usually metal). Used to replace both parts of the joint (both femoral condyles are covered). The design of such an endoprosthesis differs from the unicondylar one in that it has more powerful attachments to the bone and increased width.
- Total endoprosthesis with axial stabilization. It is also used in total knee replacement operations, when its parts (upper and lower) are fixed with long pins along the longitudinal axes of the femur and tibia. Pins for secure fixation are driven into the space filled with bone marrow (medullary cavity).
Another sign of the classification of knee prostheses is the method of their fixation. There are 2 options: structures installed with cement and cementless methods. In the first case, when replacing a knee joint, its artificial analogue is stabilized (fixed) with quick-curing medical cement. With the cementless method, fixation is carried out as bone tissue grows into the implant.
Cemented knee joint prostheses are more reliable and versatile (used in any type of replacement surgery). An endoprosthesis for cementless installation has a special surface - porous, textured (it provides the opportunity for bone to grow into the implant).
How is the operation performed?
Knee replacement surgery can be performed either under general anesthesia (more often) or under spinal/epidural anesthesia (less often). Takes 1–3 hours. Progress of the procedure:
- an incision is made in the front of the knee (the surgeon opens the kneecap and displaces it to gain access to the tissues of the joint located behind it);
- removal of damaged tissue (femoral head, tibia);
- measuring bones and preparing the prosthesis (the dimensions must be kept extremely accurately);
- cleaning the ends of the bone and installing an endoprosthesis;
- replacement of a section of femoral bone tissue with a curved metal element;
- the end of the tibia is replaced with a plate (also metal, but flat);
- installation of a plastic gasket between the elements of the knee prosthesis (it replaces the cartilage necessary to reduce friction during movements);
- replacing the back of the kneecap if necessary;
- applying sutures or clamps and a bandage (sometimes it is replaced with a splint to fix the limb in a stationary position).
Rehabilitation
After knee replacement, the patient remains under observation (in the hospital) for 3–5 days. During this time, he undergoes a special course of exercises (physiotherapy to strengthen the knee).
Features of the rehabilitation period:
- swelling of the feet and legs is likely;
- movement - with the help of special means (metal frame or crutches);
- classes can be carried out on a simulator for passive movement (the patient remains in bed, the leg is fixed in an elevated position, and a special support makes movements of the knee, which improves its blood supply and helps reduce swelling);
- There may be noticeable discomfort when walking and making leg movements (this is normal).
Complete rehabilitation after knee replacement can take up to 2 years, but the patient can often move independently without special aids after 6 weeks. And after 2 months, many are already driving vehicles.
Exercises after knee replacement
During the recovery period, doctors recommend performing a standard set of tasks: flexion and extension of the knee joints, pulling the operated leg up. At an early stage, exercises should be performed lying on your back. At a later stage - standing, using a chair or table for support.
Exercise No. 1
- Sit on a chair.
- Place your feet on the floor.
- Bend and straighten the limb at the knee, making sliding movements with the heel on the floor.
Exercise No. 2
- Sit on the edge of a chair, place your heels on the floor.
- Straighten your leg and pull your foot towards you.
- Keep your back straight.
- Lean forward until you feel a stretch on the back of your thigh muscles.
- Hold your body in this position for 5 seconds.
- Straighten up, return to your original state.
Exercise #3
- Stand next to a chair or table, holding onto it with your hands.
- Shift your body weight from one side to the other.
- Lift one leg off the floor and lift it, holding for 4 seconds.
- Place it on the floor.
- Distribute body weight evenly.
- Repeat the task, maintaining balance alternately on the healthy and sore leg.
A person with an implant will have to limit his sports hobbies throughout the rest of his life. Football, hockey, and weightlifting are contraindicated for him. Swimming, cycling, skiing and race walking are allowed.