The calf muscle is the most important part of the lower limb; it is used when running, walking and other types of loads on the legs. It is formed by two large bundles of fibers that start from the femur.
A calf muscle bruise is a common leg injury that must be treated under the supervision of a specialist, especially if there is serious tissue damage.
What is a calf muscle injury?
A bruise of the calf muscle is understood as a closed mechanical injury to the soft tissues of the leg. Most often, a bruise does not lead to disruption of the anatomical integrity of the muscle, although in serious cases, stretching or even rupture of muscle fibers is possible. A bruise occurs suddenly and affects the body for a limited time.
In most situations, this type of injury comes from:
- impact with a blunt, heavy object;
- falling onto a hard surface.
Typically, muscle injury in the lower leg area is local in nature and can affect not only muscle fibers, but also subcutaneous tissue and tendons. Closed damage to the skin almost always occurs; the integrity of the skin is rarely compromised.
Injury to the calf muscle is common among athletes, and by its symptoms it is difficult to distinguish it from other traumatic lesions in this area (for example, from a sprain, acute muscle strain).
Getting a bruised calf rarely has serious consequences for a person, since this area of the body is highly resistant to mechanical stress. But often pathological changes after injury are observed not only in soft tissues, but also in blood vessels and nerve endings.
Important! Treatment of a bruised calf muscle must be timely - otherwise its fibers become vulnerable, the leg cannot bear the load, and is susceptible to various inflammatory diseases.
Calf pain: differential diagnosis
Pain in the calf muscle (calf) is a universal symptom that can occur with a large number of diseases.
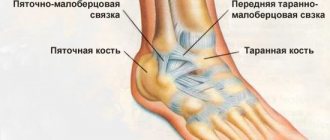
The main muscle mass of the posterior surface of the leg (calf) is formed by two muscles - the superficially located gastrocnemius muscle and the more deeply located soleus muscle. The tendons of these muscles come together and attach to the heel bone, forming the so-called. Achilles tendon. The calf muscles provide movement in the ankle joint (flexion and extension), which is necessary for walking, maintaining body balance in an upright position and shock absorption during movements. The arterial blood supply to the gastrocnemius muscle comes from its own arteries, originating from the popliteal artery. Venous outflow is carried out through the veins accompanying the arteries, which in the thickness of the muscle form wide cavities lined with endothelium - sural sinuses. The above muscles are innervated from the tibial nerve (L3-4).
Chronic venous insufficiency.
Today, in the genesis of pain in chronic venous diseases, three main components are distinguished: distensional, ischemic and inflammatory.
The distension component occurs due to overstretching of the venous wall by excess blood when the mechanisms of its outflow are disrupted. Such disorders may be a consequence of dysfunction of the muscular-venous pump, which plays a leading role in ensuring venous outflow in the vertical position of the body. Stagnation of blood in the veins of the leg can occur as a result of decreased activity of the calf muscles, for example, due to prolonged stay in a stationary vertical or sitting position, as a result of damage to the valve apparatus of the superficial (varicose veins) or deep (post-thrombotic syndrome) veins, which is accompanied by a disruption of the normal centripetal movement of blood and its throwing into the distal sections with each muscle contraction (reflux), as well as with damage to the corresponding muscles and adjacent joints. Such pain often occurs after prolonged static loads and is easily relieved by night rest and/or by placing the limbs in an elevated position.
The inflammatory component is a reflection of the currently generally accepted concept of leukocyte aggression as a leading component in the pathogenesis of chronic venous diseases. Its essence lies in the fact that when the speed of venous outflow decreases and signs of venous stasis appear in the veins of the leg, leukocyte-endothelial interaction occurs with the expression of corresponding adhesive molecules on the cell surface, which leads to the migration of white blood cells into the thickness of the vascular wall and their degranulation. Released oxygen free radicals, proteolytic enzymes and cytokines not only have a damaging effect on the structural components of the venous wall, primarily the collagen framework, but also activate non-myelin C-nociceptors, which are responsible for transmitting the pain impulse. Thus, the inflammatory component of venous pain reflects not only stagnation of blood in the veins of the leg, but also the process of active development of chronic venous diseases, which can ultimately lead to the appearance of varicose veins. The addition of an inflammatory component makes venous pain more persistent and not relieved by elevated position of the limb and night rest.
The ischemic component is associated with severe inflammatory changes in the venous wall with desolation of the vasa vasorum, which leads to serious morphological restructuring of the affected veins. It should be assumed that the ischemic component occurs in severe forms of chronic venous diseases and can cause constant pain in the varicose nodes themselves.
Classic pain in venous insufficiency is dull, arching in nature, intensifies after a long stay in a standing or sitting position, decreases or disappears completely after an overnight rest or placing the limb in an elevated position. Often the pain is accompanied by transient swelling of the soft tissues in the lower third of the leg and cramps of the calf muscle at night.
Acute venous insufficiency – deep vein thrombosis of the leg. As a result of a sudden difficulty in venous outflow from the lower extremities and the development of acute venous congestion, very intense constant bursting pain in the calf muscle can be observed, slightly decreasing when the limb is elevated, accompanied by an increase in the volume of the muscle and its thickening, cyanosis of the skin and an increase in the subcutaneous vascular pattern. The severity of symptoms will depend on the location of the thrombosis - the more veins are involved in the process, the more acute the manifestations will be. With isolated thrombosis of the sural sinuses, moderate intensity, clearly localized pain may be observed, intensifying with plantar flexion of the ankle joint and with pressure on the site of the sinus projection on the skin.
Chronic arterial insufficiency develops as a result of occlusion of the arteries by an atherosclerotic or autoimmune-inflammatory process. In such cases, the muscles experience oxygen starvation and switch to the anaerobic metabolic pathway, which leads to the accumulation of acidic products that irritate pain receptors. In case of arterial insufficiency, pain in the calf muscles is observed when walking and forces the person to stop (intermittent claudication syndrome); in the initial stages of the process, pain does not bother them at rest. The pain is accompanied by coldness of the extremities, chilliness, the skin becomes pale, flaky, easily vulnerable, and hair loss. As the disease progresses, the muscles and subcutaneous tissue become thinner.
Acute arterial insufficiency - sudden blockage of the arteries due to thrombosis or embolism leads to acute ischemia of the limb. In this case, pain in the calf muscle will be observed at rest, be intense, accompanied by disturbances in sensitivity and motor function, up to the development of paralysis and muscle contracture.
Osteochondrosis of the lumbar spine (radicular syndrome) is the second most common cause of pain in the calf muscles. It is based on compression of the spinal nerve root at its exit from the spinal canal. As a result, projected pain occurs in the place where the nerve fibers go - including in the calf area. In this case, pain can be associated both with compression of the nerves and the generation of pain impulses in them, and with tonic muscle contraction and the subsequent development of fibro-dystrophic changes in muscle tissue. With radicular syndrome, pain is associated with certain movements and changes in body position (for example, bending the torso forward, to the sides, flexing a limb at the hip joint). As a rule, pain intensifies with prolonged stay in the provoking position and decreases after warm-up, physical therapy, massage, and thermal effects. With muscular-tonic syndrome, it is possible to detect areas of increased tone in the water of dense, painful foci in the jejunum of the muscle. Over time, the muscle may become diffusely denser due to the development of fibrotic changes in it. Subsequently, due to a violation of the autonomic innervation, a congestive (vasodilation) or ischemic (vasoconstriction) component of the pain syndrome may occur.
Peripheral polyneuropathy can be a complication of diabetes mellitus, a consequence of the toxic effects of ethyl alcohol on the body, etc. Diabetic polyneuropathy is characterized by a combination of night or morning pain at rest, localized in the distal parts of the lower extremities, with crawling sensations, burning, numbness, muscle weakness and decreased skin and (primarily) vibration sensitivity. In this case, the pain can be very intense. Damage to the autonomic nerves can lead to trophic disorders and the addition of the vascular component of the pain syndrome. Neuritis of the tibial nerve is characterized by paroxysmal pain that occurs along the nerve fibers. In this case, in the intervals between attacks, pain is completely absent.
The pathology of the knee joints - primarily osteoarthritis - is characterized by pain in the periarticular area during exercise. The pain is localized mainly in the area of the anterior and inner surfaces of the knee joint, and intensifies with prolonged stay in an upright position of the body, with long walking. Particularly characteristic is increased pain when climbing and especially descending stairs. In the initial stages of the disease, the pain completely disappears with rest (there is no need to elevate the limb). With the development of active inflammation, pain may appear at the beginning of movement and morning stiffness in the joints. During the development of the disease, it is possible that a muscular-tonic component of the pain syndrome may occur, in which the calf muscle is in constant tension and becomes dense and painful on palpation. When effusion accumulates in the joint cavity, limited accumulations can form in the inversions of the joint capsule - Becker cysts, which can aggravate the pain syndrome, compress nerves and veins with the development of a neuropathic and vascular component.
Dermatomyositis, polymyositis is an autoimmune inflammation of muscle tissue, characterized by constant dull persistent pain, aggravated by movements in the ankle joint, combined with muscle weakness and symptoms of intoxication. The muscles become swollen, painful on palpation; over time, they may become thickened, heaviness, nodularity, fibrosis, the formation of calcifications, up to complete atrophy. In autoimmune diseases, as a rule, lesions of other organs and systems, primarily the skin, are detected: erythema and swelling of the periorbital area, scaly erythema of the fingers and hands, redness of the periungual ridges, foci of hyperpigmentation-depigmentation of the skin - with dermatomyositis; swelling-induration-atrophy of the skin in scleroderma, erythema on the face, damage to the kidneys, heart in lupus, etc. Meanwhile, damage to the calf muscles in autoimmune myositis is uncommon.
Myositis can also be a manifestation of cancer, parasitic diseases (trichinosis, toxoplasmosis, cysticercosis) or be a complication of a cold, injury or overstrain of the calf muscle.
Fibromyalgia , a chronic autoimmune disease of muscle tissue, is rarely accompanied by isolated pain in the calf muscles. Intense constant pain and severe muscle weakness in the proximal muscles of the limb girdles are more often observed. There is also prolonged morning stiffness and pain in specific points upon palpation.
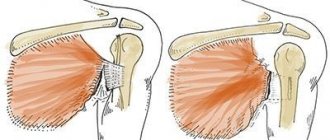
Overstrain, sprain, or muscle rupture can be accompanied by severe intense pain in the damaged area, which sharply intensifies when attempting to move. Inflammatory phenomena (myositis) may occur.
Causes of pathology
Athletes involved in gymnastics, track and field, football, contact sports, and long jump are at risk of getting a bruised calf muscle more often than other people. A direct blow or fall on a limb during such activities is not uncommon.
Athletes often ignore proper treatment and continue to exercise with a similar injury, which only increases pain and swelling of the leg, causing the risk of complications.
Bruising of muscle fibers can happen to a person in everyday life - during a domestic injury, a fall from a height, during a fall on ice, after an injury at work. Often, a bruise from various types of falls is accompanied by a calf strain, which is a partial rupture of the attaching fibers that attach the muscle to the tendon.
Who is more susceptible to calf muscle injury? Risk factors:
- regular exercise without warming up;
- too intense physical activity, constant muscle strain;
- working in a position that is unnatural for the muscles of the limbs.
Signs of a calf muscle injury
If the damage in a place such as the calf is mild, it only slightly disrupts blood microcirculation. First, spasms of small vessels in the bruised area occur, then they expand sharply. Due to a violation of the integrity of the capillaries and an increase in the permeability of their walls, the tissues become saturated with stagnant fluid. After a few minutes or hours, swelling may be noticeable at the site of injury.
Rupture of blood vessels causes bleeding under the skin or into the thickness of the muscle, and the larger the affected vessel, the more serious the bleeding. Multiple damage to blood vessels leads to the appearance of a hematoma (bruise) after some time, which can be present for up to 10–20 days or more. Pain in uncomplicated cases is usually moderate, but as swelling progresses it can intensify.
A strong blow to the leg causes more serious consequences. A muscle rupture is possible, and its symptoms appear immediately as they occur:
- feeling of a strong blow to the back of the leg;
- sharp, severe pain;
- sensation of popping, tearing in the leg;
- rapid appearance of bruising;
- limitation of limb mobility;
- lameness;
- pain when trying to stand on your leg.
Another possible complication that can occur with a powerful blow to the leg is crushing of soft tissues. This causes bleeding, inflammation and death of the affected fibers. The bruise from such an injury is deep, large, painful and may not go away for months.
Reasons why bruises often appear on the legs
The appearance of bruises on the legs without a blow or injury is an alarming sign indicating health problems. Most often they occur suddenly and may be accompanied by bruising. In this case, you should not delay a visit to the doctor, since if the blood vessels are in normal condition without injury, hemorrhage does not occur in the upper layers of the skin. In case of injuries, they can remain on the legs for quite a long time and this is a type of norm that does not require special treatment.
Among them may be:
- Vitamin deficiency, in which due to a lack of vitamins C, K, P, the elasticity of the walls of blood vessels decreases and their fragility increases. If you adjust the menu and replenish it with rose hips, black currants, chokeberries, then the lack of vitamins can be compensated. Most often, such bruises appear in the spring, when the manifestations of vitamin deficiency are most severe.
- Reduced strength of the connective tissue that protects the capillaries. In this case, the appearance of bruises on the legs without a contusion becomes possible with the slightest pressure. This needs to be diagnosed (which is only possible in a specialized center). If the diagnosis is established, sometimes the fragility of blood vessels can be eliminated by taking special medications.
- Lack of platelets, in other words, a blood disease in which there are problems with blood clotting. The localization of bruises is not limited to the legs alone; they also appear on other parts of the body.
- Varicose veins, which not only cause bruising, but also spider veins. The appearance of bruises in this case may be accompanied by a feeling of heaviness in the legs, swelling, and bloating of the veins. As a treatment, the doctor will prescribe you: taking special medications that increase the tone of the veins; sclerotherapy (bonding of blood vessels through subcutaneous administration of drugs); wearing special knitwear that maintains muscle and vein tone).
- Hemorrhagic vasculitis. The reason for the appearance of this disease lies in the fact that the immune system fails and the cells of the blood vessels are perceived as foreign. The IS begins to produce antibodies that destroy the walls of blood vessels. This leads to inflammation, and as a result, the appearance of hematomas.
- Yellow bruises may indicate ruptured blood vessels. This is typical for people actively involved in sports. Under heavy load, capillaries under the skin of the extremities inevitably burst. As a result, bruises appear. Therefore, if after a fitness class your legs hurt a lot and bruises appear, we recommend reducing the level of stress during training.
- The appearance of bruises on the body may be a consequence of developing diabetes, because contrary to popular belief, this disease does not only affect blood sugar levels. Diabetes causes a metabolic disorder that affects blood circulation. Bruises appear, seemingly for no apparent reason, because the vessels become more fragile and brittle, and blood clotting worsens.
- Another reason for the appearance of bruises under the knee at the back, most often is a tendon sprain, varicose veins or internal arterial thrombosis.
- Also, if bruises appear on their own, seemingly for no apparent reason, this may be a reaction to the use of analgesics, antidepressants and anti-inflammatory drugs. The fact is that the components of these drugs reduce blood viscosity, which in turn leads to the appearance of hematomas.
You should start by diagnosing the causes, for which you should visit a phlebologist to rule out problems with the blood. If many small bruises appear on the body, we are talking about a blood disease. By taking tests, the number of platelets in the blood is determined and if a deficiency is detected, appropriate treatment is prescribed. If everything is normal according to hematology, you cannot do without examining the blood vessels to find out why bruises often appear on the body and legs: on the foot, on the inside of the thigh, on the knees, on the calves.
As preventive measures, it is advisable (even in the absence of problems with blood vessels) to wear comfortable shoes, dose physical activity, avoiding stagnation on the one hand, but also without straining it excessively, on the other, adjusting the diet. At the first signs of varicose veins, it would be a good idea to take special medications that strengthen the walls of blood vessels, but only a specialist can say about the advisability of taking them, as well as recommend a specific drug and its dosage. And then the problem that women often develop bruises on their legs for no reason will not bother you.
At the Antireflux phlebological center, our specialists will help you identify the true causes of bruises on your legs and body. After conducting the necessary tests and diagnostic studies, the necessary medications and treatment regimen will be selected according to the cause of the bruises.
Watch our video about why bruises can form for no reason:
What should the victim do?
It is advisable to seek help from a doctor as soon as possible - to a clinic or emergency room. A mild bruise of the calf muscle can be treated at home without contacting a specialist, however, making a diagnosis on your own is problematic. In some cases, it will be necessary to perform an ultrasound or MRI of soft tissues if there is a suspicion of compression of blood vessels and nerve trunks.
A person’s actions in case of injury should be as follows:
- Provide complete rest for the injured leg, put it in an elevated position to improve blood flow (the ideal option is to keep the leg like this for about a day).
- Do not try to stand on your sore leg, do not jump, do not run, do not play sports.
- Apply a cold compress to your leg - a bubble or bottle with cold water, ice in a bag, etc. Hold the compress for 10 - 15 minutes, repeat the procedure 4 times a day.
Important! You cannot warm your leg for 3 to 5 days after the injury!
How to treat a calf bruise
Treatment of a bruised calf muscle with cold in the first hours after injury can reduce hemorrhage in the tissue. A pressure bandage made of an elastic bandage helps a lot, which will prevent severe swelling from appearing, but you should not put too much pressure on the limb.
If the hemorrhage under the skin is significant, it is necessary to pump out the clotted blood, which is achieved by puncture. From the fifth day, physiotherapy (UHF, heat compresses, baths) is recommended.
You should walk on crutches during the recovery period. Surgical treatment is prescribed for large foci of hemorrhage and consists of opening the hematoma, draining the cavity and suturing the incision.
The following medications are used to treat bruises:
- Novocaine for blockades - for severe muscle pain;
- oil solutions for making absorbable dressings;
- non-steroidal anti-inflammatory drugs in tablets, injections, ointments to reduce swelling, pain, inflammation.
First aid for bruises
Timely and correct first aid measures taken in the first 24 hours after an injury will help to recover faster, cope with pain and reduce the consequences of the injury.
What to do if you are injured[1]:
- assess the condition, make sure there are no serious injuries - dislocations or fractures of the limbs;
- ensure rest, as physical activity on the injured arm or leg can aggravate the situation;
- cool the injury site with ice or a cold compress - this will help reduce pain, reduce swelling, and prevent bruising;
- if necessary, you can apply a compression bandage;
- if the bruise is extensive and accompanied by significant swelling, and the bruise is located on the arm or leg, then to facilitate the outflow of blood and lymph from the affected area, it is worth raising the limb above the level of the head while resting;
- use non-steroidal anti-inflammatory drugs in the form of gels, ointments or creams to reduce pain and swelling.
A bruise can have serious health consequences, so regardless of the severity of the injury, you should consult a doctor.
article 2
Rehabilitation
Rehabilitation after a bruise can take a long time:
- for serious injuries - up to 8 weeks;
- for mild cases - up to 1 - 2 weeks.
After the pain subsides (from about 10-12 days), you need to start massaging the muscle with movements from bottom to top, gradually stretching the leg. Stretching exercises last no more than 1 to 5 minutes and are performed very carefully.
With the right approach, recovery will be complete, and the damaged leg will not make itself felt in the future due to overload and sports training.