Every 3rd patient who comes to a rheumatologist with a complaint of joint inflammation, according to statistics, suffers from infectious arthritis. This disease requires immediate consultation with a doctor, because it can completely and irreversibly destroy a joint in a couple of days, and every 12th of those who are unlucky enough to get the disease die every year from its complications. But if you go to the hospital in a timely manner, 70% of patients get off with a “mild fright” - modern medicine allows you to save joints from deformation in most cases.
Let's look at the symptoms and treatment of infectious arthritis.
Infectious arthritis: causes, mechanism, complications
What is infectious arthritis? Infectious arthritis is an acute or chronic inflammation that occurs in the joint capsule due to bacterial or viral infection. Infection (gonococcal or non-gonococcal) can develop in the synovium, synovial fluid and soft tissue adjacent to the joint. The incubation period usually varies from several hours to several days (usually no more than 10).
Many pathogenic microorganisms produce so-called adhesive proteins and acids that help them attach to articular surfaces for further reproduction. These substances actually “eat away” the cartilage - the initial erosion develops into irreversible changes as the number of microorganisms increases. In addition to poor nutrition, the joint suffers from enzymes with which the human body tries to cope with bacterial agents - by “dissolving” foreign cells, these proteins damage the synovial fluid, ligaments and the cartilage itself.
What are the causes of the disease? The cause of the disease in children and adults is gram-negative and gram-positive bacteria - staphylococci, streptococci, gonococci, HIV, parvoviruses, spirochetes. Diseases such as rubella, mumps, hepatitis, dysentery, brucellosis, and borelliosis can provoke infection of the joint and an acute form of arthritis. Tuberculosis, mycosis and a number of other diseases often lead to a chronic, sluggish form.
People with rheumatoid and other types of arthritis and arthrosis, gout, joint prostheses, people over 60 years of age, and those addicted to injecting drugs or alcohol are especially susceptible to the disease. Risk factors also include recent surgery, immunosuppressive therapy, skin infections, the presence of bacteria in the blood (bacteremia), chronic diseases of the lungs, liver, kidneys (especially those requiring hemodialysis), cancer, diabetes, sexually transmitted diseases and a number of systemic diseases .
What complications occur with infectious arthritis? Almost a quarter of patients affected by infectious arthritis complain of partial or complete limitation of mobility in the affected joints.
Left untreated, this disease can provoke a purulent and even necrotic process in the bone and adjacent soft tissues. If the septic process spreads to the bone marrow, inflammation of the spinal column may develop. This is fraught with destruction of the vertebrae. The relatively high percentage of deaths in infectious arthritis is explained by severe intoxication of the body, septic shock and the possible development of respiratory failure.
3. Symptoms and treatment of the disease
Symptoms of osteomyelitis
Acute osteomyelitis develops quickly, within 7-10 days. Symptoms of acute and chronic osteomyelitis are very similar and include:
- High temperature, irritability, fatigue;
- Nausea;
- Tenderness and swelling around the affected bone;
- Decreased range of motion.
- Vertebral osteomyelitis often causes severe back pain, especially at night.
Treatment of osteomyelitis
Diagnosis of osteomyelitis
is the first step towards treating this disease.
And this is a very difficult process. X-rays, blood tests, and bone scans
may be used to diagnose osteomyelitis .
In addition, the doctor must determine the type of microorganism (usually a bacterium) that caused the infection
. This is necessary in order to choose the right medicine. Most cases of osteomyelitis are treated with antibiotics, surgery, or both.
Antibiotics
help control infection and often avoid surgery. For patients with osteomyelitis, antibiotics are usually given through an IV for several weeks, followed by a course of antibiotic tablets.
In cases of severe or chronic osteomyelitis, surgery may be required to remove the affected tissue and bone
. Surgery in this case will help prevent further spread of the infection.
About our clinic Chistye Prudy metro station Medintercom page!
Symptoms of infectious arthritis
Infectious arthritis is characterized by suddenness: pain appears unexpectedly, as if out of nowhere, and extremely intensely signals the onset of the disease. Almost immediately, stiffness sets in in movements - both active (using only muscles) and passive (produced with the help of hands or other aids). Typically, the first symptoms of infectious arthritis are observed in only one joint, with the possibility of spreading to others. But with blood diseases, viruses, gonococcal infections, polyarthritis is possible, in which symptoms are observed in several joints at the same time.
The main signs of infectious arthritis are:
- redness of the skin over the joint, local or general increase in body temperature;
- pain when touching the joint;
- accumulation of fluid in adjacent tissues caused by an inflammatory process;
- a sharp deterioration in mobility (the joint moves tightly, even if you bend it with your hand);
- fever, chills.
Specific symptoms and treatment for infectious arthritis vary depending on the pathogen. Gonococcal arthritis may be accompanied by ulcerative rashes on the skin and mucous membranes, in the mouth or in the genital area. If infection occurs through a bite, the lymph nodes usually become enlarged. Fungal infections of the joints can occur without fever or other systemic manifestations.
The disease is usually localized in the shoulder, elbow, wrist and interphalangeal joints, as well as in the knee and hip joints. Certain diseases can “select” specific joints - for example, borelliosis most often affects the knees.
Bone pain due to osteoporosis
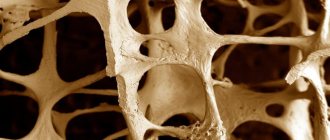
Osteoporosis is a disease that leads to the destruction of bone tissue, the first sign of which is bone pain. Its cause is metabolic disorders, so for bone pain of unknown origin, the diagnosis can be clarified using blood tests.
Where does calcium go?
Bone consists of a mesh protein “skeleton”, in the cells of which calcium and phosphorus salts are deposited. This is precisely what explains its strength: if the bone were simply hard, it would be as fragile as porcelain, but the protein base gives it the necessary flexibility. In the process of human development - starting from the prenatal period - a flexible “matrix” of the future bone is first formed, and it is filled with calcium later. The level of calcium saturation in bone varies at different periods of life. Why does this depend?
The thing is, keeping our skeletons strong isn't calcium's only concern. It is necessary for muscle contraction, including the heart. Therefore, a decrease in the level of calcium in the blood below a certain “subsistence level” is quite rightly considered by the body as a life-threatening situation. And the skeleton is a huge “reserve” of calcium, from which it can be taken if necessary.
Acute infectious arthritis
The acute form is observed in 95% of cases recorded by doctors. Unlike chronic arthritis, which affects people at risk, even absolutely healthy young people are not immune from it. Acute infectious arthritis, the most dangerous form of the disease, is characterized by severe swelling and heat in the affected joint. Erythrematous skin lesions against the background of other symptoms are a clear reason to call an ambulance.
You should also immediately consult a doctor if signs of arthritis are observed within 2-10 days after being bitten by dogs, cats, rats and other animals, as well as humans. Infections of the digestive tract are also dangerous. Nongonococcal reactive arthritis, which they can provoke, leads to joint destruction within the first hours after the onset of the disease!
Gonococcal infection, which is transmitted from mother to child, between sexual partners, as well as through household contacts, is less dangerous. However, the presence of concomitant diseases (for example, rheumatoid arthritis or systemic lupus erythematosus) significantly worsens the clinical prognosis in acute infectious arthritis.
Infectious arthritis in children
Infectious arthritis occurs in every 5-10 children, girls are especially vulnerable to the disease. In patients under 16 years of age, the disease is often accompanied by loss of appetite, increased irritability, temperature from 37.1 to 38 ° C (sometimes higher), and there may be complaints that the limb is as if paralyzed. Sometimes the disease is hidden and makes itself felt only by minor pain, lameness, and allergic rashes, for which there are other explanations. If a child is atypically lethargic, losing weight, gets tired quickly, or “pulls” a limb, this is a reason for an immediate examination!
Infectious arthritis can result from congenital infections (eg, staphylococcal infections). Children under one year old become inactive, are not interested in food, and avoid putting stress on the affected joints. They behave more cautiously or, on the contrary, restlessly, and begin to whine when touching the sore joint.
More than half of children suffering from infectious arthritis are under 3 years of age—particularly vulnerable to bacterial, viral, and fungal infections.
In no case should you neglect vaccinating children against influenza (Pfeiffer bacillus) and pneumococcus - it helps reduce the risk of infectious arthritis several times. Young children are especially susceptible to staphylococci, streptococci and gram-negative bacteria.
Please note: infectious arthritis in children can develop due to hypothermia, high physical activity, taking glucocorticosteroids and other drugs, as well as post-vaccination complications.
If left untreated, infectious arthritis can leave a minor with lifelong disabilities, especially if there are genetic disorders of the immune system.
Treatment of infectious arthritis
Treatment of infectious arthritis depends on several parameters: the form of the disease, the causative agent and concomitant diseases. If necessary, treatment of complications is carried out.
Self-medication for this disease is strictly contraindicated, since it is impossible to determine the cause of arthritis without special laboratory tests - highly specialized drug therapy is required.
Diagnosis of infectious arthritis
Diagnosis relies on symptoms of infectious arthritis (eg, pathological changes in the tissue around the affected joint). Why does a doctor determine whether the infectious agent is actually in the joint, blood or adjacent tissues, and determines the infectious agent. This is necessary for the correct choice of antibiotic: if the bacterium or a specific strain turns out to be insensitive to the drug, precious time will be lost.
For example, an ultrasound examination of a joint helps a specialist determine the presence of effusion in the joint and lesions.
To identify the causative agent, leukocyte and bacteriological analysis of the joint fluid is performed, which makes it possible to determine the presence or absence of pathogenic microorganisms. After laboratory culture, with a high probability, the type of pathogen will be established - unless it is gonococcus, Borrelia spirochete or treponema (the causative agent of syphilis), since they are difficult to detect in joint material.
A general blood test (helps to detect bacteremia), ESR, PCR, and, less commonly, examination of urine, sputum or cerebrospinal fluid are also performed. To achieve this, minimally invasive interventions are performed - for example, taking blood from a vein or puncturing a joint. An x-ray is prescribed last - it allows you to evaluate the destruction of the joint and bone heads caused by the disease, determine the narrowing of the joint space and other deformities.
Taking an anamnesis plays an important role in determining the symptoms and treatment of infectious arthritis - it helps to establish the possible cause of the disease at the pre-laboratory stage and eliminate unnecessary studies.
Taking antibiotics to a patient (for self-medication or treatment of a primary disease) can significantly complicate diagnosis.
Drug treatment of infectious arthritis
Sometimes treatment with broad-spectrum antibiotics is prescribed even before the pathogen is identified (usually penicillin, cephalosporins). For children under 3 months of age, initial therapy is with antibiotics active against gram-positive bacteria.
The drugs are administered intravenously (2-4 weeks) and then orally (another 2-6 weeks). In urgent cases, injections directly into the diseased joint are possible. A combination of various antibiotics is possible (for example, for tuberculosis), as well as intravenous and oral use of various drugs simultaneously. With the correct selection of antibiotics, improvement is observed already in the first 2 days of treatment.
In case of fungal infection, antimycotic agents are prescribed. In case of parasitic - antiparasitic. For some diseases, special chemotherapy or antiallergic treatment is performed.
If the cause of arthritis is a viral infection, instead of specific treatment, symptomatic treatment is carried out, aimed at eliminating fever, pain (analgesics, non-steroidal anti-inflammatory drugs), maintaining cartilage tissue (chondroprotectors and other similar drugs). Immunostimulating therapy is possible only as prescribed by a doctor and is completely contraindicated in rheumatoid arthritis.
Non-drug treatment
In the presence of a purulent process, the accumulated exudate is removed using a drainage tube or pumped out through a needle once a day, sometimes rinsing with saline solution is carried out. In difficult cases, when it is impossible to remove pus in this way (for example, due to bone growths), surgical intervention is possible. If the joint is severely damaged, prosthetics are performed. In some cases, arthroplasty, arthrolysis, and synovectomy are prescribed.
To ensure that the joints do not lose mobility, patients undergo physical therapy (for example, medicinal electrophoresis, compresses, amplipulse, magnetic therapy), and are prescribed therapeutic exercises - strictly under the supervision of an instructor. The complex includes active and passive exercises that help avoid contractures. Strength exercises shouldn't hurt.
In the acute stage of the disease, massage and physical therapy are contraindicated. In the early stages of the disease, it is recommended to limit joint mobility using a splint or splint. Clinical recommendations for infectious arthritis include timely treatment of systemic and local infections, chronic diseases, as well as compliance with the rules for surgical interventions.
You may be interested in:
Osteoarthritis of the knee joint Osteochondrosis of the knee joint, or what to do when your knees hurt? Reactive arthritis is a disease of young people Osteochondrosis of the lumbar region Osteoarthritis of the elbow joint
Approaches to the treatment of purulent-inflammatory diseases of large joints
Dear visitors of our site! This article is devoted to the surgical treatment of purulent-inflammatory diseases of the joints, complicated by the destruction of bone tissue (osteomyelitis), and purulent complications of endoprosthetics.
This group of diseases is a serious, unresolved problem in modern orthopedics. There are no uniform standards for the treatment of this pathology. Treatment approaches are based on the personal experience of individual authors and clinics. We would like to highlight the fundamental aspects of diagnosing this group of diseases and share our personal experience of their treatment.
The incidence of septic arthritis ranges from 2 to 10 cases per 100,000 population. The predominant lesion is the knee joint (up to 55%), followed by the hip and ankle joints. Mostly children and the elderly suffer from such diseases.
What are the prerequisites for the development of purulent arthritis? These are injuries to the joint area, degenerative and rheumatoid diseases of the joints, injections in the joint area, arthroscopic interventions, a history of joint replacement, purulent-inflammatory diseases, trophic ulcers of the distal extremities, sexually transmitted infections, systemic administration of glucocorticoids.
Clinical picture of the disease. Manifestations of the disease are quite distinct when joints close to the skin are affected (elbow, knee, ankle). This is tissue swelling in the joint area, local redness and increased skin temperature. When large, deep-lying joints, such as the shoulder and hip, are affected, local changes may not be pronounced, and the patient will only be bothered by pain in the joint area. An increase in body temperature may also not appear immediately. The photograph below shows a typical clinical picture of arthritis of the knee joint: the contours of the right knee joint are smoothed, the joint is increased in volume.
Laboratory diagnosis of the disease. The examination of a patient with a suspected purulent process must necessarily include a clinical blood test with calculation of the leukocyte formula and erythrocyte sedimentation rate, and a blood test for C-reactive protein. Among the laboratory indicators, I would like to dwell specifically on the level of procalcitonin. The procalcitonin test is currently the most objective method for determining the generalization of a bacterial infectious process. A dynamic increase in this indicator in the patient’s blood tests is an indicator of the spread of the purulent process beyond the joint and the development of sepsis.
Instrumental diagnostics: - radiography of the affected joint; — spiral computed tomography of the joint; - joint puncture followed by microscopy and culture of the discharge to determine the infectious agent and its sensitivity to antibiotics. This manipulation must be performed before starting antibiotic therapy.
Treatment. In the treatment of purulent-inflammatory diseases of the joints, our task is to quickly stop the inflammatory process and, if possible, preserve the function of the joint. According to various authors, during a purulent process in the joint, the articular cartilage is affected 4–6 days from the onset of the disease and finally dies off in the 4th week of the disease, after which the effectiveness of joint-preserving operations sharply decreases. In the absence of signs of bone tissue damage, preference is currently given to operations that preserve the joint. If superficial joints are affected in the early stages of the disease, it is possible to use puncture methods and broad-spectrum antibiotic therapy. If puncture methods are ineffective, drainage of the joint is recommended within 48 hours from the onset of the disease. Ideally—most modern authors tend to do this—the use of arthroscopic techniques.
Our personal experience: treatment of septic arthritis of the ankle joint in a 19-year-old patient through 3 weeks of flow-through drainage. The flushing system was installed through accesses up to 2 cm. The result of treatment was complete relief of the inflammatory process and recovery of the patient. During two years of follow-up, no relapse of the disease was noted. When the purulent process spreads to the bone tissue, non-viable tissue is removed and the joint area is stabilized using an external fixation device. As a result, the inflammatory process is stopped and arthrodesis of the affected joint is formed, that is, fusion between the bones that form the joint, which subsequently ensures adequate supporting function of the limb.
Personal experience: An 81-year-old patient was admitted to the clinic with pain in the hip joint that had been bothering her for 4 months after falling from a height. During the week before admission to the clinic, the pain steadily increased, and the supporting function of the limb was impaired. She did not notice any increase in body temperature; she constantly took anti-inflammatory drugs (Movalis) in large doses.
X-ray upon admission.
Zones of destruction are identified in the body of the ilium and in the head of the femur.
Puncture of the hip joint reveals thick purulent contents.
The patient underwent emergency surgery: the joint was opened, the focus of osteomyelitis was sanitized, the head of the femur was removed, the joint was fixed with a rod-based extrafocal device. A flow-through drainage system has been installed. The patient was treated with broad-spectrum antibiotics for 6 weeks. During treatment, pain in the hip joint was relieved, and clinical and laboratory tests showed a decrease in the inflammatory response.
The external fixation device was removed 8 weeks after surgery. The hip joint is fixed with an orthopedic fixator. 3 months after surgery, the fixator was removed. The patient walks independently with full weight bearing on the operated leg. The inflammatory process has been stopped.
Results of spiral computed tomography of the patient’s pelvic bones 3 months after surgery.
Signs of the formation of a fusion between the femur and the body of the ilium are determined. This fusion ensures adequate support function of the limb in the future.
Currently, a serious problem in modern orthopedics is purulent complications of endoprosthetics . According to CITO data for 2012, 80,000 endoprosthetics of large joints were performed in Russia. The ratio of primary and revision endoprosthetics was 9:1. The complication rate for primary arthroplasty of large joints was 2.4%. Of these, 40.6% are infectious complications. The rate of complications during revision arthroplasty was 12.9%. Of these, 51.4% are infectious complications.
In case of early deep suppuration after hip replacement, it is possible to preserve the endoprosthesis . Chronic infection of the endoprosthesis area and destructive osteomyelitis in adults, which developed against the background of septic arthritis, are indications for radical surgical sanitation, removal of endoprosthesis components and necrotic areas of bone tissue.
Approaches to performing operations for suppuration of endoprostheses vary. In our practice, we use articulating spacers (temporary “substitutes” for the prosthesis) - individually made from bone cement with the addition of antibiotics. The use of these devices allows you to maintain limb length, ensure walking with support on the operated leg, improve the patient’s quality of life in the postoperative period, and facilitate subsequent re-endoprosthetics .
Clinical example: Patient 65 years old. History of total hip replacement performed abroad in 2002. No dynamic monitoring of the joint was carried out. Over the past two years, since 2012, I have been experiencing periodic pain in the hip joint. Since September 2013, over the course of 3 months, he has noticed a gradual increase in pain. Two weeks before admission to the clinic, massage of the joint area and acupuncture were performed at home. After a course of these procedures, a sharp increase in pain and a rise in body temperature to 39 degrees were noted.
Radiographs of the patient upon admission.
Signs of destruction of the acetabular component of the prosthesis, signs of destruction of bone tissue along the femoral component of the prosthesis are determined.
During puncture of the joint, thick purulent contents were obtained. The joint cavity was opened, the components of the endoprosthesis were removed, and the osteomyelitis lesion was radically treated. During the inspection, purulent melting of the proximal femur was revealed. An articulating spacer is installed.
X-ray of the patient after surgery.
The model of the proximal femur is formed from bone cement with antibiotics, reinforced with a proximal femoral rod.
The postoperative course is smooth. The inflammatory process has been stopped. Re-endoprosthetics is planned. This clinical example clearly demonstrates the need for timely contact with a specialist traumatologist - orthopedist and the inadmissibility of performing physiotherapeutic procedures without preliminary adequate diagnosis of the cause of pain in the joints.
The Orthocenter specialists are proficient in all methods of surgical treatment of purulent-inflammatory joint diseases and are ready to come to your aid.