In this article we will look at the reasons why fingers became crooked.
This phenomenon refers to a change in bone tissue or the shape of joints, resulting in a change in the configuration and direction of the bones. This pathology causes a person many different problems. If, for example, you have crooked toes, the load on the feet is distributed unevenly, as a result of which joint diseases begin to develop. Don’t underestimate the aesthetic component - your toes can be hidden from prying eyes, but a similar problem with your toes will not go unnoticed. If left untreated, this pathology can cause a complete loss of control of the hand. The most common problem in the field of orthopedics is curvature of the joints.
Diabetes
One of the complications of this pathology is neuropathy, which is manifested by damage to the nerve endings in the extremities. As a result, they experience a decrease in sensitivity. That is why a person does not pay attention if his shoes rub or something hurts his foot, he does not feel injuries or cuts. Dirt can penetrate into such wounds, after which the process of inflammation develops. That is, deformation of the fingers can be a consequence of neuropathy. Why else can your fingers become crooked?
Arthrosis
It is a chronic degenerative-dystrophic disease of the joints, in which destruction of cartilage occurs, the development of pathological changes in the capsule, ligamentous apparatus, synovial membrane, and nearby bone structures. The main reason for the development of arthrosis is a violation of metabolic processes. The pathology manifests itself as severe pain, stiffness in the morning, and limited mobility. In the absence of timely treatment, the pathology causes deformation of the hands and curvature of the little finger. Crooked fingers are very unsightly.
Psoriatic arthritis
It is a chronic joint disease that develops against the background of psoriasis. The pathology is characterized by asymmetrical damage to the joints, pronounced phenomena of secondary osteoarthritis, focal bone compactions, and marginal growths. During the development of the disease, a person often experiences subluxations and dislocations of the affected joints, and immobility of the distal joints between the phalanges of the toes and hands develops. In severe forms of the disease, bending of the toes behind each other is common.
Symptoms
The main sign of arthrosis of the fingers is the appearance of formations on the joints: Heberden's or Bouchard's nodes. Such growths cover the dorsal or lateral surface of the damaged joint, and most often Heberden's nodes are observed in areas close to the nail plate, and Bouchard's vesicles cover the area of the middle of the fingers. Almost always, nodules appear symmetrically on the fingers of both hands. The size of such formations varies from the size of a match head to the size of a pea.
During the development of such formations, the patient often experiences an unbearable burning sensation. The growth of nodules may be accompanied by throbbing pain, characteristic of the process of formation of purulent contents under the skin. After the bubble matures, it bursts and the liquid mass flows onto the surface of the skin. After a certain period of time after this, the pain subsides, the swelling disappears and the skin acquires a natural color.
In addition to the visual signs indicated above and the pain that constantly overcomes and intensifies with the acute development of inflammation - the addition of arthritis, the following symptoms may be observed. When the disease recurs, there is an increase in body temperature and signs of general intoxication of the body: headache, muscle weakness, fatigue, drowsiness.
As the disease worsens, the joints of the hand become increasingly deformed, and the fingers take on the appearance of hooks.
Rheumatoid arthritis
It is a chronic systemic autoimmune disease that affects joint structures. Any joint can become inflamed, but most often the small joints of the feet and hands are susceptible to pathology. Periodically, the disease worsens against the background of climate change, hypothermia, trauma, psycho-emotional stress, physical activity, infections, and concomitant pathologies. Often the development of rheumatoid arthritis is accompanied by damage to internal organs.
Crooked toes are usually the result of various pathologies:
- Atherosclerotic changes in the lower extremities. Atherosclerosis of the veins of the lower extremities is a pathology in which blood flow in the legs is completely or partially blocked. The reason for this phenomenon is blockage of blood vessels with blood clots and atherosclerotic plaques. As the pathology progresses, narrowing or complete blockage of the arteries occurs. As a result, the blood supply to the legs deteriorates, pain appears in the calves when walking, discomfort occurs at night, and the little finger becomes deformed. Why do you still have crooked toes?
- Flat feet. The foot of people with this disease lengthens, causing the flexor muscles to begin to overpower the extensor muscles. As a result, the tendons become even tighter and cause deformation of the fingers. Crossed fingers with flat feet are a common occurrence.
- Gout. It is a chronic progressive pathology, which is characterized by disturbances in purine metabolism, excess uric acid in the blood, recurrent arthritis, and deposition of uric acid salts in tissues. In the vast majority of cases, gout affects the joints of the thumbs and index fingers, and less commonly, the joints of the knee and ankle. Gout is accompanied by severe sharp pain in the affected joint, the development of severe swelling, and the appearance of redness. As the pathology develops, persistent curvature of the joints occurs and motor volume is impaired.
Diagnostics
As a rule, any deformation changes in the hands can be identified during examination. However, the signs of arthritis and arthrosis are very similar to each other, so additional studies are often prescribed, including:
- Blood test (for the presence/absence of inflammatory processes, detection of uric acid levels).
- Analysis of urine.
- X-ray. The image will show in detail articular deformations and osteophyte formations.
Diagnostic manipulations also have a wider range, depending on the characteristics of the genesis of the disease being studied.
Types of deformities on the legs
Curvature of the toes can be of the following types.
- Taylor's deformity. This deformity is often called “tailor’s foot.” With this disorder, the lateral part of the foot increases, and varus deviation of the last toe is observed. The disease is characterized by inflammation of the fifth metatarsophalangeal joint. Factors contributing to the development of Taylor deformity are congenital disorders of the ligamentous apparatus, injuries.
- Claw-shaped deformity. In this case, all toes are affected except the big toe. The fingers begin to curl downward, resembling the claws of an animal. This deformity develops as a result of disturbances in the activity of the muscle system. Cerebral palsy, injuries, and flat feet can contribute to the development of this pathology.
- Hammer deformity. Typically affects the index toes. They begin to bend, after which they are fixed at a certain angle. The patient experiences severe pain. This deformity occurs mainly due to a genetic predisposition in people with long metatarsal bones. The risk group includes people who have been diagnosed with progressive transverse flatfoot. People often have a crooked thumb.
- Valgus deformity. It affects the big toes and is characterized by the formation of a bone growth at the base of the big toes. As this disease develops, the arches of the feet become flattened and the first metatarsal bone deviates inward. Along with the formation of growths, corns form and the development of hammer-shaped deformities of the index, middle, and ring fingers occurs.
A crooked index finger is also not uncommon.
What causes arthrosis of the fingers
The first and main reason for the development of the disease is genetic predisposition. If the patient’s parents or grandparents had fingers affected by arthrosis, such a person should take care of the health and beauty of his hands from his youth.
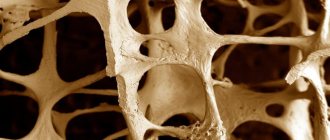
However, it is not arthrosis itself that is inherited, but the structure and density of cartilage tissue and bones; metabolic features.
Another reason why bone destruction can occur is excessive stress on the fingers. The group at increased risk of the disease includes people in the following professions: pianists, massage therapists, office workers who type large amounts of text on the computer every day.
Note! Arthrosis of the fingers can be triggered by diabetes mellitus, endocrine system disorders and other pathological metabolic processes. Menopause (hormonal disorders in women during menopause) causes the body to actively lose moisture, along with a decrease in estrogen levels.
This causes cartilage tissue to become thinner and bones and joints to become more fragile.
Menopause (hormonal disorders in women during menopause) causes the body to actively lose moisture, along with a decrease in estrogen levels. Because of this, cartilage tissue becomes thinner and bones and joints become more fragile.
The most common cause of arthrosis is injuries to the wrist joints and phalanges of the fingers. It is especially dangerous when inflammatory processes develop after injuries.
On hands
Finger deformities are of the following types:
- Swan neck. This deformity is characterized by excessive extension of the fingers in the middle joint and flexion in the upper joint. The thumb has only one interphalangeal joint, so this deformity does not affect the thumbs. However, the development of severe hyperextension of the interphalangeal joint of the thumb can cause a rectangular or zigzag deformity. There are crooked and middle fingers.
- Button loop. With this type of deformity, the finger is bent at the middle joint, but straightened at the top. This deformity develops as a result of rheumatoid arthritis, osteoarthritis, dislocation, or tendon rupture.
- Hammer deformity. It is an injury to the tendon that straightens the nail phalanx of the finger. With this deformation, the nail phalanx bends towards the palm. The disorder is characterized by a lack of active extension function of the upper joint.
What to do when your finger becomes crooked?
Valgus deviation of 1 finger - symptoms and treatment
Treatment of hallux valgus should begin with the selection of comfortable shoes , orthopedic insoles and exercises to strengthen the muscles. Often, standard orthotics do not help stop the deformity and relieve pain, so it is important to use insoles made individually for the patient.
To prevent and treat the disease, the doctor may recommend a valgus hinge splint - a fixator that holds the joint in its normal position. To reduce inflammation and relieve pain, nonsteroidal anti-inflammatory drugs (for example, celecoxib, ketoprofen) are prescribed [12].
Non-surgical treatment may relieve symptoms but will not correct the foot deformity. Therefore, if pain persists, surgery . The search for effective treatment methods began in the 19th century and, according to various authors, there are from 200 to 500 different surgical techniques [13]. However, the problem is still relevant: surgery brings temporary relief, but does not eliminate the cause - weakness of the muscular system of the foot. All existing methods of foot surgery can be divided into two types: on soft tissues and on bones. The decision about which surgical technique is used depends on the degree of deformity, degenerative changes in the joint, and the shape and size of the metatarsal. Surgeries on soft tissues are recommended for mild to moderate lesions. In severe stages of deformation, there is a need to restore bone structures; for this purpose, osteotomy is used (Latin osteotomia - bone dissection).
The generally accepted method of surgical treatment of hallux valgus is the original McBride technique, created in 1928. Later, the method was improved by various authors, which made it possible to reduce the trauma of the operation and improve its results. The McBride procedure involves passing and fixing the adductor pollicis tendon through a hole in the metatarsal bone. This method is a special case of myotenoplasty (muscle and tendon transfer) and refers to operations performed on soft tissues. In some cases, the McBride operation may be supplemented with osteotomy[3][5][13].
Stages of forefoot reconstruction surgery using myotenoplasty:
1. Feet before surgery.
2. Isolation of the tendon of the muscle that abducts the first finger.
3. Removal of the head of the first metatarsal bone (Sade's operation).
4. Creation of a channel for the tendon of the muscle that abducts the first finger.
5. Passage into the canal of the tendon of the muscle that abducts the first finger.
6. Proximal wedge osteotomy.
7. Osteosynthesis (connection) of bone fragments of the first metatarsal bone.
8. Creating a screed.
9. Feet immediately after surgery.
The patient is usually discharged from the hospital less than a week after the operation. The sutures are removed after 12-14 days. After the operation, the patient uses Baruk orthopedic shoes with a wedge-shaped sole for a month to unload the forefoot. It is worn from two to eight weeks, depending on the complexity of the operation.
On average, after two months the patient can wear regular shoes and returns to his normal lifestyle. However, until six months after the operation, it is undesirable to wear shoes with heels more than three centimeters. To prevent relapses, you should wear insoles. Conclusions about the success of the operation can be made after three to four months (in severe cases - after six months) based on control X-ray images.
Therapy for deformed fingers
Therapy for curvature of the fingers involves complexity and consists of exercise therapy, physiotherapy, the use of medications and the use of orthopedic devices.
The main goal of drug treatment is symptom therapy, that is, pain relief, elimination of inflammation, swelling, normalization of metabolic processes and blood supply to joint structures. The following medications are indicated for use:
- Anesthetics (“Analgin”, “Baralgin”, others).
- Muscle relaxants: “Sidalud”, “Mydocalm”. These drugs help relieve spasms, minimize muscle pain, and normalize blood circulation.
- Non-steroidal anti-inflammatory drugs: Piroxicam, Ketorolac, Ibuprofen. These medications help reduce pain and relieve inflammation.
Treatment of arthrosis using alternative medicine methods
Before you start using infusions, baths and compresses, you must consult your doctor, make sure that the ingredients used are safe and of good quality, and rule out allergic reactions to the components.
- Table salt and honey must be mixed in equal proportions until a homogeneous paste is obtained. The mixture is used for compresses on sore joints (at night).
- Clay applications provide good results. They improve the quality of cartilage tissue and skin condition.
- An infusion prepared from the string is used as a wound-healing and anti-inflammatory agent. 2 tablespoons of dry raw materials are poured with a glass of boiling water and left for 20 minutes. Drink the strained tincture 2 tbsp. spoons 3 times a day. Treatment lasts 1 month.
- Chopped horseradish in the amount of 40 g. mixed with Vaseline (50 g.) This composition is used to lubricate sore joints. Treatment helps reduce finger pain and inflammation.
- Burdock leaves are twisted with a meat grinder and applied fresh to the fingers, the compress is insulated.
- Teas made from rosehip, mint, lingonberry, and thyme are good for arthrosis.
- Lump chalk is crushed and a small amount of kefir is added to it (to the consistency of thick sour cream), and applied as a compress to the finger joints overnight.
Use of orthopedic devices
When using orthopedic devices, the load on the affected joints is reduced and the likelihood of additional injury is eliminated. An orthopedist will help you choose special shoes, braces, and various devices. If the disease is at an early stage of development, wearing wide, soft shoes may be effective.
The curvature of the index toe can be corrected by using arch supports and special insoles.
If we consider the curvature of the fingers, then, as a rule, it is sufficient to apply a special splint to the upper joint. You should wear this splint for up to 8 weeks; after removing it, you will need to gradually restore joint mobility.
Surgical methods
Surgical correction methods can only be used for fixed deformities if conservative therapy does not produce the expected results. The following operations are performed for curvature of fingers.
- Removal of bursitis.
- Distal osteotomy (in which the doctor reduces the angle between the bones by cutting the distal edge and then moving it to the lateral plane).
- Installation of implants.
- Arthrodesis (artificial joint immobilization).
- Resection and subsequent replacement of soft tissues located near the affected joint.
- Resection arthroplasty (removal of the end portion of the metatarsal bone).
- Exostectomy (excision of the upper part of the metatarsal bone).
It should be noted that surgery aimed at eliminating finger deformities will require subsequent rehabilitation, which will take about two months.