It is best to use folk remedies for treating osteomyelitis with the consent and supervision of the attending physician. Since this is a serious disease characterized by inflammation of the bone marrow, the consequences may be different. Against the background of overwork, hypothermia or injury, harmful microorganisms are activated, causing inflammatory processes.
Traditional recipes will help relieve symptoms.
Causes of osteomyelitis
Osteomyelitis is an inflammatory lesion of all bone structures and adjacent tissues.
Typically, this pathological process is accompanied by osteolysis and osteonecrosis. The bone softens and gradually breaks down due to infection with subsequent disruption of the blood supply to it, which is called osteolysis. Due to the same disruption of blood supply, osteonecrosis develops, that is, the death of bone cells. Among the causes of osteomyelitis, several groups can be distinguished:
- traumatic - fractures, dislocations or other lesions in the anamnesis that contributed to damage to blood vessels and disruption of blood supply in a specific area of the bone;
- socio-economic - a low standard of living is accompanied by the risk of addiction to bad habits; representatives of marginalized communities are at greater risk of encountering bone injuries, inappropriate treatment, and subsequent infection of wounds;
- Corticosteroid hormone therapy - these drugs can be used to treat a wide variety of diseases and some studies indicate a relationship between their long-term use and osteonecrosis;
- the presence of concomitant diseases, in particular blood diseases.
The reasons for the transition of an acute inflammatory process of bone into a chronic form are:
- errors in treatment (prescribing antibiotics without determining sensitivity),
- early discontinuation of antibiotics,
- late osteoperforation,
- lack of comprehensive treatment,
- poor drainage,
- exhaustion of the body due to concomitant diseases,
- colds.
Clinical observations show that chronic foci of infection in the tonsils, carious teeth, urinary tract, genitals are factors that provoke hematogenous osteomyelitis, especially with injuries, hypothermia, overwork, exhaustion of the body and vitamin deficiency.
There are hematogenous osteomyelitis, in which microbes enter the bone marrow through the bloodstream from an inflammatory focus in the body, and traumatic osteomyelitis, which occurs with open fractures, gunshot injuries, and purulent bone injuries.
The causative agent of osteomyelitis is Staphylococcus aureus, less often - Streptococcus, Proteus, Pseudomonas aeruginosa, etc.
According to the clinical course, they are distinguished:
- acute osteomyelitis (usually of hematogenous origin),
- chronic osteomyelitis:
- primary chronic,
- secondary chronic - a consequence of acute hematogenous osteomyelitis, a purulent bone wound with open gunshot fractures due to inadequate primary treatment of the wound or errors in treatment; less often develops against the background of a serious patient’s condition with significant suppression of the immune system.
Acute hematogenous osteomyelitis occurs mainly in childhood and adolescence, that is, it is a disease of a growing organism. Microflora from an obvious focus of infection (umbilical sepsis, pyoderma, abrasions, wound, boil, carbuncle, phlegmon, erysipelas) or hidden latent infection (chronic tonsillitis, chronic inflammation of the urinary tract, carious teeth, etc.) is carried by the blood flow into long tubular bones. The area of risk is the area of the metaphyses, where there is a wide branched network of vessels and slow blood flow, and the sinuses of the epiphyses. Studies have shown that in the epiphyses and metaphyses there are no terminal vessels, but there is a wide vascular network of anastomosis with diaphyseal vessels, therefore the embolic theory of the pathogenesis of hematogenous osteomyelitis has lost its validity.
Studies by other scientists have shown that microbes from the sinuses, where they settle (especially in osteoporosis), penetrate into the perivascular spaces, where inflammation begins. There is swelling, purulent infiltration around the vessels, fiber, osteon canal system (Haversian canals) of a certain area of the bone. The filling process occurs in a closed space with strong walls, which leads to a rapid increase in intraosseous pressure, which blocks first the venous and then the arterial network with the development of ischemic necrosis and the progression of the purulent-necrotic process in the bone. Consequently, in osteomyelitis, osteonecrosis does not occur as a result of embolization of the vascular network, but as a result of extravascular occlusion through compression of the vessels by the inflammatory infiltrate in the extravascular tissue. Intravascular processes are secondary.
Circulatory disorders in osteomyelitis are generalized. Pain indicates an increase in intraosseous pressure. With osteomyelitis, intraosseous pressure increases 4-5 times compared to normal. The pain disappears immediately after decompression perforations are applied to the bone. Experimental studies have shown that long-term administration of a foreign protein leads to venous stasis, increased exudation, and swelling of the tissue, which in total causes intraosseous hypertension and creates conditions for the sedimentation of microbes in the bone with the subsequent development of the inflammatory process - osteomyelitis. Pathomorphological changes in hematogenous osteomyelitis occur in the bone marrow, around the vessels in the osteon canals, hips, bone tissue, adjacent soft tissues, and joints. Most often, the focus of inflammation occurs in the metaphysis and begins with swelling of the bone marrow, compression of blood vessels, and slowing down the speed of blood flow. Compression of the veins leads to expansion of the arterial network of capillaries, releasing blood elements into the perivascular space. Degeneration and decay of bone marrow cells occurs, intraosseous pressure increases, intraosseous circulation is disrupted, and osteoporosis increases.
Sometimes total bone necrosis occurs. The periosteum thickens and peels off with pus that has penetrated from the medullary canal. Gradually, the periosteum is destroyed, and pus comes out into the adjacent soft tissues, necrosis, thrombus, arteritis with vascular wall urination occur, and bleeding develops. From the metaphysis, the inflammatory process penetrates into the epiphysis, and pus through the lymphatic vessels, destroying the cartilage, penetrates into the joint cavity. Purulent arthritis occurs.
It is characteristic of hematogenous osteomyelitis that, simultaneously with inflammatory, necrotic, degenerative processes, active reparative processes occur: replacement of the necrosis focus with young connective tissue, newly formed vessels, followed by the appearance of osteoblasts from the inner layers of the periosteum, bone marrow, which differentiate and form young bone tissue.
In a third of cases, the acute process turns into subacute and chronic with the formation of a focus of bone destruction and sequestration.
Clinical manifestations of osteomyelitis:
- typical for the disease is seasonality, namely the transition period from summer to autumn-winter and from winter to spring-summer, when weather instability, frequent colds, decreased protective properties of the body, vitamin deficiency, and increased sensitization are noted;
- Mostly children, young people, and young people get sick;
- often the disease begins with a prodrome - the patient complains of weakness, children lose their liveliness, become capricious, their appetite worsens, evening chills and heavy sweats occur;
- in the vast majority of cases, the onset of the disease is acute, reminiscent of an acute general infection - chills, high body temperature occur, young children often experience confusion, rapid pulse, low blood pressure;
- in the case of a toxic form, death may occur within the first days, as with septic shock;
- The patient's face is hyperemic, petechiae or a rash appear on the skin, breathing quickens and becomes shallow.
Hematogenous osteomyelitis can be isolated or multiple (affecting several bones):
- the onset is acute, body temperature reaches 39 °C,
- there are no flushing sweats, and chills are not so intense and frequent,
- there are no manifestations of irritation of the central nervous system;
- severe bursting pain occurs in the affected bone;
- the face turns pale, the lips are cyanotic, the tongue is coated, dry,
- headache, general weakness, tachycardia, tachypnea increase, appetite disappears.
Clinically, after the acute manifestations of osteomyelitis subside, the patient’s condition almost normalizes, and the symptoms of inflammation disappear. But over time, as a result of hypothermia, colds, injuries, malnutrition, inflammatory diseases of the genitourinary system, increasing pain, swelling, redness of the skin, pain on palpation again appear at the site of bone damage, body temperature rises to 38 ° C, leukocytosis increases in the blood, ESR increases, fistulas often open with the release of pus. Often small sequestra emerge from purulent fistulas.
Traumatic osteomyelitis is a complication of an infected wound with open, gunshot fractures or a postoperative complication.
Among the microflora that leads to traumatic osteomyelitis, Proteus, staphylococcus, streptococcus and Pseudomonas aeruginosa are most often isolated (about 54% of cases). In the clinical course, acute, subacute and chronic (purulent-necrotic) osteomyelitis is distinguished, which can have the following phases:
- active with the presence of a fistula;
- exacerbation phase with pronounced signs of local or general inflammation;
- phase of attenuation, stable remission (absence of fistulas and manifestations of a purulent-inflammatory process).
With traumatic osteomyelitis around the focus of bone inflammation, significant changes occur in the adjacent soft tissues, namely fistulas, ulcers with or without bone exposure, the presence of a soft tissue defect (purulent-necrotic wound), the bottom of which is bone, and, finally, a trophic ulcer .
Clinical patterns of the condition of wounds and open fractures indicate that after correctly performed primary surgical treatment on the third day, the patient’s condition improves - body temperature decreases, swelling decreases, there is minor bleeding, leukocytosis also decreases, and there is no tendency to increase ESR. There is no throbbing pain in the area of damage, and gradually the pain subsides altogether. On the 10-12th day the wound heals.
The acute stage of osteomyelitis lasts more than 2-3 months, then it becomes subacute. The patient's general condition improves, body temperature decreases, chills and pain disappear, soft tissue swelling decreases, and appetite appears. The wound is cleaned, granulated, epithelized along the periphery, and reduced in size. A fistula with moderate purulent or serous-purulent discharge is formed.
The radiograph shows the demarcation of the pathological focus, periosteal layers, and formed sequesters. Spongy sequesters partially resolve. If the process in the bone does not subside within 4-6 months, osteomyelitis enters the chronic stage.
Diagnostic methods
Already during the initial examination and studying the patient’s complaints, the doctor can make a preliminary conclusion about the state of his health. But accurate information can only be obtained after a full diagnosis. It includes the following methods:
- a detailed laboratory blood test - clearly shows signs of an acute inflammatory process;
- radiography - turns out to be informative only at the end of the second week of the disease, when pathological changes can be noticed in the bone tissue;
- radioisotope scanning - carried out at the initial stages of the disease;
- MRI or CT scan is performed according to indications to clarify the diagnosis.
In general, it is not difficult to identify a disease with a complete, properly organized diagnosis. The main thing is to choose an effective treatment for osteomyelitis and start it as early as possible, eliminating the likelihood of complications.
How to treat osteomyelitis?
Treatment of osteomyelitis should be undertaken as early as possible, preferably from the first hours of the disease - this will ensure the best consequences.
Having discovered hematogenous osteomyelitis, broad-spectrum antibiotics (for example, gentamicin, mefoxine, kanamycin) are immediately prescribed. Depending on the severity of the disease and the patient’s condition, antibiotics are administered intraarterially, intravenously, intramuscularly and intraosseously. When carrying out antibiotic therapy, prevention of candidomycosis is mandatory.
In addition to antibiotic therapy, in the first days after diagnosis it is necessary to perform osteoperforation of the bone at the site of the lesion. Osteoperforation is done with a spectrodrill or a triangular awl with the obligatory opening of the medullary canal. Osteoperforation ensures the outflow of pus, reduces intraosseous pressure, this in turn reduces disturbances in the vascular network of the bone and localizes the lesion. In recent years, osteoperforation has been performed with laser beams. The technique is simpler, gentle, and has significant bactericidal and hemostatic properties.
Immobilization of the limb is mandatory. In addition, compresses with a 30-50% dimexide solution are applied to the area of the inflamed bone, which is placed on the skin lubricated with antibiotic ointment or hydrocortisone or heparin ointment.
Antibiotic therapy and osteoperforation are carried out against the background of increased body resistance. To do this, active immunization is prescribed with vaccines, staphylococcal toxoid, hyperimmune staphylococcal gamma globulin, and antistaphylococcal plasma. In case of increasing anemia, blood is transfused from donors who have been previously immunized with staphylococcal toxoid.
Vitamin therapy and proteolytic enzymes are widely used in treatment. To reduce intoxication, low molecular weight dextrans, protein preparations, and infusion therapy are prescribed, taking into account the need to normalize the water-electrolyte balance and acid-base state.
Thanks to timely complex pathogenetic treatment, more than 92% of patients with hematogenous osteomyelitis recover.
Treatment of chronic osteomyelitis is exclusively surgical. Before the operation, fistulography must be done to identify the fistula tracts and leaks that need to be cut out. After this, using chisels or cutters, the sequestral box is opened, sequestration and pathological granulation tissue are removed. The branches of the sequestral box are refreshed, given a scaphoid shape and packed with bone grafts preserved at low temperatures with antibiotics. The wound is sutured with mandatory drainage.
When the entire perimeter of the bone is affected, resection of the affected area is performed, a bone osteotomy is made proximal or distal to the resection site, a compression-distraction device is applied, and the free graft is gradually pulled up to the distal or proximal fragments. A bone callus appears, filling the defect with new healthy bone tissue.
Despite the achievements of antibacterial therapy, solving the problem of treating chronic bone osteomyelitis remains one of the difficult tasks. Treatment of patients with chronic osteomyelitis should be carried out comprehensively, based on the general condition of the patient, concomitant diseases, age, condition of soft tissues, and the nature of bone damage. In chronic osteomyelitis, there is always a bone wound and the bone cavity festers, their walls do not collapse, the inner surface of the walls is necrotic with signs of inflammation. The cavity is always filled with varying amounts of pus, pathological granulations, and sequesters. Adjacent soft tissues are infiltrated, with the presence of one or more fistulas.
Such a bone wound does not have the conditions for self-healing, but only contributes to the deterioration of the patient’s general condition and suppression of the immune system. In addition, with frequent colds and hypothermia, relapses and exacerbations of the pathological process constantly occur. Considering this, the main method of treatment is surgery. It consists of total removal of pathologically affected bone and soft tissues.
Methods of surgical intervention
The most common surgical treatment option is opening the lesion to drain the purulent masses and wash the tissues with antibacterial, antiseptic solutions. This makes it possible to alleviate the patient’s general condition, minimize the risks of the spread of pathological fluid throughout the body, and increase the effectiveness of drug therapy.
In difficult situations or in chronic cases of the disease, doctors can remove part of the bone tissue with all subsequent procedures that are provided for such cases as part of surgical treatment. This includes washing the cavity with special solutions, performing bone grafting, and installing drainage. Also during the recovery stage, maintenance drug therapy is carried out.
The operations are performed under general anesthesia.
What diseases can it be associated with?
Osteomyelitis can occur against the background of the following diseases and disorders:
- osteoporosis,
- decompression sickness,
- sickle cell anemia,
- myeloproliferative diseases,
- Gaucher disease,
- systemic lupus erythematosus,
- Crohn's disease,
- thrombosis,
- arterial embolism and vasculitis,
- furunculosis, carbunculosis.
Also, the basis of osteomyelitis is the factor of trauma. But not every damage to bone integrity results in osteomyelitis. For the development of the disease, two factors are necessary - severe infection of the wound and damage to the blood supply in the damaged area, which the listed diseases only contribute to.
Hematogenous osteomyelitis becomes a trigger for the occurrence of such severe complications as sepsis, metastatic abscesses in the lungs, liver, pleura, and kidneys. Complications of hematogenous osteomyelitis also include pathological fractures and dislocations as a result of destruction of the articular ends.
Complications of chronic post-traumatic osteomyelitis:
- amyloidosis,
- bone deformities,
- stiffness and ankylosis of joints,
- pathological fractures,
- malignancy of fistula walls.
Sunbathing
The most effective morning procedures.
If the season allows, then additional therapy in the fight against osteomyelitis will be warming the affected part of the body with solar heat. You must stay in the sun until 10 a.m., exposing the open wound to the rays. The procedure time should be 10 minutes, the duration can be gradually increased. Preventive baths have an analgesic effect in osteomyelitis.
What drugs are used to treat osteomyelitis?
For the treatment of osteomyelitis, among other things, the following are used:
- broad spectrum antibiotics
- gentamicin,
- mefoxine,
- kanamycin;
- neohemodesis,
- rheopolyglucin,
- neocompensan;
- native plasma,
- protein,
- aminopectides,
- hydrolysine;
Preventive actions
Prevention consists of simple tips, adherence to which will help avoid situations where treatment of osteomyelitis . The main recommendations include:
- taking steps to reduce the likelihood of injury. It is they who often lead to infection of bone tissue and all the ensuing negative consequences;
- compliance with the rules of personal hygiene - helps reduce the risk of viral or bacterial infection entering the body;
- an active lifestyle and proper nutrition to maintain a normal immune system;
- timely and correct treatment of dental diseases to prevent the subsequent spread of pathogens;
- effective fight against bacterial infections when they are detected. With a prolonged course, the risks of the spread of pathogens are much higher;
- taking measures to reduce the likelihood of contracting viral infections. Against their background, in some cases, inflammatory processes can also develop.
Of course, following simple methods and rules of prevention is much easier than undergoing long-term and quite serious treatment for osteomyelitis. Everyone should take proper care of their health, doing everything possible to reduce the risk of any problems.
Which doctors should you contact if you have osteomyelitis?
- Traumatologist
- Surgeon
After the start of treatment, acute general symptoms and symptoms of intoxication are significantly reduced and local symptoms come to the fore, that is, pain in the limb, swelling at the site of bone damage. The patient spares the limb, protects it from movement and fixes it in a half-bent position, in which the antagonist muscles relax and the severity of pain decreases. In the area of edema, increased skin temperature and even superficial palpation cause exacerbation of pain.
Constant pain leads to sleep disturbances.
The intensity of joint pain increases with the accumulation of inflammatory fluid (synovitis) in the joint cavity. During joint puncture, purulent synovial fluid is obtained.
X-ray control allows you to confirm the clinical diagnosis and identify the nature of the osteomyelitic lesion. But it should be remembered that in the case of an acute onset, radiological manifestations in the affected bone can be detected no earlier than 2-3 weeks from the onset of the disease, and their severity depends on the severity of the inflammatory process and the area of bone damage.
At the onset of the disease, radiographs show loss of spongy and cortical bone structures, followed by the formation of a focus of osteoporosis with destruction, over which thickening of the periosteum occurs.
In addition to paraclinical diagnostic methods, a significant place is given to bone puncture, which has not only diagnostic but also therapeutic value, because bone perforation leads to a decrease in intraosseous pressure and a decrease in pain. In case of traumatic osteomyelitis, X-ray examination should be carried out in the dynamics of the disease, since at first there are no destructive changes in the bone structure, but later they arise.
The radiograph shows osteoporosis, increasing necrosis of the ends of fragments, periosteal layers above the fracture site.
Proper nutrition is the key to a quick recovery
Don't lose sight of your diet. Compliance with it is a prerequisite for successful treatment. In general, patients are given basic recommendations:
- fractional meals - eat 5-6 times a day in small portions;
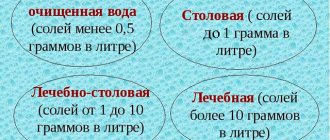
- maintaining water balance - drink about 2.5 liters of fluid per day;
- fortified products. It is recommended to focus on fermented milk products, fruits and vegetables, lean fish and meat. Dishes should be steamed, boiled or baked. Fatty and fried foods should be avoided.
Proper nutrition helps provide the body with the nutrients it needs and gives strength to fight the disease. Therefore, during the therapy process, compliance with the listed points is a prerequisite.
Treatment of other diseases starting with the letter - o
| Treatment of obstructive bronchitis |
| Obesity treatment |
| Treatment of burns of the larynx |
| Treatment of herpes zoster |
| Treatment of adrenal tumors |
| Treatment of tracheal tumors |
| Treatment of ARVI |
| Treatment of orchitis |
| Treatment of osteoarthritis |
| Treatment of osteoma |
| Treatment of osteoporosis |
| Treatment of osteochondrosis |
| Treatment of osteochondropathy |
| Treatment of acute abdomen |
| Treatment of acute intestinal failure |
| Treatment of acute mesenteric ischemia |
| Treatment of acute renal failure |
| Treatment of laryngeal edema |
| Treatment of otitis media |
| Treatment of pityriasis versicolor |
The information is for educational purposes only. Do not self-medicate; For all questions regarding the definition of the disease and methods of its treatment, consult your doctor. EUROLAB is not responsible for the consequences caused by the use of information posted on the portal.
Yolk and honey
To prepare the medicine, use only natural products.
To make a compress you need:
- Prepare 500 g of bee product, 450 g of rye flour and butter, 7 yolks.
- Melt the honey.
- Beat the yolks.
- Add butter and flour.
- Mix all ingredients and form into a flat cake.
- Apply a compress to the affected area, cover with a cloth and bandage.
Healing barberry
The root vegetable has analgesic and anti-inflammatory properties.
It is recommended to treat the disease with the help of barberry. To prepare the decoction you need:
- Take 150 g of barberry root and 1.5 liters of water.
- Peel and cut the root, put it in a saucepan, add a liter of water.
- Cook for 15-20 minutes.
- Remove from heat.
- Leave for 5 hours and strain.
- Take 2 tbsp decoction. l. every day half an hour before meals.
- The course lasts 3 months, with a break of 4 weeks.