If you are concerned about the feeling of pain and stiffness in the sternum along the spine, do not rush to take heart drops, because the cause of this condition may be the development of arthrosis. When it comes to problems in the musculoskeletal system, knee, hip, neck and even lumbar joints immediately come to mind. But in medicine there is another type of such disease that is rare. Its name is arthrosis of the costovertebral joints. The localization of dystrophic changes occurs in the thoracic region, and the disease is the most common cause of pain.
What is arthrosis of the costovertebral joints?
The thoracic region includes 12 vertebrae. In their structure, they differ from the lumbar or cervical ones in that they have a smaller diameter and length. But their spinous processes are somewhat longer. In order for the vertebrae to connect to each other, they need pairs of symmetrical articulations located between these processes. They are called intervertebral, facet or arcuate. Such bone joints are present in all parts of the ridge, except the sacrum and coccyx. In this area the vertebrae are fused together. In the thoracic region they are flat and inactive.
Anatomy of the thoracic spine.
Osteoarthritis of the costovertebral joints is the destruction of cartilage and tendons between the edges of the vertebral articulations, a rare form of osteoarthrosis or spondyloarthrosis. Degenerative changes progress, cartilage and tendons become inflamed, and any friction in the area of inflammation causes pain and stiffness. The most common localization of dystrophic disorders in costovertebral pathology is the 9th and 10th ribs.
Changes in the joints of the spine often lead to disruption of the functionality of the entire musculoskeletal system. And if until recently it was believed that the disease was characteristic of older people, in whom the natural aging processes affect the rate of metabolic reactions, now it also occurs among young people over 30-40 years of age. In men, the risk of developing costovertebral pathologies is 3-5 times higher than in women . Most cases occur between 20 and 35 years of age.
Diagram of blood vessels.
Costovertebral arthrosis develops gradually and goes through several stages. Under the influence of provoking negative factors, the thoracic region of the back is exposed to external influences. In response to the irritant, inflammation occurs in the area of cartilage and tendons. If it repeats, the pathology becomes chronic. A compensatory reaction occurs - the proliferation of connective tissue in the area of dystrophy and the formation of osteophytes. This leads to deterioration in joint mobility and deformation. The process is closed: inflammation provokes deformation, and deformation generates inflammation. The more changes in the joint, the more pronounced the symptoms of the disease become: pain of varying degrees of intensity, limitation of body mobility, the amplitude of which gradually tends to zero.
Arthrosis of the costovertebral joints often manifests itself in the form of synovitis - a recurrent inflammatory process in cartilage and tendons. During an exacerbation, a person experiences pain that prevents movement. During the chronic course, no signs of malaise are noted.
Osteoarthritis of the facet joints
Facet joint syndrome (spondyloarthrosis)
- a disease associated with degeneration and damage to the facet joints, manifested by back pain, usually without neurological disorders. The facet joints have a typical structure and consist of articular cartilage, synovial membrane, synovial fluid and capsule.
Facet joints are formed when the inferior articular process of the overlying vertebra connects with the superior articular process of the underlying vertebra. Each articular process is covered with a layer of hyaline cartilage 2-4 mm thick. This thickness is necessary to withstand heavy loads. The ability of articular cartilage to deform and return the convex-concave shape of the articular surface helps to carry out movements in several planes. The main function of the facet joints is to support and stabilize the spine during all possible movements.
In this case, the intervertebral disc and facet joints at the same level constitute a single spinal motion segment or “three-joint complex.” In this case, the disc accounts for 60-70% of the load, and the joints 15-40%. Degenerative changes in the intervertebral disc lead to increased stress on the facet joints, and conversely, damage to the facet joints can accelerate disc degeneration.
Pathophysiology of the development of pain in lesions of the facet joints.
In the vast majority of cases, damage to the facet joints is the result of many years of repeated trauma associated with a suboptimal range of motion in them and an increase in the load on these joints due to degeneration of the intervertebral discs.
In some cases, damage to the facet joints can develop acutely, for example, with a whiplash injury to the neck or with sports injuries, but basically the process is chronic in nature. With damage to the discs, from which degenerative changes in the spine most often begin, the weight load gradually shifts to the intervertebral joints, reaching from 47 to 70%.
Such overload of the joints leads to successive changes in them: synovitis with the accumulation of synovial fluid between the facets; degeneration of articular cartilage; stretching of the joint capsule and subluxation in them. Aseptic inflammation develops in the affected area with the release of a large number of inflammatory mediators such as interleukin-1, interleukin-6, substance 3 and others. Which enhance inflammatory and degenerative changes. Continued degeneration leads to the development of periarticular fibrosis and the formation of bone outgrowths on the surface of the joint - osteophytes, which increase the size of the upper and lower facets, which become pear-shaped. Eventually, the joints degenerate dramatically, losing almost all cartilage.
Quite often, this process of degeneration occurs asymmetrically, which is manifested by uneven loads on the facet joints. The combination of changes in the disc and facet joints leads to a sharp limitation of movements in the corresponding motion segment of the spine.
Clinical picture.
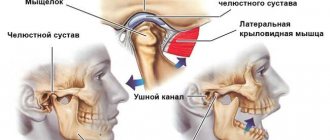
Before moving on to considering the clinical picture of facet joint syndrome, it is necessary to dwell on the features of the innervation of the facet joints (intervertebral joints). The facet joints have a large number of encapsulated and non-encapsulated nerve endings that have proprioceptive (sense of position in space) and nociceptive (pain) sensitivity. Each facet joint and periarticular space is innervated from two or three adjacent levels - ensuring mutual overlap of the spread of pain from adjacent lumbar facet joints. Pain from the L5-S1 joint is reflected in the coccyx, hip joint, back of the thigh, and sometimes in the groin area. Irritation of the L4-L5 joint is characterized by pain radiating from the site of irritation to the buttock, the back of the thigh and hip joint and, only occasionally, to the tailbone. From the L3-L4 joint, pain spreads to the chest area, the lateral surface of the abdomen, the groin, reaches the front surface of the thigh and, very rarely, the tailbone and perineum. Irritation of higher level facet joints (Th12–L1, L1-L2, L2-L3) is limited to the appearance of pain in the upper back and abdomen, thoracic and even cervical regions. Separately, Meijn syndrome is distinguished - a type of facet syndrome with damage to the Th12-L1 intervertebral joint. Dysfunction of this joint leads to the appearance of referred pain in the area of the iliac crest on the affected side.
In facet joint syndrome, pain increases with extension and decreases with flexion. The pain can radiate paravertebrally (near the vertebral column), into the buttock. Referred pain emanating from the intervertebral joints is lateral, diffuse, difficult to localize, sometimes it radiates along the back of the thigh, but never spreads below the popliteal fossa. It is limited to the lumbosacral region above the affected joint, radiating to the gluteal region and upper thigh. Facet pain may be more or less cramping. Characteristic is the appearance of short-term morning stiffness and an increase in pain towards the end of the day. The pain intensifies from prolonged standing, extension, especially if it is combined with bending or rotation to the painful side, when changing body position from lying to sitting and vice versa. Unloading the spine - bending it slightly, taking a sitting position, using support (stand, railing) - reduces pain.
Characteristic signs of pain caused by “facet syndrome” (spondyloarthrosis):
• THE ONset OF PAIN IS ASSOCIATED WITH ROTATION AND EXTENSION OF THE SPINE; • PAIN HAS A LATERAL DIFFUSE CHARACTER; • PAIN DOES NOT RADIATE BELOW THE KNEE JOINT; • MORNING STICKNESS IS CHARACTERISTIC; • THE ONset OF PAIN IS ASSOCIATED WITH ROTATION AND EXTENSION; • PAIN INCREASES IN STATIC POSITIONS; • WARM-UP, UNLOADING THE SPINE REDUCE PAIN.
Treatment of facet joint syndrome
When treating facet syndrome, a multilevel approach is most effective. Heat treatments and relaxing massage in combination with NSAIDs (eg, nimesulide, lornoxicam) and muscle relaxants (eg, mydocalm) are a reasonable start to treatment
.
The next logical step is to inject steroidal anti-inflammatory drugs mixed with local anesthetic intra-articularly or parafacetically. This ensures stable relief of inflammation in the affected area and thereby has a long-lasting therapeutic effect. If the disease progresses and these techniques are ineffective, radiofrequency denervation of the joints is performed. Share this post on social networks:
Types and reasons for its development
Costovertebral arthrosis can be primary or secondary. Classification by form depends on the causes of pathological disorders. Primary arthrosis is characterized by subtle forms of its course, in which it is impossible to determine the cause of the appearance of dystrophic changes. This diagnosis is usually made to older people, in whom the development of disorders is associated with the natural processes of aging.
The nature of the occurrence of secondary type pathology is more or less clear. Causes of the disease:
- inflammatory diseases;
- back injuries and vertebral compression;
- endocrine diseases;
- infections, including tuberculosis;
- genetic factors;
- congenital disorders in the formation of the spine;
- flat feet, as a result of impaired shock absorption of the foot;
- excessive physical activity not related to work;
- poor posture due to a sedentary lifestyle;
- problems with metabolism.
Arthrosis of the costotransverse joints can also develop depending on the condition of the spine itself. It can be provoked by spondylolisthesis, intervertebral hernia, osteochondrosis, spondyloarthrosis and other diseases of the thoracic back.
Forms of the disease
Arthrosis of the lumbar, cervical, and thoracic spine is conventionally divided into two groups:
- primary;
- secondary.
If the disease has developed due to age-related changes, and its root cause has not been established, they speak of primary arthrosis. The development mechanism is associated with degenerative-destructive processes in cartilage tissue, wear of joints and dysfunction of various body systems. If the disorder was preceded by fractures, injuries, acute infectious diseases, hormonal imbalances, osteoarthritis takes a secondary form.
Often the cause of the disease is the inflammatory process occurring in the joint. In some patients, the cartilage located in the sternocostal joints is affected. This disorder is called “Tietze syndrome” and has the character of aseptic inflammation. Tuberculosis can provoke spinal-costal arthrosis. Scientists also note the role of genetic disorders and congenital joint dysplasia.
Diagram of the connection of the ribs with the spinal column and sternum
Symptoms of the disease
The signs of costovertebral pathologies are identical and have common features. A person feels back pain of varying intensity depending on the stage of the disease, which can intensify with external stress. At rest, the patient does not experience discomfort. There is no morning stiffness associated with the disease, except for the starting pain at the beginning of movement. Other signs are slight swelling of the soft tissues and redness of the skin. But more often these symptoms are absent.
As the patient's condition worsens, the symptoms become more pronounced. The pain becomes intense, the limitation of mobility in the joints becomes more severe. Depending on which joints of the sternum are damaged, costal arthrosis differs.
When the bone and cartilage structures between the ribs and vertebrae are destroyed, the following symptoms are characteristic:
- the appearance of pain in the back in the chest area;
- discomfort increases with deep breaths and during movement;
- tissue swelling and pain may be observed in the area of localization of inflammation;
- reflex spasms appear in the spine;
- mobility in the joints gradually deteriorates, which leads to severe pain even when breathing;
- stiffness when moving goes away in a short time;
- During movement, crunching and clicking may occur in the back.
Sometimes costovertebral arthrosis is asymptomatic for some time. It is often possible to find out about the disease by chance, during routine radiography. At first, the signs are mild. However, the clinical picture changes with the progression of the pathology. Symptoms worsen towards the end of the day after prolonged strain on the back, causing fatigue. The inflammation spreads mainly to the joints of the lower chest. Most often this type of pathology is diagnosed in women over 40 years of age.
Inflammation of the connection between the ribs and the sternum is much less common. It mainly develops due to systemic diseases, injuries and infections. Clinical signs of costotransverse arthrosis:
- the appearance of unpleasant sensations along the edge of the sternum;
- severe pain occurs with maximum inspiration;
- inflammation of the costotransverse joints is insignificant;
- upon palpation, slight swelling of soft tissues is noted;
- there are no reflex spasms in the spine;
- stiffness of joint mobility continues for quite a long time.
This type of disease rarely leads to serious deformation of the chest and does not cause severe pain when breathing. The course of the pathology is more favorable than with costovertebral.
Any type of arthrosis negatively affects posture. At rest and during movement, the patient develops a permanently slouched posture, when the shoulders drop and turn forward. In the absence of treatment, dystrophic processes continue to form in the structure of the vertebrae and tendons, destroying the integrity of the osteochondral apparatus. If the disease takes a severe course, the issue of the patient’s ability to work and his further disability is decided.
Joints of the sternum
Joint type Hand joint. In appearance it is similar to a cartilaginous symphyseal joint (limitedly mobile). The xiphoid process joint. Cartilaginous immobile (synchondrotic). Usually ossifies with age.
joint . Between the manubrium and the body of the sternum, located next to the second costal cartilage. The xiphoid process joint. Between the body of the sternum and the xiphoid process. The joint marks the lower border of the thoracic cavity.
Joints of the sternum: front view
Diagnostic methods
To identify arthrosis of the costovertebral joints, various diagnostic methods will be required. This is necessary to identify damage to these joints, which can masquerade as a whole bunch of back diseases. For this purpose, the patient is prescribed the following types of instrumental methods:
- X-ray of the chest in several projections. Makes it possible to detect osteophytes, minor deformations, and indirect signs of inflammation. A specialist can determine pronounced dystrophic disorders without the help of radiography;
- computed tomography is more informative in the initial stages of the disease than radiography;
- Magnetic resonance imaging is the most effective way to detect the disease in the early stages;
The last two methods are not always carried out. This is due to expensive equipment. Not all clinics have sophisticated equipment and the cost of diagnostics is not affordable for all patients.
- Ultrasound examination can detect the phenomenon of synovitis.
Laboratory and clinical tests for costovertebral arthrosis are ineffective and have little impact on them. They are not used for diagnostic purposes.
Diagnostic measures
The first thing the doctor does is clarify the patient’s complaints and collect anamnesis (presence of injuries, back injuries, infectious diseases, heredity, difficult working conditions, etc.). Next, an external examination is carried out, during which moderate swelling of the tissues and redness of the skin in the area of the affected joints can be detected. Instrumental research methods allow you to make an accurate diagnosis, with the help of which you can determine the localization and severity of the pathological process.
X-rays show bone growth
For this purpose the following is carried out:
- radiography in several projections - allows you to identify bone growths, destructive processes and some signs of inflammation;
- Ultrasound – it can be used to detect inflammation of the inner joint membrane (synovitis);
- CT – the method is informative in the early stages;
- MRI is the best diagnostic method at the onset of the disease.
Most often, doctors limit themselves to X-rays, since the last two studies are more difficult to conduct and cost more.
Laboratory tests have no diagnostic value, so they are not usually performed. In the blood test, changes inherent in the course of any disease may be observed, against the background of which secondary arthrosis has developed. Thus, laboratory manifestations of inflammation are an increase in leukocytes and an acceleration of ESR. These signs are not specific.
No ads 3
Methods of treating the disease
Diseases of the musculoskeletal system require an integrated approach. Treatment should be aimed at relieving pain, eliminating the inflammatory focus, restoring tissue, preventing further destruction of joints and tendons. Therapy of costovertebral arthrosis includes the following measures:
- Use of medications.
- Physiotherapy.
- Manual therapy.
- Massage.
- Visiting sanitary and resort institutions.
- Ethnoscience.
Drug treatment
To relieve pain and inflammation in the damaged areas, the patient is prescribed painkillers and non-steroidal anti-inflammatory drugs. Their action is aimed at reducing pain, eliminating inflammation and swelling of tissues. The duration of taking such drugs depends on the stage of the disease, the clinical picture and does not have a negative effect on other organs and systems. Non-steroidal anti-inflammatory drugs can be used at any stage of the disease, but the greatest effectiveness of such therapy is observed when the joint is not yet deformed.
Although the video is about the treatment of osteochondrosis, all the principles outlined are relevant for the topic of this article:
Medicines for external use are widely used for therapeutic purposes. They normalize blood circulation in tissues, improve their nutrition, eliminate inflammation, swelling, and pain. This category includes ointments and gels. The most optimal conditions for the effective use of gels and ointments are the initial and middle stages of the pathology. As soon as the joints begin to undergo dystrophic changes, the result of such treatment is reduced to zero.
For severe muscle spasms, the patient is prescribed muscle relaxants to relieve tension and relax tissue in areas damaged by the disease. Chondroprotectors are used to restore cartilage structures. They contain chondroitin and glucosamine, which in their properties are close to natural joint structures. These medications are designed to strengthen and protect the diseased joint, stimulating its recovery and regeneration.
The use of medications is a symptomatic treatment, which without an integrated approach is not able to completely rid a person of the problem.
Physiotherapy and exercise therapy for costal arthrosis
Physiotherapy and exercise strengthen the muscles of the joints and increase their endurance. They help reduce body weight, thereby reducing the load on the joints. Doing sports and physical activity promote the restoration of cartilage tissue, which helps fight the disease. After physical therapy exercises, the muscles need to relax, so the patient will need massage courses.
Physiotherapeutic techniques for costotransverse arthrosis:
- laser therapy. Under the influence of a laser beam acting on the area of localization of inflammation, it is possible to excise damaged tissue and stop the source of joint destruction. Pain and swelling gradually disappear. To prevent the process from resuming, the patient needs systematic diagnostic monitoring and the use of chondroprotectors;
- magnetotherapy. The technique is similar to laser treatment, except that the operating mechanism in it is a magnet;
- ultrasound and phonophoresis;
- galvanization;
- acupuncture. Refers to manual therapy. This is not enough for complete healing. Used in combination with other technologies.
The greatest therapeutic effect from such techniques is achieved when treating a patient in a sanitary resort environment. This way the patient can take a comprehensive approach to the problem. Methods of manual treatment, herbal and hirudotherapy have not yet been sufficiently studied, and therefore are not recommended as independent therapeutic methods.
Radical treatment methods
When deformations already begin in the joints, conservative medicine is not able to fight arthrosis. The patient is indicated for surgical treatment. In simple cases of deformation and dystrophy, fragments of destroyed cartilage are excised from the damaged joint. After surgery, the inflammatory process can be stopped.
If the degenerative changes are too pronounced, then surgical treatment is carried out by endoprosthetics with the replacement of the deformed bone joint with an artificial one. After radical treatment, a rehabilitation period begins, including medication, physical therapy, diet, and preventive measures.
Possible complications
Any disease without treatment is fraught with the development of serious complications, costovertebral arthrosis is no exception. When faced with an illness, people rarely turn to specialists for help. Instead, they are treated with folk remedies, which is not always justified.
If inflammation of the costotransverse and vertebral joints is not treated, their condition can worsen significantly. Complications include:
- limitation of mobility and functionality of joints;
- compression of nerve fibers, blood vessels supplying tissues with oxygen and nutrients;
- development of chronic diseases of the spine, joint deformities, formation of osteophytes;
- the appearance of pathologies in internal organs.
Based on the symptoms of costovertebral pathologies, the doctor can diagnose lung or heart diseases - the clinical picture of these pathologies is quite similar. This is the insidiousness of the disease. Incorrect diagnosis or incorrectly prescribed treatment are additional reasons for the development of complications in the patient.
How to prevent the development of pathology?
How to prevent the development of arthrosis of the costovertebral joints? Knowing the causes, the development of degenerative disorders can be avoided if you engage in their prevention. The exception is back injuries, which cannot be prevented. To prevent costovertebral arthrosis, doctors recommend physical activity: walking more, cycling, swimming, and including different types of physical activity.
Hula hoop has a good preventative effect. Contrary to all the myths that this device for rotating the body negatively affects the condition of the internal organs, all vertebral cartilage and tendons are perfectly worked out. Blood circulation along the back improves, tissues receive more oxygen and nutrients.
Body weight control also prevents the development of pathological disorders in the joints. It is important to adhere to a special diet so as not to gain weight, but to eat well and in a balanced manner. In case of excessive loads on bone joints in athletes and people whose work involves heavy physical labor, in order to prevent arthrosis, it is necessary to take a reasonable approach to training or loads.
If the first signs appear that are similar in their symptoms to diseases of the bone joints, you should consult a doctor and undergo a full examination. If the diagnosis is confirmed, remember: costotransverse arthrosis is not a death sentence, but a call to action. A set of methods of conservative therapy and physical treatment will help cope with the disease.
Prevention
Preventive recommendations for various diseases of the musculoskeletal system are the same and consist of body weight control, moderate physical activity and proper nutrition. Elderly people should take vitamin and mineral complexes, since the beneficial substances obtained from food will not be enough for them.
The most important rule is a timely examination by a doctor (especially when pain occurs) and undergoing medical examinations. An important place in the prevention of arthrosis is occupied by the detection and timely correction of congenital pathologies of the musculoskeletal system. Patients and people at risk should minimize prolonged mechanical and static loads on the joints.