01.12.2020
Bursitis of the knee joint is called inflammation of the synovial bursa (bursa), which is located between the bones and tendon fibers. A healthy bursa reduces friction when walking. An inflamed cavity makes it difficult for the joint to move and causes a feeling of discomfort. The inflammatory process can develop in one or several cavities at the same time.
Bursitis - what is it?
Bursitis is an inflammation of the joint capsule. It is caused by a pathological process occurring in the mucous membrane of the bursa. As a result, a large amount of fluid accumulates inside it (effusion), and this leads to significant functional impairment. Moreover, the greater the effusion, the stronger the dysfunction of the joint.
ICD-10 code:
- A54.4 - Gonococcal infection of the musculoskeletal system.
- M06.2 - Rheumatoid bursitis.
- M70 - Soft tissue diseases associated with stress, overload and pressure.
- M71.1 - Other infectious bursitis.
- M71.5 - Other bursitis, not elsewhere classified.
- M73.0 - Gonococcal bursitis (a54.4).
- M73.1 - Syphilitic bursitis (a52.7).
- M75.5 - Bursitis of the shoulder.
- M76.4 - Tibial collateral bursitis [pellegrini-stidy].
Typically, joint inflammation is associated with excessive stress.
Mostly all diseases of the musculoskeletal system begin acutely, the first symptom being pain. As a result, a person cannot fully move and sometimes even do his job. The development of bursitis is a fairly rapid process. However, in the initial stages, this disease is highly treatable.
Patients never notice how important the musculoskeletal system plays in their lives until some kind of breakdown occurs in it.
The target joints of bursitis are precisely those joints in which the disease develops most often. This predisposition may change, and bursitis may occur in other joints, which does not exclude this diagnosis, but is only statistically less likely.
The most common target joints for the development of bursitis are the knee and elbow joints. “Golfer's elbow” is a well-known expression in the sports world. Because bursitis of the elbow joint mainly affects people of such professions (golfers, tennis players).
Knee bursitis is more common among professional dancers, runners, and other track and field athletes. It is on this joint that the greatest load falls on them, and the body’s compensatory systems cannot always distribute it evenly.
In addition to bursitis, which occurs in athletes, there are diseases of infectious and autoimmune etiology. The difference between these and post-traumatic types of bursitis is treatment. When the disease is infectious, antibiotics are used, and when it is autoimmune, corticosteroids and cytostatics are used.
Diagnostic methods
Ultrasound is one of the most informative diagnostic methods
Before prescribing therapy, the attending physician will ask the patient to undergo the necessary diagnostic measures. They will help the specialist correctly determine the diagnosis and identify the person’s existing disorders that are contraindications to certain types of therapy.
A traumatologist, therapist and orthopedist can diagnose bursitis of the knee joint. At the initial stage of therapy, the doctor collects anamnesis and conducts a visual examination of the area affected by inflammation, in this case the knee.
Next, the patient is sent to undergo diagnostic procedures and tests:
- Ultrasonography;
- X-ray;
- Magnetic resonance imaging;
- Blood analysis.
Additionally, puncture of the contents of the joint cavity may be required to determine the composition of the fluid that fills it.
To confirm the diagnosis, differential diagnostics will be required. It allows you to distinguish bursitis from other similar pathologies, such as arthrosis, osteomyelitis and synovitis. For these purposes, computed tomography and joint arthrography are performed.
Types of bursitis
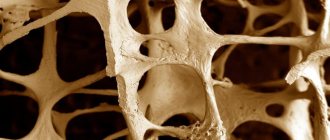
Bursitis is mainly the accumulation of a larger volume of fluid in the joint capsule than normal (more than 2.5-4 ml), which manifests itself as signs of inflammation. Based on the composition of this fluid, bursitis can be:
serous;- purulent;
- hemorrhagic (blood in the joint capsule).
The purulent form of bursitis is a consequence of incorrect treatment of serous bursitis. The main etiological (causal) role in its development is played by the infectious pathogen.
Depending on the course, the disease can be:
- sharp;
- subacute;
- chronic;
- recurrent.
Acute bursitis occurs and develops rapidly. Most often, with adequate treatment, the disease goes away without a trace. Consequences may occur in the case of its chronic and recurrent course.
In accordance with the factors leading to the development of bursitis, specific and nonspecific inflammation are distinguished. Specific ones include:
- chlamydial;
- gonorrheal;
- tuberculosis;
- syphilitic.
Causes of the disease
Why does a condition such as bursitis occur? Doctors say that a disease such as bursitis occurs if all three pathogenetic links are met:
there is a chronic source of infection (even carious teeth);- blood flow in the joint is impaired (constant loads, injury);
- the overall reactivity of the body is reduced (cannot fully resist infections).
Joint bursitis does not occur out of nowhere. For its development, the simultaneous presence of several factors is necessary. Some of the main reasons for its occurrence include:
- joint injuries that lead to organic disorders in the inner wall of blood vessels - the endothelium;
- the presence of a persistent focus of infection;
- slowing down blood flow in the area of articular tissues.
The likelihood of developing the disease is high if all three of the above conditions are met. If at least one of them is missing, bursitis will not occur.
Probable causes of the disease:
injuries and constant overload of the joint;- microbial and fungal pathogens (including “dormant” foci of infection, infection is possible through lymph and blood);
- systemic diseases (psoriasis, systemic lupus erythematosus, rheumatism);
- endocrine causes;
- metabolic diseases (gout).
Inflammation of the joint capsule is always associated with some factor. If, for some reason, this factor cannot be accurately established, they speak of an iatrogenic disease.
Bursitis "crow's foot"
The pes anserine bursa is located below the joint space, at the attachment point of the sartorius, subtendinous and gracilis muscles, which are connected into a single tendon, which is attached to the tibia. It is difficult to injure it, therefore inflammation of the presented bursa occurs as a consequence of previous diseases.
Foot anserine bursitis occurs primarily in athletes and older people. The impetus for development is deforming osteoarthritis, which occurs from excessive pressure on the joint elements. The disease also affects the adjacent tendons, causing inflammation (tendinitis).
A swelling forms at the back, pain is felt in the inner part of the knee, especially pronounced when going up and down the stairs. Due to the similarity of the clinical picture with other diseases, it is not always possible to make an accurate diagnosis during the initial examination, so additional examinations are carried out.
Symptoms of bursitis
Bursitis translated from Latin means “inflammation of the bursa” (joint capsule). Accordingly, the disease is manifested by all local symptoms of inflammation, as well as the body’s general reaction to the pathological process as a whole (it can have varying degrees of severity depending on individual reactivity).
Patients who have a mass formation in the joint area need to know what bursitis is and which doctor should be contacted with this problem.
The symptoms of bursitis differ little for inflammation of various joints. The main manifestations of the disease can be grouped into three categories:
pain syndrome;- functional disorders;
- changes in appearance and temperature.
Bursitis of deep-lying joints manifests itself as a slight swelling over the projection zones of these joints.
Bursitis is a disease that occurs as a result of the “settlement” of pathogenic microorganisms in the vessels supplying blood to the joint tissue. Clinical symptoms and complaints of patients with bursitis:
- joint pain;
- redness in the joint area;
- limited mobility;
- increased temperature, both local over the joint and general;
- increase in joint volume due to loss of inflammatory fluid;
- fluctuation over “weak” points of articulation;
- change in the shape of the joint (becomes more rounded);
- intoxication syndrome (for the bacterial nature of the disease).
The above symptoms occur within a few hours. There are serous and purulent stages of bursitis, each of which is characterized by its own manifestations.
Symptoms of the purulent stage of bursitis development are characterized by extreme severity. There is severe arching pain, even at rest. Mobility in the joint is sharply limited, and the local temperature above it is increased. When purulent bursitis develops, its symptoms are not so easy to treat. And in case of accumulation of pus in the joint capsule, surgical methods are used.
It is important to remember that purulent effusion negatively affects the condition of the joint. Adhesions and adhesions can form inside the joint. Articular cartilage also undergoes irreversible degenerative changes. All this has its consequences even after purulent bursitis is completely cured.
Symptoms (signs)
Clinical picture
• Acute bursitis •• Pain •• Local tenderness on palpation •• Limitation of range of motion •• Redness and hyperthermia of the skin with a superficial location of the bursa.
• Chronic bursitis •• Hardening of the bursa wall, intracavitary adhesions, calcification •• Atrophy of regional muscles.
• Localizations •• Shoulder joint area: subacromial bursitis •• Knee joint area: ••• Suprapatellar, infrapatellar (nun’s knee [forced kneeling for a long period of time]) ••• Prepatellar (maid’s knee [need to rest your knees on the bed when making bed]) ••• Semimembranous, or Baker's cyst, - communicates with the knee joint, can simulate arthritis of the knee joint •• Olecranon area (miner's elbow [rest on the elbow]). With rheumatoid arthritis, rheumatoid nodules are found in the walls of the bursa, with gout - tophi •• The ankle joint area: ••• Achilles bursitis ••• Calcaneal fasciitis ••• Plantar fasciitis •• The ischial tuberosity area (tailor's buttock) •• The greater trochanter area of the femur .
Exudate with bursitis
Exudate can be called any fluid in the body that is synthesized as a result of inflammation. Often, regardless of the organ, it has a constant composition and properties (protein, cell, glucose content).
By origin, exudate is blood plasma that has sweated from the venous vessels. Any inflammation in the immediate area of the lesion causes blood stasis in the venules (this is how the body is protected from possible bacteria, fungi and other damaging factors that could cause it). Some blood cells, electrolytes and even proteins also sweat with the plasma.
In acute bursitis, the tissues of the bursa are filled with serous exudate.
Normally, there is a small amount of fluid in the joint capsule. Its volume is approximately 4 ml in the knee joint and 2.5-3 ml in the elbow joint. It serves as shock absorption during movements. The main diagnostic sign for bursitis is a pathological increase in the volume of this fluid.
Causes
Etiology. Injuries, physical overload, arthritis (most often with rheumatoid arthritis and gout), infection with microorganisms (most often Staphylococcus aureus) or Mycobacterium tuberculosis.
Pathomorphology • In acute bursitis - stretching of the synovial bursa with exudate • In chronic bursitis - thickening of the walls of the synovial bursa, the inner surface is covered with fibrin deposits. The cavity of the bursa is filled with blood clots, and calcification of connective tissue structures is possible. Tendinitis and bursitis of the upper extremity most often occur as a result of repeated microtrauma, which ultimately leads to rupture of the connective tissue fibers of the tendon and bursa.
Diagnostics
The following are used to diagnose bursitis:
general clinical blood tests;- Ultrasound of the joints involved in the process;
- puncture of the joint cavity with microbiological seeding of the contents on nutrient media;
- determination of specific markers of various diseases (gout, connective tissue diseases, arthritis, autoimmune diseases).
As a result, data from diagnostic methods and certain clinical symptoms allow a diagnosis of bursitis to be made.
To diagnose acute bursitis of the knee, shoulder, and elbow joints, clinical data are sufficient. In some cases, an ultrasound of these formations may be required. But if bursitis of the deep-lying joints is suspected, symptoms alone may not be enough.
Some of the modern diagnostic methods are bursography and angiography. During bursography, a contrast agent is injected directly into the joint cavity (diagnostically significant - widening of the interarticular space, flow of contrast into the pockets of the bursa), and to perform angiography, it is sufficient to inject a radiopaque agent into the vascular bed near the affected joint. This method is used for the differential diagnosis of bursitis and hemangioma or lipoma.
To definitively confirm the diagnosis of acute bursitis, a joint puncture is performed. To do this, the joint capsule is pierced with a thick needle under anesthesia and a certain amount of liquid is taken for its microbiological inoculation on nutrient media. This is how the causative agents of the disease are identified.
Diagnosis of knee bursitis
BCS has quite clear external signs, so the primary diagnosis is based on an initial examination and anamnesis confirming the presence of injury. When diagnosing bursitis, it is important to differentiate it from arthritis. With similar symptoms, these are completely different diseases that can occur in parallel to each other.
Subtleties of diagnosing different forms of CSD:
- The easiest way to diagnose the infrapatellar form of bursitis, since in this case the inflammation is close to the skin;
- the chronic form is easier to determine by palpation of compactions, which are a consequence of fibrosis against the background of prolonged inflammation;
- deep bursitis that cannot be palpated is determined using x-rays.
If x-rays are not enough, to diagnose deep bursitis, the following is prescribed:
- arthrography;
- bursography;
- Ultrasound;
- puncture of the articular cavity;
- analysis of markers (arthritis, gout, autoimmune diseases).
After research and identification of clinical signs, a diagnosis is made, the nature of the pathology, its localization, and the degree of damage are clarified.
Treatment of bursitis
This disease is highly treatable and rarely leads to disability. The risk of complications such as osteomyelitis, ankylosis, deforming arthrosis is quite small. However, symptoms of bursitis should be identified in the initial stages of development. Then it is necessary to start treatment. All symptoms of bursitis can be treated, conservatively or surgically. As a conservative method of therapy, the following is used:
tablet and injection forms of drugs (anti-inflammatory, painkillers);- physiotherapeutic methods (allowed only in the final phases of the disease, when there is no pathological effusion, and it is necessary to fight only to restore joint function);
- physical methods to slow down the progression of inflammation;
- traditional methods of treatment;
- antibiotics.
When bursitis is diagnosed, treatment can only be carried out using pathogenetic and symptomatic therapy. Medicines can be administered either orally (orally) or parenterally (intravenously and intramuscularly). To reduce the consequences of bursitis, patients are prescribed a course of non-steroidal anti-inflammatory drugs (tablets, injections and ointments), such as Paracetamol, Diclofenac, Nimesulide, Meloxicam. In cases of severe bursitis with a high probability of disability, corticosteroids are prescribed.
Since the disease develops in the presence of a microbial pathogen, infectious causes of bursitis require a course of antibiotics to treat it.
These medications help fight infection, which is one of the main causes of bursitis. Broad-spectrum antibiotics are used, and if they are insufficient, a culture of the inflammatory fluid from the joint is done to identify microorganisms and their sensitivity, and then more specific drugs are prescribed. Antibiotics that can be used to treat bursitis: protected penicillins, macrolides, fluoroquinolones.
Treatment of pathology
CSD is a dangerous disease that, if left untreated, can cause impaired motor function and other serious consequences. Treatment is selected individually, the patient is prescribed medications and physiotherapy, and, if necessary, surgery.
Medications
Treatment of knee bursitis with medications is aimed at normalizing well-being, eliminating severe symptoms and promoting recovery. For the treatment of CSD, tablets, ointments, gels, vitamins, and injections are used.
Most often prescribed for bursitis:
- Dimexide. The solution is applied externally. It is used in combination with Novocaine to make compresses that eliminate pain, swelling and other symptoms.
- Voltaren Emulgel. Gel for external use has a powerful anti-inflammatory effect. Used in combination with other drugs.
- Diclofenac. This is a non-steroidal anti-inflammatory drug, available in the form of intramuscular injections or tablets. The product relieves swelling, inflammation, and local hyperthermia.
- Chondroxide. One of the most popular chondroprotectors. Restores cartilage tissue and ligaments. Release form: tablets.
Bursitis is actively treated with topical medications. Particularly popular are ointments based on snake and bee venom - Viprosal, Virapin, Apizartron.
Physiotherapeutic procedures
For CSD, various physiotherapeutic procedures are prescribed to help cope with the disease. They suppress symptoms and prevent the progression of the disease. One procedure takes about half an hour, and they are carried out several times a day. Course - 5-20 days.
The most effective manipulations:
- ultrasound;
- electrophoresis;
- X-ray therapy;
- diathermy.
In addition, radon and hydrogen sulfide baths are prescribed.
Folk remedies
In folk medicine there are many methods for treating bursitis. All of them are safe, but their effectiveness manifests itself mainly at the initial stage of the disease.
Folk remedies for the treatment of BCS:
- A cabbage leaf is tied to the sore knee, preferably overnight. This method effectively relieves inflammation.
- Fresh leaves of Kalanchoe or aloe (it is recommended to take large ones) are ground and applied to the inflamed knee. A bandage with aloe resolves inflammation.
- Dry burdock root is ground into powder and mixed 1:1 with some animal fat. The resulting mixture is rubbed into the knee and a tight bandage is applied.
- Applying freshly picked lilac leaves helps relieve pain.
- To relieve inflammation and pain, take baths in pine decoction. It is diluted with water, and then the affected knee is lowered into it for 20 minutes.
Freshly squeezed grapefruit juice has an excellent healing effect. It is recommended to drink it for knee bursitis three times a day, half a glass.
Before using this or that treatment method, you should consult your doctor about this.
How to treat at home
Before the development of the pharmaceutical industry, people knew how to treat bursitis without pills and other drugs. Several recipes with proven effectiveness have survived to this day.
Symptoms of bursitis can be relieved using traditional medicine. Painkillers are most often used. But it is also possible to cure bursitis using traditional methods if this disease is still in the initial stages of its development. And to prevent the process from progressing to surgery, the symptoms of bursitis should be eliminated in time.
Treating bursitis at home:
compresses from garden vegetables (mainly those that grow underground) at night;- infusion of propolis (10 g of propolis, pour 100 g of vodka, leave for five days);
- bath of pine needles (collect needles, soak, boil, then let steep for 12 hours).
In any case, treatment for bursitis requires not only the use of traditional methods, but also a medicinal approach. Traditional medicine alone may not be enough.
Massage is never used for bursitis. Treating bursitis with this method may cause the infection to spread more and make the condition worse. And then the patient cannot avoid surgery.
Symptoms
An increase in body temperature is the first symptom of the onset of bursitis
Bursitis of the knee joint has a specific clinical picture. Its specific symptoms and signs reveal it. When they appear, it becomes clear that the person requires treatment.
As mentioned earlier, the chronic form of the disease is often asymptomatic. Pain during its development begins to bother a person only at the time of physical exertion and increased activity. Aggravated bursitis has a completely different clinical picture. The patient complains of swelling, pain and redness of the skin. The amount of synovial fluid also increases. Gradually, the bursa shell becomes denser. Cystic neoplasms begin to appear in the cavity, making it increasingly difficult for the knee to bend and straighten.
In the acute form of the disease, the symptoms of bursitis are pronounced. The patient complains of the following pathological conditions:
- Constant pain in the inflamed area;
- Painful swelling of the knee;
- Increased body temperature.
The pain may occasionally travel to other parts of the body, such as the feet or legs. In this condition, it is necessary to begin treatment immediately so as not to start the process and provoke the development of complications.
Only an experienced specialist can tell you how to properly treat bursitis of the knee joint in this case.
The subacute form of the pathology manifests itself during treatment therapy, as it is characterized by the reverse development of bursitis symptoms.
The symptoms of purulent bursitis do not go unnoticed by the patient due to the strong severity of their manifestations. A phenomenon such as this disease is accompanied by the following symptoms:
- Weakness;
- Chills;
- General malaise;
- Nausea;
- Migraine;
- Lack of interest in food;
- Feverish condition.
If a patient with purulent bursitis of the knee joint is not provided with urgent medical care, his condition will continue to rapidly deteriorate.
Complications
Regardless of the cause of the development of bursitis, this disease, despite its apparent simplicity, can be quite dangerous in terms of its complications.
Complications of bursitis:
development of ankylosis in the joint;- adhesive process in the joint capsule;
- osteoarthritis;
- osteomyelitis.
Treatment of bursitis should be timely and complete. Because the symptoms of the disease can be stopped quickly, but dealing with complications is quite difficult.
Achilles bursitis
Develops at the junction of the heel bone and tendon. The accumulated exudate causes compaction of the surrounding tissues, and the motor activity of the joint is partially lost. It is often combined with other pathologies: heel spur, plantar fasciitis.
There is swelling in the heel area, patients complain of pain spreading higher to the calf muscle. When you try to stand on your toes or lean on your heel, the pain intensifies and movements in the ankle become difficult.
Untimely treatment leads to complications: the formation of pus, rupture of the Achilles tendon, phlegmon, sepsis. If there is no effect from complex therapy, they resort to a surgical method, during which the damaged area of the bursa is excised.
Prognosis for recovery
After treatment of acute bursitis, if the therapy was successful, there are no visible pathological changes in the joint (all the same, micro damage to the articular formations cannot be avoided). A sluggish chronic disease can leave behind clearly noticeable intra-articular adhesions and scars.
Bursitis is a disease that does not go away completely without a trace. Regardless of what the cause of the disease was (metabolic disease or injury), the damaging factor has already caused harm to the joint elements.
To avoid inflammation of the joint capsule, it is necessary to promptly sanitize existing foci of infection and prevent injury to the joint. Professional athletes, in whom the incidence of the disease is significantly higher than in the population, should rationally dose the load on the joint and, if necessary, use elastic bandaging.
General information about the disease
The knee joint is one of the most loaded joints, therefore it often suffers from various pathologies
The joint capsule is directly involved in the activity of the knee joint. It looks like a pocket. The bursa protects the joint from mechanical damage, due to which it may lose its functionality. The fluid that fills the synovial bursa facilitates its movement. If blood clots, pus or serous fluid form in one or more cavities, doctors diagnose a person with bursitis.
Knee bursitis is most often found in people who spend a lot of time on their feet.
This applies to service workers and athletes. In young children, the disease can develop due to a lack of certain vitamins and minerals in the body.
The disease has a place in the international classification ICD 10. It was assigned code M70.