Osteoarthritis is a joint disease that is most common in older people. As a rule, the disease affects the joints of the hands, hip and knee joints, as well as the lumbar and cervical spine.
Often pathology is recorded in people of a certain profession. So, football players and hockey players are characterized by osteoarthritis of the knee joint, journalists and secretaries - osteoarthritis of the fingers, ballerinas - inflammation of the feet, plasterers, masons and painters - damage to the shoulder joints.
1
X-ray of the cervical spine
2 X-ray of hip joints
3 X-ray stop
Types of osteoarthritis
Depending on the cause of primary and secondary osteoarthritis are distinguished
Primary osteoarthritis appears for an unknown reason, and secondary joint pathology can occur after injuries, inflammatory processes (rheumatoid osteoarthritis, purulent inflammation of the joint, arthritis with systemic lupus erythematosus, etc.), endocrine diseases and metabolic disorders.
Classification by location:
- generalized osteoarthritis - inflammation of all joints of the body;
- Osteoarthritis of the spine can also affect the cervical and lumbar regions. With this pathology, a person feels pain both when moving and during prolonged standing and sitting;
- Osteoarthritis of the hip joint is characterized by pain in the thigh, buttocks and groin. The patient is limping and has difficulty moving. In advanced cases, the thigh muscles atrophy and bone tissue begins to deteriorate;
- Knee osteoarthritis occurs when the knee is injured. When moving, a person feels pain, restriction in movement, which subsequently leads to joint deformation;
- osteoarthritis of the elbow joint - a problem with bending the arm, a tingling sensation is felt in the affected joint;
- osteoarthritis of the shoulder joint is characterized by the inability to raise the arm upward, subsequently the shoulder becomes completely immobile;
- Osteoarthritis of the hands appears in women during menopause; the symptoms of the disease are swollen joints and stiffness of movement in the morning.
Don't underestimate osteoarthritis! Advanced disease can lead to impaired mobility and joint deformation. and also to complete loss of ability to work!
Only timely, qualified treatment will help your joints!
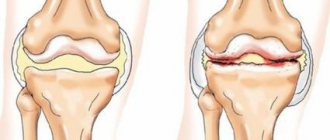
What actually happens with osteoarthritis?
With this disease, intensive aging of the articular cartilage occurs. The result is a loss of elasticity of the articular cartilage. In addition to the fact that the articular surfaces become rough, cracks also appear on them. In many cases, the cartilage wears away so much that the bone is exposed. All this leads to a decrease in the elasticity of the articular cartilage and causes dysfunction of the joints. Further, all of the above changes can be accompanied by inflammation, which causes bone tissue to grow, and this leads to disease and deformation of the joints.
Symptoms of osteoarthritis
Osteoarthritis can develop over a long period of time, sometimes unnoticed. Pay attention to the following signs of joint pathology:
- localized periodic pain in the joint, which appears during exercise and subsides again at rest;
- morning stiffness in the joints;
- the appearance of inflammation in joint tissues;
- swelling in the joint, cracking noise when moving;
- decreased range of motion in the joint;
- loss of mobility and joint deformation.
Degrees of osteoarthritis
Osteoarthritis stage 1 . Pain during exercise and at rest, joint mobility is slightly limited.
Osteoarthritis grade 2 . The pain intensifies, and a crunching sound is heard when moving the joints. Limitation of mobility in the joints, the appearance of restrictions in the range of motion. Treatment is conservative, without surgery.
Osteoarthritis grade 3 . Constant pain in the joints, which intensifies with movement, persistent contractures. Significant limitation of joint mobility. If the legs are affected, a person can move only with the help of a cane, crutches, or walker.
1 General blood test
2 Diagnosis of osteoarthritis
3 Consultation with a rheumatologist
Classification
Deforming osteoarthritis has several degrees of severity, determined by the characteristics of the disease and on the basis of a medical examination.
The scientific community distinguishes three stages of this disease:
- the first degree is set when there is a slight decrease in the level of joint mobility, its edges are very slightly deformed, the joint space has narrowed only slightly, and the growths are at the initial level;
- the second degree is marked by a decrease in the mobility of the cartilage, the appearance of crunches during movements, mild muscle atrophy, a more obvious narrowing of the gap and the appearance of significant bone growths;
- third degree is the most serious. The joint is severely deformed and severely limited in its movements, the joint space is completely absent, the bone is clearly changed. There are many growths and cysts.
Some experts also distinguish another stage - the initial stage of development of the disease. It is difficult to detect because it does not appear on x-rays.
Causes of the disease
A number of reasons can contribute to the appearance of the disease:
- injury or overstrain of joints due to increased physical activity;
- decrease in the amount of estrogen in women during menopause;
- elderly age;
- joint surgery;
- excess body weight;
- hereditary predisposition;
- disruption of the activity of endocrine organs;
- osteoporosis, etc.
Diagnosis of osteoarthritis
Osteoarthritis of the joints is detected using the following studies:
- X-ray diagnostics;
- Ultrasound of joints;
- MRI of joints;
- blood tests: general and biochemical;
- diagnosis of synovial fluid.
1 MRI of joints
2 Diagnosis of osteoarthritis
3 Consultation with a rheumatologist
Treatment of osteoarthritis
Treatment of osteoarthritis is a long-term process, during which it is necessary to follow all the recommendations of an orthopedic doctor and rheumatologist.
When treating deforming osteoarthritis, analgesics and non-steroidal anti-inflammatory drugs are used to relieve pain and improve the functioning of the diseased joint.
To reduce inflammation of the synovium of the joint and relieve acute pain, the doctor may prescribe injections of corticosteroid hormonal drugs that are given inside the joint.
To prevent the destruction of joint tissue, chondoprotectors are prescribed.
If necessary, surgical procedures can be used, which include removal of the affected parts of the joint and endoprosthetics. One of the optimal treatment methods is arthroscopy.
Why is arthroscopy needed?
Arthroscopy is a minimally invasive surgical procedure used to diagnose and treat the affected part of the joint.
Today, arthroscopic surgery is considered one of the best types of surgical treatment, with which you can not only replace and remove damaged tissue, but also restore the joint itself. And also analyze the condition of various bones.
Main types of atroscopy:
- Arthroscopy of the knee joint (or meniscus). In case of rupture of the meniscus, posterior and anterior cruciate ligaments, artificial grafts or those taken from the patient’s own ligaments can be used.
- Arthroscopy of the shoulder joint . Indispensable for the prevention and treatment of lesions of the shoulder joint. Athletes often experience a rotator cuff tear, while other patients often experience joint instability and shoulder dislocation.
- Arthroscopy of the hip joint . Used to assess the condition of the femur and other articular elements and provide appropriate treatment. This manipulation is carried out much less frequently and only by specialists with extensive experience.
- Arthroscopy of the elbow joint is prescribed as a diagnosis for pain in the arm and any problems with flexion-extension of the limbs. For arthritis, a surgical form of this technique is possible.
- Arthroscopy of the ankle joint . Pathology of the ankle joint is characterized by a fairly large number of indications for surgery. A month after arthroscopy, the patient can move comfortably, leaning on a stick.
Indications for arthroscopy
The arthroscopic technique is universal and is used for both diagnosis and surgical treatment.
Indications for arthroscopic diagnosis:
- joint instability;
- various dislocations and subluxations;
- the appearance of chronic inflammation in bone tissue;
- meniscal cyst,
- injury to the meniscus and cartilage in the knee joint;
- ligament ruptures in the knee;
- removal of foreign bodies, as well as growths and adhesions from the articular cavity;
- washing joints and removing excess fluid;
- arthrosis and arthritis.
How is arthroscopy performed?
Arthroscopy can be performed under either general or local anesthesia. Local anesthesia is usually sufficient. The duration of the manipulation is from half an hour to an hour (depending on the type of problem and the required surgical intervention).
Knee arthroscopy is performed through small incisions in the knee area. The knee cavity is washed with a special solution; this is done to improve the visibility of the articular surfaces and remove pathological fluid from the joint.
During diagnostic arthroscopy, an arthroscope is inserted into the cavity of the knee joint, which transmits an accurate picture of the condition of the joint to the monitor.
If surgical treatment , the doctor inserts the necessary surgical instruments through other incisions in the joint. After the manipulation, sutures and sterile patches are applied, then the joint is bandaged. If all the doctor’s instructions are followed, after 1.5-2 months the patient can return to normal life.
1 Consultation with a rheumatologist
2 Consultation with a rheumatologist
3 Consultation with an orthopedist
What is osteoarthritis and how to deal with it
(information for people suffering from arthrosis)
WHAT IS OSTEOARTHROSIS?
Osteoarthritis is a very common joint disease, affecting about 80% of our population aged 50-60 years, but sometimes it appears earlier, at the age of 30. In osteoarthritis, the articular cartilage is primarily affected. As you know, a joint is formed by the articular surfaces of bones covered with cartilage tissue. During various movements, cartilage acts as a shock absorber, reducing pressure on the articulating surfaces of bones and ensuring their smooth sliding relative to each other. Cartilage consists of connective tissue fibers loosely arranged in a matrix. The matrix is a jelly-like substance formed by special compounds - glycosaminoglycans. Due to the matrix, cartilage is nourished and damaged fibers are restored. This structure makes cartilage look like a sponge - in a calm state it absorbs liquid, and when loaded, squeezes it into the joint cavity, providing a kind of “lubrication” of the joint.
During life, cartilage reacts flexibly to stereotypical shocks repeated thousands of times during certain types of work or running, jumping, etc. This constant load leads to aging and destruction of some of the fibers, which in a healthy joint is compensated by the synthesis of the same amount of new fibers. Osteoarthritis develops when there is an imbalance between the formation of new building material for the restoration of cartilage tissue and destruction. A kind of less valuable cartilage structure arises, capable of absorbing smaller volumes of water. The cartilage becomes drier, brittle, and in response to stress, its fibers are easily split. As arthrosis progresses, the layer of cartilage covering the articular surfaces becomes thinner, until it is completely destroyed.
Along with the cartilage, the bone tissue underneath also changes. Bone outgrowths form along the edges of the joint, as if compensating for the loss of cartilage by increasing the articular surfaces. This is the cause of joint deformities due to arthrosis. Popularly, this condition is called “salt deposition,” which is simply an illiterate name for arthrosis disease.
WHAT FACTORS LEAD TO OSTEOARTHROSIS?
There appears to be no single reason leading to the development of this disease. A number of factors are important, one way or another weakening the cartilage, the harmful effects of which accumulate throughout life and ultimately lead to the development of arthrosis. The onset of the disease in this situation can be characterized as an unfavorable combination of circumstances, and these circumstances are different for each person. Nevertheless, a number of factors can be identified, the presence of which increases the risk of developing arthrosis.
1. AGING - With age, cartilage becomes less elastic and loses its resistance to stress. This does not mean that all people develop arthrosis in old age. But in the presence of other predisposing factors, the risk of getting sick increases with age.
2. CONGENITAL FEATURES - Connective tissue dysplasia syndrome is currently widespread. This is a congenital weakness of connective tissue, manifested by increased joint mobility, early development of osteochondrosis, and flat feet. If a certain motor regimen is not observed, this condition can lead to the development of arthrosis at a young age.
Another fairly common congenital anomaly is complete or incomplete dislocation of the hip joint (this is why preventive examinations of newborns are carried out immediately after birth), which, if it is incorrectly reduced or treated incorrectly, leads with age to a severe form of osteoarthritis of the hip joint.
3. GENETIC PRESPOSITION - It has been proven that the predisposition to the nodular form of arthrosis affecting many joints is inherited. Women whose mother suffered from this form of arthrosis have an increased risk of developing the disease.
4. INJURIES - Severe simultaneous injuries, accompanied by a bruise, fracture, dislocation, damage to the ligamentous apparatus of the joint, or repeated microtrauma to the joint, can contribute to the development of arthrosis. Microtraumatization is the cause of the development of arthrosis in workers of a number of professions and professional athletes. An example is the development of arthrosis of the knee joint in miners and football players; arthrosis of the elbow and shoulder joints in those working with a jackhammer; arthrosis of small joints of the hands in secretaries - typists, weavers; arthrosis of the ankle joints in ballerinas; arthrosis of the hand joints in boxers, etc.
5. RELATED DISEASES - Any metabolic disorders, endocrine disorders contribute to the development of arthrosis. Arthrosis often develops in obese people, in patients with diabetes mellitus, thyroid diseases, and in menopausal women. Various circulatory disorders in the extremities, such as varicose veins and atherosclerosis, also contribute to the development of arthrosis.
HOW DOES OSTEOARTHROSIS MANIFEST?
The first symptom that makes you see a doctor is pain in the joint. The intensity of pain can vary - from pronounced, limiting joint mobility, to moderate, occurring only with certain movements.
The cause of severe pain, as a rule, is reactive inflammation of the joint (so-called synovitis) or inflammation of the tissues surrounding the joint (muscles, tendons, bursae). Inflammation in the joint occurs due to the fact that pieces of destroyed cartilage enter the articular cavity and irritate the synovial membrane of the joint. Inflammatory pain is quite pronounced, intensifies with any movements in the joint, and also occurs at rest in the 2nd half of the night. When the tissues surrounding the joint (tendons, bursae) are inflamed, the pain intensifies when performing certain movements, there are painful points in the joint area, and “starting” pain is characteristic (after a period of rest it is difficult to start movement). With proper treatment, inflammation in the joint or surrounding tissues can be stopped, which is accompanied by subsidence of pain, disappearance of night pain, and improved joint mobility.
In the absence of inflammation, in the initial stages of arthrosis, the pain syndrome is mild. Pain occurs only when there is significant stress on the joint, such as prolonged fixation of the joint in one position (sitting in an uncomfortable position), prolonged walking or running, or carrying heavy bags. These pains go away after a short rest and relaxation of the joints. In advanced stages of arthrosis, pain is almost constant.
WHAT JOINTS ARE AFFECTED IN OSTEOARTHROSIS?
In principle, arthrosis can develop in any joint. Depending on which joints are predominantly affected, several forms of arthrosis are distinguished. In the first form, the small joints of the hands and feet are mainly affected. Dense nodules, the so-called Heberden's nodes, form on the fingers. These nodules are bony outgrowths along the edges of the joints. During the formation stage, they can be painful, and the skin over them may turn red. Then the inflammation subsides, painless joint deformities remain, and hand function remains satisfactory. In the form of osteoarthritis with predominant damage to the joints of the 1st fingers, the function of the hand noticeably deteriorates already in the early stages of arthrosis. The next form is osteoarthritis of the supporting joints. Weight-bearing joints include the knee and hip joints. Osteoarthritis of the knee joints is called gonarthrosis. Arthrosis of the hip joints - coxarthrosis. And finally, there is a form of osteoarthritis that affects many joints at once, then they talk about polyosteoarthrosis.
WHAT EXAMINATIONS ARE NECESSARY FOR DIAGNOSIS OF OSTEOARTHROSIS?
A rheumatologist can suspect osteoarthritis based on complaints, medical history, and examination of the patient. To confirm the diagnosis, radiographs of the most disturbing joints are necessary. The photographs show changes characteristic of arthrosis: in the early stages, the contour of the bones forming the joint is emphasized, then the joint space narrows, and bone growths form along the edges of the joint. Depending on the severity of changes on radiographs, there are 4 stages of arthrosis - from the first, with minimal changes, to the fourth, when the structure of the joint is almost completely damaged. Among additional research methods, thermographic (thermal imaging) and ultrasound (ultrasound) examination of joints can help to detect inflammation in the joints or surrounding tissues, which cannot be seen on an x-ray.
PROGNOSIS (FUTURE) FOR PATIENTS WITH OSTEOARTHROSIS The prognosis for patients with osteoarthritis can be considered quite good and even good, and this is not false optimism. The opinion that this disease is constantly progressive is unfounded. Complete disability due to osteoarthritis is rare, and most patients experience joint problems only occasionally. When they say that arthrosis is incurable, it means that those changes that have already formed in the joint cannot be reversed. But, as a rule, when you first consult a doctor, these changes are insignificant, and by following a certain motor regimen and recommendations for rehabilitation, you can prevent further progression of arthrosis. It should also be remembered that with this disease, periods of exacerbation associated with reactive inflammation of the joint are followed by periods of rest, when the joint is practically not bothered or complaints are minimal.
HOW TO LIVE WITH OSTEOARTHROSIS
The appearance of the first symptoms of arthrosis should not be a reason for panic, but rather a signal from the body about the need to slightly change the existing motor stereotypes.
Firstly, you need to try to limit movements associated with increased load on the articular cartilage. With arthrosis of the hip, knee, and ankle joints, it is necessary to reduce such types of physical activity as running, jumping, lifting and carrying heavy objects, squats, fast walking, especially over rough terrain, climbing hills, and walking up stairs.
All of these activities place a force on the affected joints that is significantly greater than the body's weight, which is harmful to the already damaged cartilage. You should also avoid fixed positions, such as prolonged sitting or standing in one position, squatting or bent position when working in the garden. Such postures impair blood flow to diseased joints, as a result of which the nutrition of the cartilage also deteriorates. If the joints of the hands are affected, you should limit carrying heavy objects, manually pushing up heavy things, typing on a stiff typewriter, playing musical instruments, etc.
In any case, it is necessary to develop a rhythm of motor activity so that periods of load alternate with periods of rest, during which the joint should be unloaded. Approximate rhythm - 15-20 minutes. load, 5-10 min. rest. You need to unload the leg joints in a lying or sitting position. In the same positions, you can perform several movements in the joints (flexion, extension, bicycle) to restore blood circulation after exercise.
Secondly, despite the presence of a number of restrictions, it is necessary to lead an active lifestyle by increasing physical activity, which does not have a negative effect on cartilage. You need to force yourself to do special exercises every day, some of which are given below. A common feature of these exercises is that when they are performed, the load on the articular cartilage is minimal, and the muscles surrounding the joint work to a greater extent. This allows you to form a good muscle corset around the joint, maintain normal mobility and sufficient blood circulation in the limb. In addition, these exercises strengthen the cartilage itself, which requires movement for normal nutrition. Regular practice of these exercises should turn from an unpleasant chore into a useful habit, which is the best way to maintain normal joint function. You need to exercise for at least 30-40 minutes a day, it is better to divide this time into several times a day for 10-15 minutes. A noticeable effect occurs within 2-3 months - the pain syndrome decreases, vitality increases, and the body's hidden reserves are released.
SOME TYPES OF EXERCISES FOR PATIENTS WITH OSTEOARTHROSIS:
It is always best to start exercising under the guidance of a rehabilitation specialist (physical therapy doctor), preferably in health groups specialized for a given localization of arthrosis. After finishing the group classes, you need to continue studying at home, using the acquired skills. The main principle is to repeat the exercises frequently throughout the day for several minutes. Exercises should be performed slowly, smoothly, gradually increasing the amplitude. In this case, it is better to focus on the sore joint, think about how, during movements, blood flows to the joint, bringing with it nutrients that, when the limb relaxes, feed into the cartilage, and during movements are squeezed into the joint cavity, providing good “lubrication” to the joint.
OTHER OPPORTUNITIES FOR IMPROVING PHYSICAL FIT:
1. Walking on level ground at a moderate pace is a good way to maintain muscle tone. Try to take a 20-30 minute walk every day. The main thing is not to rush, since when walking quickly, the load on the joints begins to exceed body weight by 1.5-2 times. Walking shopping with heavy bags also does not improve your physical fitness.
2. Swimming is an optimal sport for diseases of the musculoskeletal system. In water, maximum range of motion in the joints is possible without weight bearing, which is optimal for articular cartilage. If you don't know how to swim, you can practice in aquagymnastics groups.
3. Exercising on exercise machines more effectively allows you to form a muscle corset. The same goes for the cycling trainer. It is important to correctly fit the exercise bike to your figure (the leg should be straight in the lower position) and ensure that the exercise bike is firmly secured to the floor.
4. Cycling, in addition to its beneficial effect on joints, brings a positive emotional charge. You should avoid riding on uneven terrain (bouncing movements harm your joints), as well as falling from the bike. If you have difficulty maintaining balance, weakness, vision problems, or are not very confident in the saddle, then it is better to exercise at home on an exercise bike. It is also important to choose the right bike. You need to choose between a sports and semi-sports type, since they are lighter and faster than road ones. Since the handlebars on sports bikes are lowered down, while on road bicycles they are usually horizontal or raised, it is more convenient to raise the handlebars on a sports bike. The most problems arise when the saddle height is set incorrectly. It should be set so that when the pedal is fully pressed in the down position, the leg is fully straightened. If the knee is bent in this pedal position, pain in the joints and muscles occurs. The distance to the steering wheel is also important - your elbows should be slightly bent. A cyclist, unlike a pedestrian, puts stress on other muscles. Therefore, to begin with, a 15-20 minute drive is enough, later, depending on the capabilities, the duration of the trips can be extended to 30-40 minutes.
5. In winter, skiing is useful, since sliding reduces the weight load.
OTHER METHODS OF REHABILITATION 1. MASSAGE - improves overall well-being, relieves painful muscle spasms, improves blood circulation, transmission of nerve impulses, thereby ensuring improved nutrition of articular cartilage. Massage should be done by an experienced specialist in the absence of exacerbation of arthrosis. The area above the joint is treated with minimal intensity. The spine is treated more intensively, from where the nerves supplying the joint and adjacent muscles emerge. In the absence of contraindications, the massage is repeated 2 times a year.
2. PHYSIOTHERAPY - also helps to improve the nutrition of cartilage. Soft methods of influence are indicated, such as magnetic therapy, laser therapy, electrophoresis with dimexide and brine, EHF therapy, laser therapy. In the absence of contraindications, physiotherapy courses are repeated 2 times a year.
3. SANATORIUM TREATMENT - allows for comprehensive rehabilitation, including the positive effects of therapeutic mud, baths, saunas, physiotherapy, massage, and physical therapy. An important role is played by a change of environment, relieving stressors, and being in the fresh air. It should be remembered that sanatorium-resort treatment can only be carried out without exacerbation of the disease.
4. ORTHOPEDIC CORRECTION DEVICES are special devices that reduce the load on the joint. These include orthopedic shoes, which must be worn if there is a shortened limb; instep supports prescribed for flat feet; knee pads that can reduce the laxity of the knee joint, thereby reducing trauma to the cartilage when walking. Instead of knee pads, you can use an elastic bandage.
DRUG THERAPY Drug treatment for arthrosis is prescribed during an exacerbation of the disease and is aimed at relieving inflammation in the joint or tissues surrounding the joint. For this purpose, anti-inflammatory drugs are prescribed, such as Diclofenac, Ibuprofen, Indomethacin, etc. It should be remembered that these drugs can have a negative effect on the gastrointestinal tract, so they should be taken after meals, in short courses - 10-15 days. There are modern drugs of this group that irritate the stomach to a much lesser extent, such as Tinoctil, Arthrotek, Movalis. It is imperative to combine the use of anti-inflammatory drugs with local treatment. Pharmacies have a large selection of ointments with anti-inflammatory properties, such as Indomethacin, Butadionic, etc. Among the more modern ones, Fastum-gel, Diclofenac-gel, Dolgit-cream, Erazon, Revmagel have proven themselves well. The ointment is applied to clean skin over the joint 2-3 times a day. Compresses with dimexide have a very good anti-inflammatory effect. Dimexide is sold in pharmacies and diluted 2-3 times with boiled water. Novocaine or analgin and hydrocortisone can be added to the resulting solution (the latter is contraindicated for hypertension and venous diseases). Compresses are placed over the area of sore joints for 40 minutes before bedtime. There are 20-30 procedures per course. Do not try to relieve a joint aggravation on your own. Experience shows that better and faster results can be achieved by early consultation with a doctor, preferably a specialist (rheumatologist or arthrologist).
INTRA-ARTICULAR ADMINISTRATION OF MEDICINES: Prescribed by a doctor to more quickly and effectively relieve inflammation in the joint. The drugs used are Kenalog, Diprospan, Celeston, Depo-Medrol, Flosteron. Many patients experience significant improvement after the first intra-articular injection, and subsequently require this procedure even with minor discomfort. I repeat that this procedure does not treat arthrosis, but allows you to stop inflammation, and if often unjustified, it is harmful to the joint.
USE OF CHONDROPROTECTORS Chondroprotectors are drugs that improve the structure of cartilage. Taking these drugs is not aimed at relieving inflammation in the joint, but helps slow the progression of arthrosis and strengthen cartilage tissue. Chondroprotectors can be taken orally, intramuscularly, or intraarticularly. The first include drugs “Dona”, “Structum” or nutritional supplements containing chondroitin sulfate or glycosaminoglycans, which are the building material of cartilage. The course of treatment with any of these drugs should be 6-8 weeks.
Chondroprotectors administered intramuscularly include rumalon, alflutop, mucarthrin, arteparone, etc. The course of treatment requires 20-25 injections, administered every other day.
Alflutop, Traumeel, and purpose can be administered intra-articularly. Such manipulations are carried out by an experienced doctor, in the absence of inflammation in the joint. The course usually requires 6-10 injections.
For a good effect, courses of treatment with chondroprotectors must be repeated 2 times a year for several years.
Following all the recommendations listed above will allow you to maintain satisfactory joint function for a long time in your life.
Prevention of osteoarthritis
To prevent osteoarthritis, you need to lead a healthy lifestyle. Compliance with an orthopedic regimen, physical therapy, proper nutrition, rest and sleep patterns - all this will help keep your joints healthy for many years.
The MedicCity clinic pays special attention to the diagnosis and treatment of osteoarthritis, gout, osteoporosis, lupus erythematosus and other rheumatoid diseases.
We take a comprehensive approach to maintaining the health of patients: after treating the underlying disease, you can take courses in massage, manual therapy, physical therapy, etc.
Easy movement for you and your joints!