Gonarthrosis is arthrosis of the knee joint, a chronic non-inflammatory disease manifested by the progressive destruction of intra-articular cartilage, which is accompanied by abnormal formation of the bones that form the joint, changes in the synovial membrane and synovial fluid.
Gonarthrosis is the most common type of arthrosis. Many people experience knee pain, especially after sitting for a long time without moving, such as after a day of work in the office. It is very likely that gonarthrosis is the cause of such discomfort.
This degenerative disease often develops with age, as stress in the knee, which cannot be avoided in various life situations, inevitably leads to wear and tear of the cartilage over the years. At first, a person feels pain when starting to move after long periods of lying or sitting, but this quickly passes. However, as the disease progresses, knee pain increases and begins to significantly limit a person's ability to move normally in daily activities.
In more than half of the cases where arthrosis affects the knee, both knees are affected at once. In the category of patients from 65 to 75 years old, gonarthrosis is detected in 35% of women and 21% of men.
General information about the disease and pathogenesis
Gonarthrosis is a type of arthrosis, a joint lesion that occurs in older people or in young people who endure heavy physical activity.
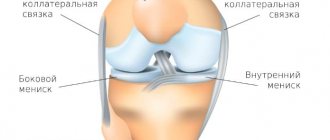
When the joint capsule cannot cope with the increasing load on it, microdamages occur, in the place of which osteophytes grow, leading to a narrowing of the joint space. The disease most often affects large and mobile joints, which bear significant load while walking or running. Example – knee and hip joints, lower back. Gonarthrosis and a healthy joint, comparison
Arthrosis is a common pathology of the musculoskeletal system. More than half of the cases of the disease are associated with damage to the knee joints. Pathological processes in the articular cavity are associated with the following phenomena:
- Due to the disruption of metabolic processes in the cartilage associated with the functioning of the circulatory system, a parallel disturbance of osmotic pressure occurs. An example is that when you squeeze the knee during movement, synovial lubricant is released, and when it relaxes, it is absorbed. When walking, the cartilage plate is constantly nourished, helping to maintain its integrity. If this process is disrupted for some reason, premature or age-related wear of the joint capsule occurs.
- Next, the structure of collagen fibers is disrupted, which causes a loss of shock absorption properties. Against the background of this pathological process, the metabolic function of cartilage cells is disrupted, which significantly slows down the regeneration of cartilage tissue. As a result, the cartilage structure becomes thinner, loses stability and elasticity.
- Against the background of emerging pathological processes, irritation of the synovial membrane subsequently occurs, which leads to the appearance of a chronic inflammatory process. Against the background of long-term inflammation, osteophytes begin to grow, which provokes a decrease in joint mobility.
- Subsequently, there is a gradual destruction of the cartilage with its complete erasure, against the background of which there is a narrowing of the joint space and an increased growth of osteophytes.
Professional athletes and people who work mostly standing all day are more susceptible to this pathology.
Bilateral gonarthrosis can be primary or secondary due to its occurrence. The primary form is not associated with exposure to adverse external factors. In such a situation, bilateral gonarthrosis develops independently, as an age-related degenerative-dystrophic process. Secondary bilateral gonarthrosis of the knee joint is the result of previous bone injuries, substance disorders, cartilage injuries and infections.
Provoking factors
Gonarthrosis is more common in the presence of such unfavorable factors in the patient’s life:
- Metabolic disorders associated with endocrine pathologies (diabetes, obesity, thyroid problems).
- Systemic circulatory disorders, including capillary fragility and varicose veins.
- Increased body weight, which creates additional stress on the knee joints.
- Previous injuries, including torn ligaments, fractures and cracks in bones.
- Previously suffered inflammatory diseases of the joints - arthritis, rheumatism. Typically, arthrosis is already a consequence of inflammatory pathologies in this case.
- Chronic overload of joints associated with excessive loads. Typically, this phenomenon affects athletes involved in running sports - marathon runners and sprinters.
- The presence of serious hormonal disorders.
- A history of chronic knee injuries that do not go away for a long time.
- Heredity.
- The presence of congenital anomalies in the structure of the knee joint.
Persons with bilateral damage to the knee joints respond more severely to therapy, since in this case the possibility of proper movement is seriously impaired.
Causes
In accordance with the reasons for its appearance, it is customary to distinguish two main types of gonarthrosis:
- primary - the cause of its appearance has not yet been established; as a rule, this is bilateral gonarthrosis, which occurs in elderly patients;
- secondary - occurs against the background of an existing injury or pathology of the knee joint at any age; As a rule, this is unilateral gonarthrosis.
In more than 20% of cases, the pathology develops after intra-articular fractures of the tibia, ligament rupture or meniscal deformation. Often gonarthrosis develops 5 years after the onset of the pathology, but in rare cases it appears after 3 months.
The appearance of the disease can be triggered by high load on the joint. People over the age of 40 who regularly work out at the gym are at risk. Excessive stress when performing heavy exercises can lead to degenerative changes. Not only training, but also stress on joints due to excess weight can lead to similar consequences. Therefore, you need to follow a diet and control your body weight. Genetic predisposition often causes gonarthrosis. If a person has weakened ligaments and is susceptible to arthritis, then he is at risk and should avoid excessive stress on the joints.
General signs of gonarthrosis
Arthrosis has a number of classic signs that occur when any joint is affected:
- Feeling stiff and stiff when waking up early.
- The stiffness goes away within an hour of waking up.
- No signs of inflammatory process.
- Discomfort or pain occurs in the knees with the corresponding type of load - climbing stairs or running.
You should also consider the signs of bilateral gonarthrosis, depending on the stage of development. A total of three degrees of the disease are classified.
Symptoms of bilateral gonarthrosis of the 1st degree
The disease develops at first without obvious signs and is almost imperceptible. Most patients rarely notice signs of stage 1 disease. If symptoms appear, they are minor. Occasionally, joint pain appears alternately during physical activity. At the initial stage, the appearance of signs of severe stiffness is not typical.
Usually discomfort occurs when walking for a long time or climbing stairs. If you sit down to rest, the discomfort disappears. In rare cases, patients note slight stiffness in the knees after sleep, which goes away within a few minutes when the person walks.
Gonarthrosis in the picture
A characteristic sign indicating the development of arthrosis is the presence of starting pain, which appears when taking the first steps after waking up. Less commonly, slight swelling is observed, indicating the development of an inflammatory process in the knee joints. Since there is no obvious deformation yet, the swelling goes away on its own. It is impossible to cure bilateral gonarthrosis, since both legs are affected, but in the initial stages of development, degeneration can be slowed down if the pathology is noticed in a timely manner.
Signs of bilateral gonarthrosis of the 2nd degree
At this stage, the manifestations become obvious and painful, so the person already pays attention to them. The pain becomes bright and pronounced, often occurring not only during stress, but also at rest. Discomfort is most often localized in the area of the anterior and posterior thighs. In the morning, there is obvious stiffness and limited range of motion in the joints, so it is difficult to bend the leg. A characteristic crunch also appears. At this stage, most patients consult a doctor for treatment.
It is important to pay attention to pain. If the joint is affected, then with active inflammation there is an accumulation of fluid in the knee area, which is why the first and second legs begin to bend poorly due to discomfort. The swelling resembles a ball in shape, most often they vary in size. When making complex movements (turning the leg to the side or a sharp lunge), pain is observed that is similar in nature to a pain and aching sensation. If bilateral gonarthrosis occurs, it is necessary to improve mobility with the help of drug correction and exercises.
Gonarthrosis 3 degrees
Grade 3 gonarthrosis of the knee joint is a terminal stage and leads to a severe pathological course. Movement is very difficult due to severe stiffness and inflammation in the knees. Since the cartilage is almost completely worn away, there is a strong proliferation of osteophytes and a significant narrowing of the joint space. The lower limbs are also often affected, making it impossible for a person to walk normally. There is severe inflammation, so advanced deforming gonarthrosis leads to severe pain.
Gonarthrosis stage 3
It is possible that a large cartilaginous fragment may appear in the articular cavity at the third stage, called an articular mouse, as a result of which severe pain appears, against the background of which there is an inability to move the limb. There is an almost complete blockade of the joint. If the articular mouse slips back, then the excruciating pain disappears. This form of the disease is treated with surgery.
Diagnostic test
To make an accurate diagnosis, it is necessary to conduct a comprehensive study. If arthrosis is suspected, the patient should consult an orthopedic traumatologist. The doctor must conduct a visual examination, listen to the patient’s complaints and send him for instrumental diagnostics.
Different research methods have different effectiveness, depending on the stage of development of bilateral knee lesions:
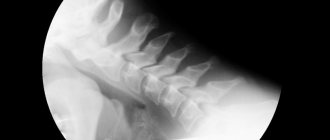
- X-ray examination. This is a basic research diagnostic method. On an x-ray, you can easily see pathological changes at stages 2-3, indicating the development of arthrosis of the knees. X-rays show growth of osteophytes and narrowing of the joint space, which indicates gonarthrosis. If the patient has just begun a destructive process in cartilage, the X-ray machine may not notice minimal changes.
- CT scan. Allows you to identify knee arthrosis at the initial stage of development. This is an improved type of diagnostics of bones and joints. A CT image is a three-dimensional model of an x-ray image.
- Ultrasound diagnostics. This type of study allows us to identify arthrosis at the initial stage and inflammatory processes in tissues, which can also be affected as complications.
- MRI. This study is prescribed if other concomitant diseases are suspected - arthritis, spondyloarthrosis. When performing magnetic resonance imaging, attention should be paid to the presence of inflammatory processes in the periarticular tissues.
It is equally important to carry out laboratory diagnostics in the form of urine and blood tests in order to identify possible concomitant pathologies in the body. What studies are prescribed:
- General blood analysis. Pay attention if the analysis shows an increase in the sedimentation rate of erythrocytes, leukocytes and lymphocytes.
- Blood chemistry. The results of kidney tests - urea and uric acid - are carefully examined in order to exclude a diagnosis such as gouty arthritis.
- General urine analysis. To determine hidden inflammatory processes in the genitourinary tract.
Based on the data obtained, a final diagnosis is made, after which a treatment regimen is prescribed. Therapy methods are selected depending on the stage of development of the disease.
Diagnostics
Before starting treatment for gonarthrosis of the knee joint, CELT doctors carry out diagnostics that make it possible to identify the cause and extent of the disease, as well as determine subsequent treatment. To do this, an examination is carried out by a specialist, anamnesis is taken, an X-ray examination, computed tomography and magnetic resonance imaging are performed. An integrated approach allows you to study pathological changes in bone structures in detail, as well as determine changes in soft tissues.
Treatment of bilateral knee joint gonarthrosis
Depending on the stage of development of the disease, treatment tactics are chosen. At the initial stages, complex conservative therapy is indicated, including the use of medications and physiotherapeutic procedures. If the joints are almost completely worn out, they are replaced surgically and endoprosthetics are performed. In the presence of stages 1 and 2 of the disease, complex conservative therapy with the prescription of medications is indicated.
What medications are prescribed for symptomatic treatment of pain:
- Non-steroidal anti-inflammatory drugs. These medications are the first-line pharmacological group of choice, as they have a number of advantages over other drugs - they act quickly, rarely cause side effects during short course use, and are easy to use (it is enough to give an injection or take a tablet 1-2 times a day). People with kidney, heart, and stomach diseases should take NSAIDs with caution. Examples of medications: Diclofenac solution for injection, Ibuprofen tablets.
- Corticosteroids. They can be used in combination with NSAIDs if there is severe pain and inflammation, or used in the form of intra-articular blockades. GCS is prescribed only if the use of non-steroidal painkillers does not help relieve severe pain during exacerbation. Individuals with diabetes, obesity, and hypertension should use corticosteroids with caution. Examples of medicinal names are Hydrocortisone, Kenalog, Diprospan.
- Anesthetics. This type of medication is not taken as a separate drug for the symptomatic treatment of gonarthrosis, but these drugs are always included in the blockade with GCS. Anesthetics have a powerful but short-term anesthetic effect, therefore they complement the work of the drugs included in the intra-articular blockade. During the injection procedure, the needle with the medicine is inserted at an angle, which makes it possible to fully penetrate the joint without touching the soft tissue. The course of treatment is short, it is enough to give 1-2 injections and the pain goes away quickly.
- Muscle relaxants. Often with arthrosis there is a violation of muscle conduction. Some muscles lose tone due to limited movement, which can cause severe spasms at the slightest load. Muscle relaxants reduce nerve conduction, thereby relaxing the pathological spasm.
Additionally, external agents are prescribed - ointments, gels, homeopathic mixtures. When the exacerbation period passes, the patient needs to attend physiotherapeutic procedures.
For preventive purposes, the following medications are prescribed:
- Chondroprotectors. These medications are used for preventive purposes. At the initial stages, chondroprotectors can help eliminate mild discomfort and stiffness that appear against the background of the growth of osteophytes. Regular use of chondroprotectors allows you to slow down the growth of bone masses in the joints. In medical practice, the most effective chondroprotectors are used, which consist of a combination of glucosamine and chondroitin. A specialist may prescribe injections that need to be performed once a day for at least 2-3 months without a break. An example of an effective medication is Rumalon (injected contents are extracts from fish cartilage), Chondrosat, Mucosat. Detailed information on use is contained in the instructions.
- Calcium and vitamin D3 preparations. Persons suffering from diseases of the musculoskeletal system are many times more likely to develop calcium-phosphorus metabolism disorders than a completely healthy person. To eliminate the risk of developing osteoporosis, it is necessary to periodically take calcium and vitamin D3 supplements several times a year. Calcium is the main building material for bones, but without cholecalciferol its normal absorption is impossible. It is especially important to take calcium supplements in the elderly, since their risk of fractures in the presence of bilateral gonarthrosis is significantly increased. An example of medications is Aquadetrim, Kalcemin, Detrimax.
- B vitamins. These drugs are prescribed as part of complex treatment, as they have a general strengthening and tonic effect. In the presence of degenerative-dystrophic diseases of the joints, vitamin complexes support the immune system and improve well-being. Examples of funds are Milgamma, Neurorubin.
Non-drug treatments
One of the most important stages in the recovery of the body after an exacerbation of gonarthrosis of the knees is exercise therapy, physiotherapeutic procedures, and visiting a massage room. Osteoarthritis of the joints often provokes stiffness and decreased range of motion, which leads to an unfavorable prognosis if you do not engage in gymnastics. To develop mobility of the knee joint, you need to do hip flexion and extension every day. This simple action will help develop normal motor range. If there is swelling in the knees, it is better to do the exercises while lying on your back.
Development of grade 3 gonarthrosis
Physiotherapy is an effective set of procedures aimed at eliminating stiffness and chronic pain. The mechanism of action of treatment methods is based on the effect on joints, soft tissues and ligaments through magnetic or current radiation. The device emits a certain frequency, which has a beneficial effect on joints in the presence of arthrosis. To enhance the effect, drugs are prescribed that have anti-inflammatory, restorative and analgesic effects. These may be mixtures of corticosteroids, vitamins, NSAIDs or muscle relaxants. The number and frequency of procedures used depends on the doctor’s orders. Typically, the number of scheduled sessions is determined in advance.
Massage also effectively helps in the treatment of arthrosis of the knee joints. The essence of the method is to relax the tight muscles surrounding the knee. You cannot do massages during an exacerbation. This therapy is indicated during the recovery period, when the pain has passed and remission is observed. Also, with the help of massage, local blood flow improves, which has a positive effect on well-being. The patient begins to move more easily, as the feeling of stiffness subsides.
Treatment
It is currently impossible to completely cure gonarthrosis, but the development of the disease can be significantly slowed down. This is exactly what the orthopedists at the CELT clinic focus all their efforts on. The earlier the course of treatment is started, the longer the development of pathological processes is delayed. Drug treatment consists of taking non-steroidal anti-inflammatory drugs, which can not only minimize pain, but also relieve inflammation. In addition, physiotherapeutic treatment and exercise therapy are used.
As for surgical treatment at the CELT clinic, it allows one to achieve positive results and is carried out only if there are indications. One of the low-traumatic but effective methods of surgical intervention is arthroscopy. It is an intra-articular procedure aimed at eliminating mechanical problems in affected joints in elderly patients.
Do you want to lead a normal lifestyle and not limit yourself to anything? Contact CELT - and we will make every effort to restore your health.
Prevention
There are no specific preventive measures to prevent knee arthrosis. General precautions include adequate exercise, avoiding overexertion, proper nutrition, and drinking plenty of water. It is important to protect yourself from stress and avoid prolonged sitting or standing in one place. It is also required to wear orthopedic shoes, which relieve stress on the feet, knees, lower back and hip joints. Women are contraindicated from wearing high heels.