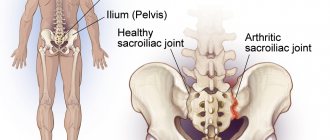
The sacroiliac joint (SIJ) is the joint between the spine and pelvis.
- This is a large diarthrodial joint, which is formed by the articular surface of the sacrum and the pelvic (nameless) bone.
- Each innominate bone is formed by the fusion of three pelvic bones: the ilium, the ischium and the pubis.
- The SIJs are necessary for the effective transfer of load between the spine and lower extremities.
- It functions as a shock absorber for the spine and converts torque from the lower extremities to the rest of the body.
- The sacrum, pelvis and spine are functionally interconnected through muscles, ligaments and fascia.
Available moves
- The main function of the SIJ is to provide stability and reduce forces acting on the lower extremities.
- A strong ligament system in a joint makes it more stable and limits the amount of movement available.
- Nutation and counternutation are movements that occur in the sacroiliac joints.
Nutation is a movement that occurs when force (weight) is absorbed at the sacroiliac joint and occurs in the direction of gravitational forces (toward the floor). Contusion is the reaction of the body lifting a joint against the force of gravity. In most people, this movement is limited to 2-4 mm of motion due to the bony architecture and ligamentous structures of the joint.
Friends, on September 21-22 in Moscow, as part of the RehabTeam project, a seminar by Georgy Temichev “Lumbar Region” will take place. Find out more...
Nutation occurs
- When the sacrum absorbs a shock, it moves downward, forward, and rotates in the opposite direction.
- As the sacrum moves forward and downward, the coccyx moves backward relative to the pelvic bones.
- This movement is impeded by the wedge-shaped shape of the sacrum, the projections and concavities of the articular surfaces, the coefficient of friction of the articular surface, and the integrity of the posterior, interosseous, and sacrotuberous ligaments, which are also supported by the surrounding muscles.
counternutation
- The sacrum moves up, back and rotates in the same direction that absorbs the force. This movement is prevented by the posterior sacroiliac ligament, which is supported by the multifidus muscle.
Ligaments and joint capsule
- The SIJ is a diarthrodial synovial joint.
- It is surrounded by a fibrous capsule containing the joint space filled with synovial fluid.
- The articular surfaces are composed of two strong C-shaped layers.
- The SIJ is distinguished from other synovial joints by the unusual articulation of two different types of cartilage.
- The sacral capsular surface is formed from hyaline cartilage (hyaline cartilage is composed of type II collagen and is the weakest type of cartilage).
- The iliac capsular surface is composed of fibrocartilage (fibrous cartilage is composed of type I collagen and is the strongest type of cartilage).
A powerful ligamentous system stabilizes the SIJ. It is weaker in women compared to men, which allows them to give birth.
- The anterior sacroiliac ligament is an anteroposterior thickening of the fibrous capsule that is weak and thin compared to other ligaments of the joint. It connects the third sacral ligament to the lateral side of the preauricular groove and is better developed closer to the arcuate line and the posterior superior iliac spine (PSI). This ligament is the most commonly injured and is a common source of pain due to its thinness.
- The interosseous sacroiliac ligament forms the main connection between the sacrum and the pelvic bone and is a strong, short ligament deeply adjacent to the posterior sacroiliac ligament. It prevents anterior and inferior movement of the sacrum.
- The posterior (dorsal) sacroiliac ligament connects the VPO to the lateral crest of the third and fourth segments of the sacrum; she is very tough and strong. Nutation, which is an anterior movement of the sacrum, loosens the ligament, and counternutation, which is a posterior movement, tightens the ligament. It can be palpated directly under the PVPO; it is often a source of pain.
- The sacrotuberous ligament consists of three large fibrous bundles and connects to the posterior (dorsal) sacroiliac ligament. It prevents nutation of the sacrum and counteracts posterior and superior movement of the sacrum during weight bearing.
- The sacrospinous ligament is triangular in shape and thinner than the sacrotuberous ligament. It runs from the ischium to the lateral parts of the sacrum and coccyx. Together with the sacrotuberous ligament, it prevents the sacrum from tilting forward relative to the pelvic bones when carrying heavy loads.
Specific pathologies
Sacroiliac joint dysfunction is a commonly used term that refers to abnormal biomechanical function of a joint. Some causes of SIJ dysfunction include the following conditions.
Consequences of injury
- Increased mobility of the SIJ may be the result of damage to the above ligaments. This can be seen in motor vehicle accidents, falls, overuse injuries, and also in sports.
Hypermobility
- May be genetically determined. The term often denotes multidirectional instability. Other causes of inherited weakness may include Marfan syndrome and Ehlers-Danlos syndrome.
- Hormonal changes can also cause hypermobility. The SIJ ligaments weaken during pregnancy due to the hormone relaxin. This weakening, along with weakening of the symphysis pubis, allows the pelvis to expand during childbirth. Ligaments can also be stretched due to increased lumbar lordosis. Thus, SIJ-related pain is common during pregnancy. However, this pain may persist after pregnancy if the ligaments do not return to their normal state. Risk factors include prolonged labor and large babies.
Degeneration
- Structural changes in the joint can also lead to dysfunction. People with altered gait, spinal deformities, or leg length discrepancies may have reduced traction in the SIJ, resulting in SIJ weakness and pain. This equates to repeated and uneven stress on the articular surfaces of the SIJ, causing weakness and pain.
Osteoarthritis of the SIJ
- Osteoarthritis of this joint is also common, and the incidence increases with age. Other risk factors for developing osteoarthritis include previous trauma.
Inflammation
- Inflammation or sacroiliitis. There are many causes of sacroiliitis. Among the causes of infectious sacroiliitis are brucellosis. This condition may also be associated with other inflammatory pathologies such as inflammatory bowel disease and seronegative spondyloarthropathy.
Diagnosis of arthrosis of the sacroiliac joint
Like any degenerative-deforming process, arthrosis of the iliosacral joint requires complex diagnostic measures. The patient is prescribed a number of examinations:
- general blood test - shows the presence of an inflammatory process;
- blood test for specific markers of inflammation;
- radiography - reveals narrowing or complete fusion of the joint space, the degree of contact of the articular surfaces, the presence of osteophytes, the condition of the cartilage tissue;
- MRI – visualizes changes at any stage of the process, reveals deviations in the structure of ligaments and muscles;
- synovial fluid analysis;
- densitometry – hardware examination of bone tissue density if osteoporosis or osteomalacia is suspected;
- mass spectrometry - blood test for vitamin D levels.
In 96% of cases, bilateral arthrosis of the sacroiliac joints is diagnosed.
Epidemiology
The prevalence of SIJ pain in chronic low back and lower extremity pain has been reported to range from 10 to 27%. There are several reports of predisposing factors for SIJ pain, such as leg length discrepancy, age, arthritis, previous spinal surgery, pregnancy, and trauma. Compared with facial and discogenic low back pain, SIJ pain is more often associated with a specific inciting event and is characterized by highly variable pain patterns.
Physical therapy
The goal of the first stage of treatment is to reduce inflammation with ice packs and anti-inflammatory medications.
The second goal is to improve mobility through mobilizations, manipulations, or exercise therapy.
If there are complaints of instability, it may be helpful to use a sacroiliac belt for temporary pelvic support, as well as progressive stabilization training to improve motor control and stability.
If the SIJ is severely inflamed, a sacroiliac belt can also be used.
Postural and ergonomic recommendations will help the patient reduce the risk of re-injury.
Core stability
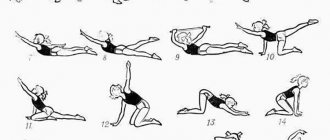
Exercise is a core component of a SIJ pain management program. Exercises that focus on improving core stability have been shown to be effective in this case.
Stabilization exercises
- In order to concentrate on contracting the local muscles of the lower back (without involving the global muscles), it is necessary to improve proprioception and motor control. It is also necessary to work in an isometric mode with two main stabilizers - the transverse abdominis and multifidus lumbar muscles. These muscles need to be trained at low levels of maximal voluntary isometric contraction. It is important to maintain controlled breathing and neutral lordosis during resistance exercise. The following principles must be followed: inhale and exhale, pull the lower abdomen below the navel carefully and slowly, without moving the upper abdomen, back or pelvis. In addition, the physical therapist may palpate the multifidus muscles. This is necessary to ensure effective muscle activation.
Special tests
- Clinical evaluation of a patient with SIJ dysfunction begins with assessment of gait and leg length differences.
- During the physical examination, the Fortin finger test should be performed. The test is considered positive when the point of tenderness is within 2 cm inferomedial to the PVPO.
- To exclude other pathologies, the hip joint and lumbar spine should be assessed in addition.
KPS stress tests
- Gillette test - performed in a standing position. The patient stands on one leg while flexing the opposite hip and knee. SIJ motion is assessed by placing one thumb under the VEPO on the side of the flexed hip and the other thumb in the midline at the S2 level. Normally, the thumb under the VPO moves lower and to the side when the hip flexes. The limitation is manifested by a decrease in the movement of the thumb compared to the healthy side.
- You can also use the Laslett test cluster. It includes the distraction test, compression test, femoral trust, sacral trust and Gaenslen test.
Disease prevention
Since arthrosis is an age-related disease, it is impossible to guarantee its absence, especially if there is a hereditary predisposition. But it is possible to reduce the risk of its development. For this purpose it is recommended:
- regular moderate physical activity;
- avoid prolonged sitting or standing;
- promptly treat any infectious disease;
- avoid stress and nervous tension;
- do not lift too heavy objects;
- maintain normal weight.
Lower back pain
- The incidence of low back pain resulting from SIJ lesions can reach 27%.
- Patients often describe a specific injury or triggering event.
- Pain originating in the SIJ is probably more common than most physicians realize due to the difficulty in localizing symptoms and associated pain patterns.
- Using a pain chart to determine the location of the pain is often very helpful in diagnosing the problem.
- Pain due to SIJ lesions can be detected at a distance of 10 cm caudal and 3 cm lateral to the PVPO.
- Pain from the SIJ can radiate to the buttocks, lumbar region, groin area and spread along the lateral thigh. Patients with SIJ dysfunction say that their pain increases when getting up from a chair, standing or sitting for long periods of time, or when climbing stairs; They also have morning stiffness.
- Numbness and tingling in the leg may also be present. As mentioned above, risk factors include differences in leg length, age, arthritis, history of spinal surgery, pregnancy and injury.
Treatment of sacroiliitis
The main goal is to eliminate the cause of inflammation.
Working with the patient involves the use of mainly conservative methods, however, surgical interventions can also be used (for purulent forms), which involve opening the purulent focus and removing the affected tissue.
The methods used, the volume and duration of treatment procedures are determined based on the results of confirming the diagnosis, on an individual basis, taking into account the existing characteristics of a particular patient.
Drug treatment of sacroiliitis
Various groups of drugs are used, which may include painkillers, hormonal/non-hormonal anti-inflammatory drugs (NSAIDs), immunomodulators, as well as broad-spectrum antibiotics and chondroprotectors.
Particular attention should be paid to chondroprotectors, the action of which can accelerate regeneration and ensure high-quality restoration of articular tissues.
Physiotherapy
Physiotherapeutic techniques are used exclusively in conjunction with the use of medications. A complex of this kind makes it possible to limit changes occurring in the tissues of the joint, which also helps to maintain its mobility.
The acute and subacute period involves the use of techniques such as electrophoresis and ultraphonophoresis, implemented with the use of drugs.
Other procedures used during recovery include exposure to magnets, laser or infrared radiation, massages, and other specific therapies (mud therapy, steam therapy, etc.).
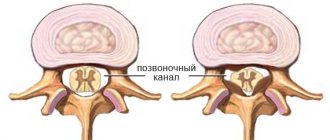
Age-related changes
The SIJ goes through many changes throughout life. In early childhood, the surfaces of the joint are smooth and allow sliding movements in many directions. After puberty, the surface of the ilium becomes rougher, covered with fibrous plaques that significantly limit movement. These age-related changes increase in the third and fourth decades, and by the sixth decade, movement may become noticeably limited. By the eighth decade, plaques and erosions form.