According to statistics, parents of three out of a hundred babies experience hip dysplasia in a newborn.
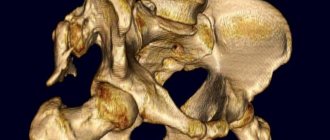
Doctors use the term “dysplasia” to mean congenital underdevelopment of a joint, which leads to disruption of its function and, in the most severe cases, can cause chronic hip dislocation.
Such a disease, if left untreated, does not end well. Impaired function of the lower limb, gait, pain in the hip joints and a high risk of disability are the consequences of advanced dysplasia. Therefore, all parents need to know the first signs of hip dysplasia in children and understand the importance of timely visits to an orthopedist. Early diagnosis and proper treatment will help avoid complications. Remember, the earlier the diagnosis is made, the more favorable the prognosis will be!
There is still no consensus among experts regarding the development of hip dysplasia in children. According to one version, the main reason is a malformation of articular tissues in the early stages of pregnancy (the first 2-3 months). This is predisposed by unfavorable ecology, exposure to toxic substances and some infectious diseases.
According to another theory, the development of joints is affected by high levels of oxytocin, the hormone that causes the onset of labor. Accumulating towards the third trimester, oxytocin increases the tone of the fetal femoral muscles, as a result of which subluxation of the hip joints gradually develops. Perhaps this is the reason for the greater prevalence of dysplasia among girls (5 times more often than boys), who are more susceptible to the influence of the mother’s hormonal levels.
The risk is also increased by incorrect intrauterine position of the fetus and prolonged difficult labor (in the breech position).
The tendency to dysplasia is often inherited, so if one of your relatives has already had such cases, you need to think about early diagnosis in advance.
The first signs of hip dysplasia in children
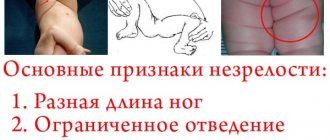
Parents themselves may suspect something is wrong, even before consulting an orthopedist. Most often this occurs in severe forms of the disease, when the head of the femur completely comes out of the socket. In milder cases, only a specialist can determine the presence of dysplasia, since subluxation and pre-luxation of the hip joint practically do not manifest themselves externally. However, there are main signs:
- limited mobility (spreading) of the hips; often the baby begins to cry when trying to move the leg to the side;
- asymmetry (mismatch) of the inguinal and gluteal folds, which become more pronounced on the damaged side.
But the presence of only these symptoms in hip dysplasia in a child is not an absolute sign of the disease and may be a consequence of impaired muscle tone.
In the event of a dislocation, the hip joint practically loses its function, and the affected leg is shortened. A “clicking symptom” occurs - the head of the femur slips from the surface of the joint when the child’s legs are bent at the knee and hip joints, as well as its reduction when they are separated.
Hip dysplasia?
Daria
1882 views
August 11, 2020
Good afternoon From birth, the child had poor separation of the legs at the hip joints. At the same time, the right leg was abducted worse. One month ago we were unable to show the child to specialists at the clinic because there was self-isolation. At 3 months, I learned that a child should normally spread his legs well when I saw a photo of my roommate’s baby from the maternity hospital. I myself started giving my daughter massages and gymnastics. As a result, the legs began to separate much better, but the right side was still more constrained than the left. They were able to show the child to an orthopedist only when he was closer to 5 months, or, to be more precise, at 4 months and almost 3 weeks. Until that time, I wasn’t very worried, because we had an ultrasound scan for the child a month ago - everything was normal there, plus the local pediatrician examined us during a visit and didn’t say anything bad about the legs at all. The orthopedist sent us for an x-ray, based on the results of which he diagnosed hip dysplasia. He prescribed a massage, physio and wearing a Freika feather bed. At the first massage session, the massage therapist was surprised that we were given such a diagnosis and asked on what basis they made it. Next we went to an osteopath (by this time 3 massage sessions and physiotherapy had passed). The osteopath, having examined the child, said that there was no dysplasia, there was dystonia and a block along the entire right side. She only worked with the child for 1 session, she said that the child did not need any more, as he was healthy. Of everything prescribed by the orthopedist, I recommended leaving only massage and eliminating the rest. We decided to go to another orthopedist, showed an x-ray, he examined the child and concluded that the child was healthy. He said not to wear a feather blanket, I didn’t ask about physio, but in the end we ruled out both physio and feather blanket. The other day we vaccinated a child and before the vaccination, the pediatrician examined the child at a paid clinic. Seeing asymmetrical folds on the child’s buttocks, I again questioned dysplasia. It also seemed to her that when you put the child on her legs, she slightly bends her right leg, “as if she were protecting her” (this is a quote). She told us to show the child to another orthopedist somewhere in MONIIAG or RDKB in Moscow. I again doubted the child’s lack of diagnosis, took out an x-ray with a conclusion and saw that it said “x-ray picture of asymmetry of the ossification nuclei of the femoral heads.” How serious is this conclusion? Will the cores be able to align and how can we help them with this? And, looking at the X-ray, do you see dysplasia or asymmetry of the nuclei and that is dysplasia? We have made an appointment with one more orthopedist in our city for the end of the week. There is still a long wait for an appointment, so I decided to ask for opinions here on the site. What advice do you have for us? Otherwise I'll go crazy by the end of the week. I am attaching photographs of the x-ray with the report and the report of the orthopedist.
The question is closed
hip dysplasia
asymmetry of ossification nuclei
Diagnosis of hip dysplasia
If hip dysplasia was not diagnosed in the first 6 months of life after childbirth, then the damage to the joint progresses - the limb shortens even more, a pathological (“duck”) gait or intermittent claudication (with bilateral dislocation) is formed.
Diagnosis of dysplasia is often carried out in the maternity hospital. If this does not happen (recently, ultrasounds are done only if there are problems), then parents can ask the pediatrician to conduct an examination themselves. It is safe for the baby’s health and guarantees high accuracy of diagnosis.
However, if a single ultrasound showed normal development of the joints, still do not forget about constant monitoring by an orthopedist. Routine examinations will help your child avoid possible problems.
The first visit to the orthopedist should take place no later than 1 month, at which time a mandatory ultrasound of the hip joint is performed. This is an indispensable condition for the early diagnosis of dysplasia. A repeat examination is carried out at the end of the 3rd, beginning of the 4th month, at which time the doctor may recommend taking an x-ray. The most difficult to diagnose is subluxation of the hip joint, which practically does not manifest itself at all and can only be seen on an x-ray.
Take preventive observation with an orthopedist seriously - the timing of the examination is not appointed by chance, each of them is associated with an important stage in child development. So, if dysplasia was detected in the first 3 months of the baby’s life, then after a course of treatment the functionality of the joint is completely restored (usually by 6-8 months), and there are no long-term consequences.
Opinion about hip dysplasia + survey
Hip dysplasia in children of the first year of life This terrifying name makes most parents tremble and is often discussed by them in connection with the need to wear splints and other devices. Let’s try to impartially understand this situation, taking into account the fact that “medicine is an inexact science.” 1. So, even among orthopedic doctors there is no single, clearly defined concept of the diagnosis of “hip dysplasia” (hereinafter referred to as DHS). This is confirmed by the results of the general medical examination of children held in Russia in 2008. For example, in a group of children under one year old in some areas of St. Petersburg, the incidence of hip dysplasia (HJD) was 40% (that is, almost every second child), while in other areas the level of hip dysplasia (HJD) was 3 - 8%. Naturally, different areas of the city cannot differ so much in the frequency of traffic accidents. This means that orthopedic doctors from different clinics have completely different approaches to diagnosing “hip dysplasia.” 2. Next. Why is all this being done? That is, why do doctors so carefully and persistently prescribe treatment for DTS? If you are told that a child with hip dysplasia (HD) will not walk or will limp, then this is not so. The likelihood of lameness is only in the extreme form of hip dysplasia (DHS) (complete dislocation of the hip), which occurs in 1 in 1000 children, and then in the absence of treatment or its failure. The rest of the children with hip dysplasia (HJD) walk normally and look no different from their peers. So this is all done with the goal of preventing premature hip failure in adulthood. A joint that has complete alignment (centration) of the femoral head and socket serves well throughout life; joints with poor centering wear out faster due to uneven load distribution.
The degree of centration can only be reliably determined by ultrasound or x-ray examination. The quality of instrumental research methods is determined by a number of factors: the correct positioning of the patient, the correct choice of sensors and radiation characteristics, the resolution of the equipment, etc. The level of compliance with these parameters is always visible on radiographs or sonograms (ultrasound images). So, let us emphasize once again that the sign of joint centration is the most important, determining future development and function. The remaining signs revealed in children during instrumental examination of the hip joints do not necessarily indicate pathology and can occur in completely healthy children (absence or delayed appearance of ossification nuclei of the femoral heads, poor development of the bony part of the socket, etc.) 3. Naturally, every child is individual, and you (the parents) are not afraid of the fact that a child at 5-6 months does not yet have teeth and, for example, a large fontanel has not “closed.” You are sure that the teeth will grow and the fontanel will harden. Although both of these conditions can be described as “oral dysplasia” and “cranial dysplasia”. The same is true with the DTS sign. After all, in essence, DTS is weak, incomplete development of the joint. In most cases, it is a natural feature of the body of a small child, and much less often a sign of a disease. Thus, the problem of hip dysplasia (HD) is such for parents more because of the frightening sound of the diagnosis and the lack of everyday experience on this topic than because of the actual seriousness of deviations in the development of the hip joint.
link
Please leave messages about your opinion. I would like a discussion.
Treatment of hip dysplasia
The younger the child, the easier it is to treat dysplasia. For example, in babies up to 3 months old, the joint can recover on its own, provided that the children's legs are always in the right position. That is why the main method of treatment in the early stages of the disease is free swaddling, in which the baby’s legs are spread apart.
But if treatment and prevention were not carried out in the first 3 months of life, then more serious and long-term treatment will be required for a complete recovery. The danger of unrecognized dysplasia is that the baby’s bones, due to age, are very flexible and susceptible to various deformations. The baby’s skeleton is constantly growing, but this same factor also explains his greater tendency to developmental defects. Most joints (including the hip) in the first months of life consist mainly of cartilage tissue, and any disturbances in the connection of the bones lead to the formation of serious deformities. To stop the progression of the disease, it is necessary to return all parts of the joint to their normal position. For this, various types of abductor splints (listed above) are usually used; they hold the baby’s legs in the desired position. After some time, the joint gradually “fixes” and begins to develop correctly.
At the age of 2-3 months, small patients with suspected dysplasia are usually not given x-rays, since even with an unconfirmed diagnosis it is customary to prescribe a preventive course of treatment: the use of soft spreading splints, a course of therapeutic exercises (with abductor-circular movements) and massage of the gluteal muscles . Splinting and massage work well with physical therapy techniques to speed up recovery.
Observation of hip dysplasia
By the end of the first year of life, all babies again undergo a routine examination by an orthopedist. Then several groups are conventionally distinguished:
- children with dysplasia who have not received any treatment;
- children with severe, poorly correctable forms of dysplasia;
- babies with residual symptoms of dysplasia.
Each child, if necessary, is prescribed further treatment - conservative (massage, gymnastics, physiotherapy) or surgical intervention. If the diagnosis of “irreducible dislocation” is confirmed, then surgery is necessary - open reduction of the joint under anesthesia.