Piriformis syndrome is a pain syndrome that is localized in the gluteal region with possible return (irradiation) to the upper thigh, lower leg and groin area.
Piriformis syndrome occurs in at least 50% of patients with discogenic lumbosacral radiculitis. Reflex tension in the muscle and neurotrophic processes in it are caused, as a rule, by irritation not of the fifth lumbar, but of the first sacral root.
If the patient is diagnosed with this, the assumption of the presence of piriformis muscle syndrome may arise in the presence of persistent pain along the sciatic nerve that does not decrease with drug treatment. It is much more difficult to determine the presence of this syndrome if there is only pain in the buttock area, which is limited in nature and associated with certain positions (movements) of the pelvis or when walking.
CAUSES OF PIRIFYFORMUS SYNDROME
Piriformis syndrome has been familiar to general practitioners for a long time; it can be a complication of lumbar osteochondrosis, a symptom of diseases of the pelvic organs, and a consequence of overload of the piriformis muscle, muscles and ligaments of the lower extremity girdle.
Primary damage to the piriformis muscle is observed in myofascial pain syndrome; the immediate causes of its occurrence may be:
- stretching
- hypothermia
- muscle overtraining
- injury to the lumbosacral and gluteal regions
- unsuccessful injection of drugs into the piriformis muscle area
- myositis ossificans
- prolonged stay in antalgic position
Secondary piriformis syndrome can occur when:
- diseases of the sacroiliac joint
- diseases of the pelvis, in particular gynecological diseases
With vertebrogenic pathology, a reflex muscle spasm may occur. Piriformis syndrome, which develops according to this pattern (not radicular), with muscle-tonic manifestations, is the most common variant of lumbar and hip pain. Pathological tension of the piriformis muscle in the form of a spasm is observed in discogenic radiculopathies with damage to the spinal roots. In these cases, there will be a clinical combination of both radicular and reflex mechanisms with the occurrence of neurological manifestations of vertebrogenic pathology.
Possible vertebrogenic causes include:
- radiculopathy of L1 - S1 roots
- tumors of the spine and spinal roots
- injuries of the spine and spinal roots
- lumbar stenosis
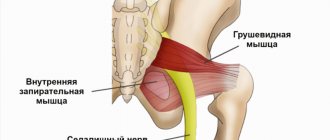
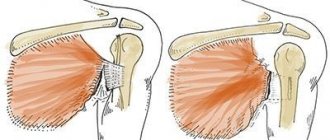
The function of the piriformis muscle is to abduct and externally rotate the hip. At the same time, she extends and abducts the hip, and with a sharp flexor-abduction pose, rotates it. The muscle is involved in “anchoring” the femoral head, similar to the function of the supraspinatus muscle in relation to the head of the humerus. It prevents rapid internal rotation of the hip in the first stage of walking and running. It creates an oblique force on the sacrum; due to its lower part, it provides a “shearing” force to the sacroiliac joint - it pulls its side of the base of the sacrum forward and the apex back. The muscle promotes antinutation (swinging) of the sacrum. If the nutating muscles pull it forward, wedge the sacrum forward, the piriformis pulls its lower sections back towards the posterior sections of the innominate bones.
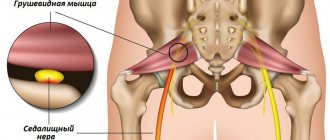
In 90% of cases, the trunk of the sciatic nerve exits the pelvic cavity into the gluteal region under the piriformis muscle. In 10% of cases, the sciatic nerve pierces the piriformis muscle as it passes into the gluteal region. A prerequisite for compression of the sciatic nerve is induration of the piriformis muscle during its aseptic inflammation. The altered piriformis muscle can compress not only the sciatic nerve, but also other branches of the second to fourth sacral nerves - the pudendal nerve, the posterior cutaneous nerve of the thigh, the inferior gluteal nerve.
Thus, with piriformis syndrome it is possible:
- compression of the sciatic nerve between the altered piriformis muscle and the sacrospinous ligament
- compression of the sciatic nerve by the altered piriformis muscle as the nerve passes through the muscle itself (a variant of the development of the sciatic nerve)
- compression of the branches of the second to fourth sacral nerves - the pudendal nerve, the posterior cutaneous nerve of the thigh, the inferior gluteal nerve
Who is at risk?
Pelvic floor muscle dysfunction occurs when the muscles are stretched, weakened, or too tight. Some people have weak pelvic floor muscles from childhood, but more often problems develop as they age. The risk group includes
- pregnant women and those who have already given birth,
- women going through or past menopause,
- women who have undergone gynecological surgery, such as hysterectomy,
- men who have had their prostate gland removed
- high-level athletes such as gymnasts, runners or trampoline jumpers.
Additional risk factors include:
- back pain,
- pelvic trauma or radiation therapy,
- constant constipation (you have to strain to empty your bowels),
- chronic cough or sneezing (asthma, smoking or hay fever),
- overweight or obesity,
- Regular lifting of weights at work or in the gym.
Let's look at these cases in more detail.
Pregnancy and childbirth
affect the physical shape of the pelvic floor muscles. The growing fetus puts pressure on the pelvic floor muscles. During pregnancy, the hormone relaxin is released, which makes tissue more elastic, allowing the muscles and ligaments of the pelvic floor to stretch during childbirth. Sometimes they remain stretched for a long time. The action of relaxin and fetal pressure prevents the muscles from holding the pelvic organs in the correct position.
Women at greatest risk during pregnancy and childbirth are those who:
- gave birth repeatedly
- gave birth using instruments: forceps or vacuum extractor,
- the second stage of labor lasted more than an hour,
- during childbirth there was a rupture of the perineum,
- the baby weighed more than 4 kg.
During menopause
The female body undergoes significant changes. All muscles weaken, including the pelvic floor muscles. Because they support the pelvic organs, problems in this area can occur, particularly difficulty with bladder or bowel control.
Menopause is often accompanied by weight gain, which also weakens the pelvic floor muscles.
The situation is also aggravated by:
- less elastic bladder
- anal trauma as a result of childbirth,
- chronic diseases (diabetes or asthma).
Gynecological or pelvic surgery
Treatments such as hysterectomy or radiation therapy can disrupt the shape of the pelvic floor muscles and cause incontinence.
After prostate surgery
Incontinence also often develops. Most men regain full bladder control within 6 to 12 months, and exercise makes a significant difference.
Professional athletes and just big fitness enthusiasts
often experience constant strong pressure on the pelvic floor. As a rule, these are gymnasts, trampoline jumpers and runners, fans of games in which you have to hit the ground a lot, such as basketball or netball. Athletes who lift weights or do high-intensity interval training are also at risk.
Urinary incontinence may be common when performing these types of exercises, but this is not normal.
CLINICAL PICTURE OF PIRIFOID MUSCLE SYNDROME
Local symptoms
- aching, nagging, “brainy” pain in the buttock, sacroiliac and hip joints, which intensifies when walking, standing, adducting the hip, and also in a squatting position
- the pain subsides somewhat when lying down and sitting with legs apart
- with good relaxation of the gluteus maximus muscle, a dense and painful when stretched (Bonnet-Bobrovnikova symptom) piriformis muscle is felt underneath it
- upon percussion at the point of the piriformis muscle, pain appears on the back of the leg - Vilenkin’s symptom
- soreness of the ischial spine is detected: a palpating finger encounters it, intensively sliding medially upward from the ischial tuberosity
- often tonic tension of the piriformis muscle is combined with a similar condition of other pelvic floor muscles - coccygeus, obturator internus, levator anus, etc. in such cases, symptoms of compression of blood vessels and the sciatic nerve in the infrapiriformis space speak of pelvic floor syndrome
- pain due to compression of the sciatic nerve is dull, “brainy” in nature with a pronounced vegetative coloring (feelings of chilliness, burning, stiffness)
- irradiation of pain throughout the leg or mainly along the innervation zone of the tibial and peroneal nerves
- provoking factors are heat, weather changes, stressful situations
- sometimes the Achilles reflex and superficial sensitivity decrease
- with predominant involvement of the fibers from which the tibial nerve is formed
Certain manual tests help recognize piriformis syndrome:
- pain on palpation of the superior internal region of the greater trochanter of the femur (attachment site of the piriformis muscle)
- pain on palpation of the lower part of the sacroiliac joint - projection of the insertion site of the piriformis muscle
- reproduction of pain during passive adduction of the hip with simultaneous internal rotation (Bonnet-Bobrovnikova symptom)
- test for the examination of the sacrospinous ligament, which allows you to simultaneously diagnose the condition of the sacrospinous and iliosacral ligaments
- tapping on the buttock (on the sore side) - this causes pain spreading along the back of the thigh
- Grossman's symptom - when struck with a hammer or folded fingers on the lower lumbar or upper sacral spinous processes, the gluteal muscles contract
The gluteus medius muscle is called the “lumbago muscle.”
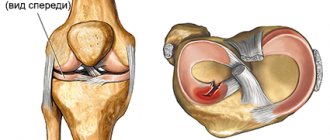
The pain caused by trigger points in this muscle resembles lower back pain, or lumbago. Referred pain spreads predominantly along the posterior part of the iliac crest, as well as into the sacrum and radiates to the posterior and outer buttocks, and can reach the upper thighs. The muscle is innervated through the inferior branch of the superior gluteal nerve by the spinal roots L4, L5 and S1. This is the abductor muscle of the thigh, the main function of which is to stabilize the pelvis in a standing position on one leg. During walking, the gluteus medius muscle prevents the possibility of suddenly falling towards the raised leg. If there are trigger points in this muscle, pain is common when walking, as well as pain when lying on your back or on the affected side and when sitting bent over in a chair. Pain referred from trigger points may resemble pain associated with a sacroiliac joint injury. During the examination of the patient, it is necessary to observe the patient’s gait, exclude the presence of foot deformity, Morton’s neuroma, and also assess the amount of hip abduction in the hip joint.
METHODS FOR DIAGNOSIS OF PIRIFOID MUSCLE SYNDROME
One of the most reliable methods for diagnosing piriformis muscle syndrome is considered to be transrectal palpation of the piriformis muscle, determined in the form of an elastic, sharply painful cord. It is also possible to palpate the piriformis muscle through the gluteus maximus muscle, with the patient “lying on his side”
An important diagnostic test is infiltration of the piriformis muscle with novocaine and assessment of the positive changes that occur. A definitive diagnosis can be made when clinical signs improve as a result of post-isometric relaxation of the piriformis muscle.
PRINCIPLES OF THERAPY
In most cases, correction is required by the primary condition that caused the formation of muscular-tonic syndrome. When the primary source of pain impulse is eliminated, reflex muscular-tonic syndrome can regress. In cases where muscular-tonic disorders become the main or independent source of pain, both local and general effects are used. Stretching, massage of the affected muscle, warming physiotherapy, and manual therapy techniques aimed at mobilizing the affected spinal motion segment are performed. It is advisable to correct the motor stereotype, avoid provoking loads and poses
Block of the piriformis muscle. The point of infiltration of the piriformis muscle is found as follows. The greater trochanter of the femur, the superior posterior spine of the ilium and the ischial tuberosity are marked. These points are connected and a bisector is drawn from the superior posterior spine to the base of this triangle. The required point is located on the border of the lower and middle parts of this bisector. A needle is inserted here vertically to a depth of 6–8 cm and the muscle is infiltrated with a solution of an antiseptic and a steroid.
Then a massage will be performed with post-isometric relaxation of the muscles that rotate the thigh outward.
Gymnastic exercises that are recommended to relax the piriformis muscle and activate its antagonists can be performed in the following order. In the supine position with half-bent legs, the soles resting on the couch, the patient makes smooth movements of connecting and spreading the knees. Then, connecting the bent legs, the patient energetically pushes the other with one knee for 3-5 s. The next exercise, the “cradle,” is performed, if possible, without the help of hands while actively flexing the hips. Then, in a sitting position, they spread their soles wide apart, connect their knees and, leaning on the couch with the palm of their outstretched hand, begin to get up from the couch. By the time the palm comes off the couch, the other hand is offered to the instructor, who helps complete the straightening of the body. At this point, the connected knees are freely separated. When the condition improves, during the regression stage and during the period of remission, it is recommended to sit often (but not for long) in the cross-legged position.
Symptoms
Patients complain of pain that occurs when walking, note discomfort in a sitting position, bent in such a way that under the weight of their own weight there is pressure on trigger points. By avoiding compression on trigger points, patients cannot sleep on the affected side, preferring to lie on their back or opposite side. But in the lateral position, compression of trigger points in the posterior fibers of the gluteus medius muscle is possible. Therefore, it is necessary to place a pillow between the knees, thereby preventing excessive adduction of the thigh in the hip joint and eliminating the painful tension of the compacted bundles of muscle fibers in this muscle. The best position for sleeping is an intermediate option between the positions on the back and on the side, while placing a pillow under the lower back.