Osgood-Schlatter disease is a traction injury to the apophysis of the tibial tuberosity (hereinafter referred to as the tibial tuberosity) due to constant loads on the secondary ossification point. Such loads are often found in sports when there is constant tension in the quadriceps femoris muscle. Avulsion (separation) of a fragment of the LBD can occur in the preossification phase or in the ossification phase of the secondary ossification point. Once avulsed, the bone or cartilage begins to grow, ossify, and enlarge. The intervening area may become fibrous and form a separate small bone, or even create an entire bony fusion with thickening of the LBD. Most often the disease occurs in boys. These traction apophysitises are probably among the most common overuse injuries in children and adolescents.
Anatomy
Tibial Tuberosity
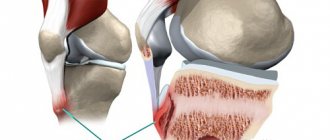
The tibial tubercle (TTU) is a large, elongated prominence on the superior anterior border of the tibia that is located slightly distal to the anterior surfaces of the medial and lateral tibial condyles. This area is the site of attachment of the patellar ligament. Tension in this muscle-tendon junction can cause pain and swelling. Mostly the pain occurs on one side, but often occurs on both sides.
Thus, Osgood-Schlatter disease is characterized by damage to the tibial tuberosity area and pain in the anterior knee joint.
Epidemiology/Etiology
In children and adolescents, there are growth plates in both the femur and tibia (endochondral bone/cartilage in the LBD area). This cartilage (flexible connective tissue that is often located between two bones), like bones, muscles and tendons, has the ability to grow. But during the growth spurt of adolescence, bones and cartilage grow much faster than muscles and tendons.
Slower lengthening of the quadriceps femoris muscle, which is the musculotendinous extensor apparatus of the knee joint, results in excessive tension where the patellar tendon attaches to the LCL. Because of this, microavulsions (microtears) of this zone may occur.
Tuberosity cartilage (the anterior part of the developing center of ossification of the LCL) can cope with the loads placed on it, but not in the same way as bone. Therefore, when a child or adolescent exercises, the stress on the patellar tendon and LBD increases, causing pain, irritation and, in some cases, microavulsions or avulsion fractures.
Increased tension at the musculotendinous junction of the patellar tendon and the ankle joint can cause the tendon to slightly pull away from the bone. Which, in turn, will increase the pain and cause swelling below the kneecap. This condition will be aggravated by activities that place greater stress on the patellar tendon, such as squats or jumping. In some cases, ossification may occur in the area of injury, which will lead to the appearance of a bony protrusion in the LBD area.
What is Osgood–Schlatter disease?
Schlatter's disease is a pathology caused by malnutrition of the knee joint area and accompanied by dystrophic changes in this area. This disease develops against the background of regular or sudden injury to bone tissue. As a rule, it manifests itself in men during the period of skeletal formation.
Clinical manifestations of the disease include: swelling in the immediate vicinity of the knee, the appearance of a compaction under it, the occurrence of noticeable discomfort in this area during exercise or in the absence of it.
Schlatter's disease was first mentioned by the surgeon O. M. Lannelong (France) in 1878. Later, the pathology was described in their works by specialists from the USA and Switzerland - R.B. Osgood and K. Schlatter. The disease is also called “Osteochondropathy of the knee joint”.
Clinic
The leading symptom of this disease is pain, which appears and intensifies during physical activity - running, jumping, cycling, kneeling, going up and down stairs, and hitting a ball (in the phase when the knee extends). Most often, pain intensifies when playing sports such as basketball, volleyball, football and tennis. Clinically, the disease manifests itself as pain localized in the LBD area. In some cases, there may be swelling and hypertrophy, as well as excessive tension in the quadriceps femoris muscle. Characteristics such as local fever and intra-articular edema are not important in this disease. There is rarely hyperthermia in this area, but swelling, tenderness and pain often occur.
Clinical symptoms include the following:
- pain on palpation of the LBD;
- pain in the tuberosity area, which intensifies after physical activity or sports;
- increasing pain when squatting, walking up stairs or jumping.
Stages and classification of osteochondropathy
When diagnosing osteochondropathy, the following classification is used: according to the degree of intensity, as well as according to the internal and external signs exhibited. In this regard, three stages of development of the disease are distinguished:
- Initial. It is characterized by episodic or mild pain that occurs in the knee area during sports activities. In this case, the compaction under the knee is not diagnosed;
- Increased symptoms. Swelling may occur in the affected area. The bone growth under the knee becomes visually noticeable. The appearance of discomfort is caused by excessive physical stress on the limb in the period after completion of sports training;
- Chronic. A lump-like growth is clearly visualized in the lower part of the knee, near which pronounced swelling is noted, and pain manifestations become long-term.
Diagnostics
X-ray of Osgood-Schlatter disease (lateral view)
The diagnosis is made based on the typical clinical findings described above.
X-ray examinations of both knee joints should always be performed, both in anteroposterior and lateral projections, to exclude tumors, fractures, ruptures or infectious diseases.
A lateral radiograph usually shows a clearly visible LBD with an incorrectly formed ossification nucleus or a free bone fragment lying proximal to the tubercle. Imaging is also useful in excluding tuberosity epiphysiolysis or neoplastic disease.
Sonographic studies may also be used. With ultrasound it is possible to see the appearance of the cartilage and bone surface, the patellar tendon, soft tissue swelling in front of the tuberosity, as well as fragmentation in this area.
Carrying out an inspection
The diagnosis can be made based on the collected medical history and objective examination. Tenderness of the LBD area upon palpation, which intensifies during squats with weights or jumping, is a fairly characteristic symptom of Osgood-Schlatter disease.
Extending the knee bent at a right angle, during which the patient must overcome resistance, reproduces pain. At the same time, no pain occurs during the straight leg lift through resistance.
The Duncan-Ely test (Ely's test or Duncan-Ely), which detects excessive tension in the quadriceps femoris muscle, will be positive in all cases.
Duncan-El test - testing the rectus femoris muscle
Causes of Schlatter's disease
Most often, the activity of this pathological process is observed during puberty in boys, and is also observed in adolescents who engage in sports training on a regular basis.
Despite the fact that it is boys who are at risk and susceptible to Osgood-Schlatter disease, at the moment this disease is also diagnosed in the female half of humanity. Signs of the disease appear, as a rule, during the development of the skeleton and fade as its formation is completed.
About 20% of young men involved in sports are diagnosed with Osgood-Schlatter disease. For those who do not play sports, the incidence rate reaches only 5-6%.
Make an appointment Online booking
- Clinic on Krasnopresnenskaya +7 (499) 252-41-35 Volkov lane, 21
- Clinic on Varshavskaya +7 (499) 610-02-09 Varshavskoe highway, 75, building 1
- Clinic in Annino +7 (495) 388-08-08 Varshavskoe highway, 154, building 1
Treatment
Treatment should begin with resting the injured extremity (called the RICE technique: a four-part system of trauma care that includes Rest, Ice, Compression, and Elevation), making changes to a regimen of physical activity and, in some cases, the use of NSAIDs.
Physical therapy
The physical therapist should focus on exercises that improve the elasticity and strength of the muscles surrounding the LCL. These include the quadriceps femoris, hamstrings, iliotibial tract and gastrocnemius muscles.
Friends, this and other questions will be discussed in detail at the seminar “Diagnostics and treatment of problems in the joints of the lower extremities.” Find out more...
At the beginning of therapy, high-intensity exercises for the quadriceps femoris should be avoided, as this will lead to increased pressure on the LCL area. Stretching exercises should initially be performed statically and at low intensity so as not to provoke pain. In the future, stretching exercises can be performed in a dynamic mode or using the PNF technique. To increase range of motion, it is recommended to perform exercises at least once a day, 3 times for 30 seconds. Quadriceps strengthening exercises can include moderate-intensity isometric exercises performed at different angles.
High-intensity quadriceps strengthening exercises and hamstring stretches should be gradually incorporated into the program. Their effectiveness has been confirmed by research (level of evidence Ia).
Shock wave therapy
The effectiveness of shock wave therapy in the treatment of Osgood-Schlatter disease is currently under debate. However, due to the low evidence base, this method cannot be clearly recommended (level of evidence IV).
Activity Limit
Conservative treatment for this condition is based on the same principles that apply to all overuse injuries. The modern approach to the treatment of Osgood-Schlatter disease does not require complete immobilization of the patient, nor does it require a total refusal of sports activities. It is of great importance that the doctor inform the parents, coach and child about the natural course of the disease. The child should continue his usual activities to the extent that pain allows. Therefore, the intensity and frequency of exercise should be reduced (that is, adapted to the specific patient). As an addition to the main activities, swimming can be recommended, which usually does not cause discomfort.
Knee pads, tape, or elastic knee supports with an infrapatellar strap or pad may also be recommended. They may help with exercise and reduce pain (Evidence Level: V).
A study by Gerulis et al. (level of evidence: IIb) showed that limiting physical activity, adapting it to the patient's capabilities and conservative treatment together have a more powerful effect than simply reducing exercise without conservative therapy.
Taping
Knee taping according to McConnell
The McConnell knee taping technique has not been specifically studied for Osgood-Schlatter disease, but has been credited with improving knee flexion and reducing pain during activity (Evidence Level IIb).
Surgery
Surgery should be avoided until the child is older and bone growth is complete. This measure is necessary to prevent premature closure of the cartilaginous growth plate, recurvation and valgus of the knee joint.
Surgical interventions in the treatment of the disease include drilling of the LBP, its excision (reduction in size), a longitudinal incision in the patellar tendon, excision of unfused bones and loose pieces of cartilage (sequestrectomy), installation of bone pins, as well as a combination of these methods.
Symptoms taking into account the classification of Schlatter's disease
Schlatter's osteochondropathy is characterized by the following undesirable manifestations:
First stage. Characterized by the appearance of minor discomfort in the lower part of the knee. During visual diagnosis, lump-like growths are not diagnosed.
Second stage. Accompanied by the appearance of a small compaction under the knee, which rises against the background of other parts of the body. Over time, the pain syndrome intensifies.
Third degree. The pathology becomes chronic. Upon visual examination, you can notice a pineal formation under the knee, which causes discomfort in the patient. In addition, elevated temperatures are observed in this area. In some situations, motor activity in the joint may be impaired.
Forecast
As a rule, the symptoms of the disease subside within two years, and the prognosis is favorable in most cases. In summary, symptoms of Osgood-Schlatter disease are reduced and completely resolved in most patients if conservative treatments are used long enough, especially after bone growth stops (Evidence Level: IIIb).
Persistent symptoms are accompanied by the growth of a free bone fragment above the LCL or within the patellar ligament. In these cases, only surgical treatment will relieve symptoms (level of evidence: IV).
It is important to convince the patient that his condition is temporary.
Military service with Schlatter's disease
As you know, men in our country are drafted into the army at the age of 18. At this age, symptoms of this disease are not observed. Consequently, this pathology cannot become a reason for the release of young people from military duties.
In some cases, it is possible to delay conscription for medical reasons - due to the need for a medical course. A young man can be released from military service only in a situation where the pathological process has provoked a significant deterioration in the motor activity of the joint.