An intracerebral hematoma (ICH) is an accumulation of blood in a limited area of the brain substance that occurs due to a violation of the integrity of a cerebral vessel. The pathological condition is provoked by weak or injured intracerebral arteries or veins, which, having ruptured, began to release blood into the intracranial space. The VMH cavity can be filled with liquid or coagulated blood, or a bloody substance mixed with brain detritus (crushed fragments of brain tissue).
Schematic representation of a large hematoma.
Cerebral hematomas can be single or multiple, unilateral and bilateral, acute, subacute and chronic. They become chronic just 21 days after the hemorrhage occurs. Triggers of pathogenesis are often the consequences of arterial hypertension and atherosclerosis (70%-80% of cases), aneurysms and vascular malformations, mechanical intracranial damage due to TBI.
Intracerebral hematomas pose a serious threat to the health and life of the patient, since the structure-forming tissues of the brain at the site of the lesions are subject to compression, dislocation, edema and necrosis. Without adequate therapy, pathology can lead to severe morphological and functional brain damage, often irreversible. With ICH of any origin, the risks of disability and mortality are too high: disability affects up to 70% of surviving patients, the probability of death is 25%-50%.
General information
Head trauma occurs as a result of a fall, a blow to the head, road traffic accidents, or accidents during sports or work. The skull bones protect the brain from damage, and the meninges provide additional protection. In this regard, most bruises do not cause brain damage.
Head injuries that damage the brain are called traumatic brain injuries (TBI or neurotrauma). The most common type of TBI is mild (this includes mild brain contusion and concussion) - it accounts for 80% of cases. If there is damage to the substance of the brain, meninges, cranial nerves and blood vessels, the injury is regarded as moderate to severe and they account for 15% of cases. Not always even a mild traumatic brain injury goes away without a trace, and moderate and severe injuries cause disability and even death of the patient.
Severe neurotrauma includes severe brain contusion , intracranial hematomas (epidural, subdural and intracerebral), which occur in 40% of neurotraumas, and diffuse axonal damage. With hematomas and brain injuries, the mortality rate is 55%, and 29% of victims are disabled.
Pathogenesis
With any brain injury, hydrodynamic forces and a shock wave act on an important hypothalamic-reticular part of it. Therefore, the synthesis of catecholamines , autonomic and vascular disorders develop, as well as liquor hypertension . The acute period of brain injury is accompanied by oxidative stress, neuronal depolarization, autoimmune inflammation and cell damage. All these mechanisms cause the death of neurons and loss of connections between different parts of the central nervous system.
Primary brain damage entails secondary changes, which are divided into intracranial ( hemorrhage , ischemia , increased intracranial pressure , swelling and displacement of the brain, compression of cerebral vessels and their spasm , neuroinfection ) and extracranial (high or low blood pressure, disturbances in potassium and sodium levels). All severe bruises and compression of the brain are accompanied by ischemia of varying severity, which plays a significant role. It develops due to deterioration of blood flow in the brain and lack of oxygen in the blood. Vascular spasm aggravates ischemia , hypoxia and cerebral edema . Ischemia can be regional (due to brain dislocation and herniation) and local (occurs in the compression zone).
If we consider the mechanism of hematoma formation, they are formed when cerebral vessels rupture. Subdural hematomas are associated with venous damage and venous bleeding. The subdural veins, which connect the cerebral cortex with the venous sinuses, are damaged. With epidural hematomas, the source is the arteries of the membranes or veins damaged by the bones of the skull during their fractures. In young children, ruptures of the sinuses of the dura mater occur.
Treatment methods for intracerebral hematoma
Conservative therapy or neurosurgery are used to treat cerebral hematomas. Recommendations for conservative elimination of hematoma are:
- small size of the lesion (≤ 40 cubic cm) without pronounced symptoms, without clinical signs of herniation and dislocation;
- old age of the patient (75 years and older);
- inappropriateness of surgery due to the high risk of unfavorable outcome (for example, large-scale hemorrhage in the dominant hemisphere or with extensive neurological damage);
- severe condition of the blood coagulation system, sepsis;
- diabetes mellitus in the stage of decompensation, uncontrolled hypertension.
The problem is solved conservatively by competent neurologists and neuroreanimatologists. The treatment plan is developed strictly individually. It may involve basic anti-ischemic, antihypertensive treatment, reduction of cerebral edema with osmodiuretics, therapy with hemostatics and neuroprotectors.
Classification of head injuries
The classification of injuries is based on the degree of brain damage. According to the classification, traumatic brain injury includes:
- Brain concussion.
- Compression of the brain.
- Brain contusion (focal, which is divided according to severity, and diffuse - a synonym for diffuse axonal damage).
- Intracranial hematomas (epidural, subdural, intracerebral).
All TBIs are also divided into:
- Closed (these are primarily non-infected injuries, accounting for 75%).
- Open (these are primarily infected injuries, since they have an entrance gate for infection to penetrate into the skull).
With a closed injury, the integrity of the soft tissues or the integrity of the aponeurosis is not compromised. Open damage is accompanied by rupture of the aponeurosis and meninges. Fractures of the skull bones and base of the skull may also occur with bleeding and leakage of cerebrospinal fluid through the nasopharynx and nose, and the contents of the skull communicate with the external environment. Of course, under such conditions there is a risk of infection of the contents of the skull. Open TBI occurs in 30% of victims.
Brain injury can be primary - resulting from a blow or any other impact with a direct effect on the brain. Thus, traumatic hematomas , contusion and axonal . Primary injury results in immediate cell death or progressive cell death over time. Secondary injuries include injuries that develop without affecting the brain. These include hypoxia , hypotension , hypercapnia , electrolyte disturbances, fever , anemia , cerebral edema , increased intracranial pressure . To assess the severity of the injury and to predict its course, the following indicators are taken into account: duration of amnesia, duration of loss of consciousness, state of basic functions. It is known that the duration of loss of consciousness in the acute period reflects the severity of TBI:
- For mild severity, the duration is less than 20 minutes.
- For moderate cases, this time ranges from 20 minutes to 6 hours.
- For severe cases - 6 hours to two days.
- For extremely severe cases, this period is more than 48 hours.
Intracranial hematomas are divided into epidural and subdural based on localization. A high probability of hematomas is observed in elderly people after a fall, in alcoholics, and in cases of fractures of the skull bones in the locations of the venous sinuses and meningeal vessels.
Meninges of the brain: 1- bone of the calvarium; 2 - hard shell; 3 - arachnoid membrane; 4 - soft shell; 5 - gray matter of the brain; 6 - white matter of the brain.
Subdural hematoma of the brain
Accumulation of blood between the dura mater and the brain. Subdural hematomas are more common than epidural hematomas and are observed in the elderly and infants.
Subdural hematoma of the brain
Acute subdural hematoma is more common in severe TBI and manifests itself in the first three days. Bleeding comes from cerebral vessels damaged by a bruise or from torn veins. This type of hematoma manifests itself as loss of consciousness due to massive brain damage. The clear gap in the clinical course, characteristic of an epidural hematoma, is often absent. Subdurals are not limited to the sutures of the skull and are therefore more common. If the hematomas are small (up to 50 mm), they can resolve under the influence of treatment. In all other cases, surgical treatment is performed. ICD-10 code for subdural hematoma I60.
Chronic subdural hematoma is a massive hemorrhage that has a capsule and causes compression of the brain. These formations are detected weeks or months after the injury, especially in cases where minor head injuries have passed without symptoms and are unnoticed by the patient. Chronic subdural hematoma differs from acute and subacute ones by the presence of a capsule. Most often, this type occurs in older people with concomitant cerebral vascular pathology, diabetes mellitus and alcoholism . In these individuals, bilateral hematomas are often detected; they contain dark liquid in the amount of 50-250 ml (usually 100-150 ml). The development of these hematomas in young people and children cannot be ruled out.
A distinctive feature of this type of hematoma is a clear gap that lasts for weeks, months, or years. Then it manifests itself clinically - a compression syndrome may gradually develop, manifested by headaches, inappropriate behavior, changes in character, memory impairment, or the condition may sharply worsen (stupor, coma) under the influence of additional factors - overheating, colds, repeated trauma, alcohol consumption. Diagnosis of chronic subdural hematomas is difficult, since there is often no traumatic history, there is an atypical course, especially in elderly people, and there are no signs of brain dislocation.
Epidural hematoma of the brain
An accumulation of blood located between the bones of the skull and the dura mater.
In 95% of cases this is a unilateral formation, but there are bilateral and even multiple ones. If we consider the localization of this type of hematoma, then they (as their occurrence decreases) are located under the tentorium of the cerebellum, the temporo-parietal part, the frontal region, the parieto-occipital and in the posterior cranial fossa.
Types of epidural hematomas:
- acute (occurs in 57% of cases and develops due to arterial bleeding );
- subacute (occurs in 32%);
- chronic (occurrence is 11%, develops due to venous bleeding ).
Epidural hematoma
Acute epidural hematoma occurs at the site of a skull fracture and rupture of blood vessels. The incoming blood gradually peels off the dura mater. Since these hematomas are limited by the sutures of the skull, they have a smaller area than subdural ones, but are larger in thickness. The typical clinical picture is the presence of a light gap that lasts up to several hours. The patient loses consciousness for a short period, comes to his senses and remains stunned, weak and dizzy , and does not have a pronounced headache . Upon examination, amnesia , asymmetry of the nasolabial folds, differences in tendon reflexes on different sides of the body, nystagmus (uncontrolled eye movements), and meningeal symptoms are . The patient's condition may be assessed as mild or moderate.
Subacute epidural hematoma , unlike acute epidural hematoma, has a long light period (up to 12 days), during which the patient remains conscious. There are also MRI differences:
- Acute has an isointense signal on T1-weighted image.
- Early subacute is hypointense on T2 images.
- Late and chronic have a hyperintense signal on T1 and T2.
Intracerebral hematoma
It is a limited accumulation of blood and blood clots in the brain tissue, which occurs when a blood vessel ruptures. The second name is intraparenchymal hematoma . After injury, several intracerebral hematomas may develop. Most often, their growth is observed in the first two to three hours after injury and hemorrhage. Intraparenchymal hematoma is mostly located in the frontal and temporal lobes, less often in the parietal lobes.
Head trauma is not the only cause of intraparenchymal hematoma. Other conditions also lead to it:
- increased blood pressure ;
- brain tumors with invasion into blood vessels;
- aneurysm rupture ;
- changes in the elasticity of the walls of blood vessels in diabetes or systemic vasculitis ;
- taking anticoagulants;
- blood diseases ( hemophilia or leukemia );
- cerebral amyloid angiopathy.
They differ in location relative to the center of the brain and the cortex: subcortical, central, cortico-subcortical, peri-cerebellar. Traumatic hematomas are localized closer to the surface of the brain, and those associated with vascular pathology are located deep in the brain. In size they are large (more than 50 ml), medium (20-50 ml) and small (up to 20 ml).
Causes
The main cause of hematomas is traumatic brain injury with or without a fracture of the skull. Injuries in the elderly and children are most often associated with falls, and in young people with road traffic accidents, violent attacks, and accidents during recreation or sports. Accidents at work and when handling weapons lead to injuries.
Most often, epidural hematomas develop from small impacts. The source of bleeding in these types of hematomas is damage to the meningeal artery or rupture of the venous sinuses. The leaking blood peels off the dura mater and a hematoma forms. Most epidural formations are localized under the tentorium of the cerebellum and temporal region; they are rare in the posterior cranial fossa, but are life-threatening. The source of subdural hematomas is often veins that are damaged due to injury, bleeding from the sinuses during contusion.
If we consider non-traumatic intracranial hemorrhages, they occur when:
- Carrying out treatment with anticoagulants.
- Coagulopathies.
- Anomalies of cerebral vessels.
- Arterial hypertension.
- Hypovitaminosis C.
- Tumors.
- Meningitis and tuberculous lesions of the central nervous system .
- Convulsions.
Spontaneous subdural hematomas form on the surface of the brain adjacent to the temporal, frontal and parietal regions, but can be found in the posterior cranial fossa and the fissure between the hemispheres.
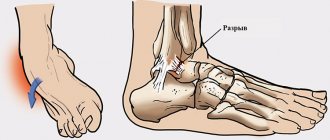
Treatment of bruises of soft tissues of the face
Facial bruising and damage to the soft tissues of the face require special vigilance, since there may be other injuries: fractures, ruptures, etc.
If at the time of the injury there were injuries to the soft tissues of the face, then it is necessary to reject the tension of the skin at the time of applying sutures. Only if necessary, the skin is immobilized to more correctly connect the edges of the wound. Particular care is required when it is necessary to connect the edges of wounds in the area of the lips, nose, eyelids, eyebrows and ears.
If skin defects due to injuries are clearly expressed, then it is impossible to apply sutures without tension, and plastic surgeries are carried out irrationally; in order to reduce the volume of a possible scar, plate sutures are applied.
If we talk about the surgical method of fixing bone elements, then mini-plates, micro-plates, and screws are needed - these are indicated in older people.
A bruise of the face, namely its soft tissues, is treated routinely at the hospital. If the treatment concerns children's health, then conservative treatment is carried out in a hospital setting: sanitation, orthodontic therapy.
Symptoms of a cerebral hematoma
Classic symptoms of hematomas are impaired consciousness , hemiparesis (paresis of the muscles of half the body) and anisocoria (different pupil sizes in both eyes). But the absence of these symptoms cannot indicate the absence of a hematoma. The consequence of intracranial bleeding is an increasing increase in intracranial pressure. The deterioration of the patient's condition is due to its gradual increase. Half of patients with epidural hemorrhage have impaired consciousness to the point of coma, and the remaining patients have a lucid interval. Depressed pupillary response to light and differences in pupil size occur in 45% of patients, and hemiparesis and epileptic seizures occur in 30%. With subdural hemorrhages, impaired consciousness occurs in 60-70% of patients, and in the rest there is a clear gap.
Any hematoma causes compression of the brain, which includes the following symptoms:
- general cerebral - impaired consciousness of varying degrees, headaches , agitation, repeated vomiting;
- focal - hemiparesis , dilation of the pupil of one eye, epileptic seizures ;
- stem - bradycardia , meningeal symptoms , increased systemic pressure, pathological reflexes from the feet.
With epidural hematomas, the classic version of compression with triphasicity in a state of consciousness is more common. At 10-30 minutes after a head injury, the patient loses consciousness, and then it is restored (fully or partially) and this period is called the “lucid interval.” It lasts several minutes to several days. Then a repeated disorder of consciousness occurs (a coma may even occur if the compression of the brain is not eliminated). Also, many patients do not lose consciousness or lose consciousness for a short time. After a light interval, the following appear: first, drowsiness , then stupor , deep depression of consciousness (reflexes persist) and coma . Paresis of the opposite limbs often develops. Bradycardia occurs and blood pressure . In the absence of emergency assistance, the patient dies due to increasing compression of the brain stem. With subdural hematomas and alcohol intoxication, a variant of the course without a clear interval is noted. It happens with severe bruises and crushes of the brain.
Some hematomas clinically manifest weeks or months after injury and hemorrhage. In this way, a chronic intracranial hematoma is formed and most often it is a subdural hematoma.
Symptoms of chronic subdural hematoma:
- Depression of consciousness of varying degrees. In chronic hematomas with gradual accumulation of blood, the disturbance of consciousness is not very pronounced. The volume of the hematoma can reach 200-250 ml.
- Localized, persistent headache is the most common complaint. The pain may progress slowly.
- Meningeal symptoms as in subarachnoid hemorrhage and meningitis .
- Impaired movement in the limbs - from mild to severe paresis.
- Changes in the tone of the facial muscles, sucking or kissing movements of the lips, tremor of the hands , slowing of movements ( bradykinesia ).
- Epileptic seizures.
- Aphasia (speech disorders).
- Sweating , orthostatic hypotension , cold extremities, blood pressure .
- Gait disturbances, instability when performing the Romberg pose.
- Mental changes: disturbance of orientation in place, time, personality, deterioration of attention and sleep. In some cases, patients quickly develop dementia.
Mild brain contusion is manifested by loss of consciousness for up to 1 hour, amnesia , nausea , vomiting , headache at the site of injury, meningism , monoparesis , short-term increase in pressure, and local attacks of epilepsy are possible. Moderate brain contusion manifests itself as impaired consciousness for up to one day. Local attacks with generalization, paresis and oculomotor disturbances are observed. Focal symptoms persist for up to three weeks. A severe brain injury is accompanied by disturbances of consciousness for several days. Convulsive syndrome , pupil dilation , hemiparesis also possible, hypomimia , stiffness of movement, and changes in muscle tone are possible.
After traumatic brain injury, post-concussion syndrome occurs, which is caused by mild diffuse damage to axons. It often develops after a mild TBI and is manifested by various subjective sensations: fatigue , headache , dizziness with nausea , irritability , depression , memory impairment, apathy , anxiety , emotional lability, difficulty falling asleep. Usually, within a few months, brain function is restored and the patient’s condition improves. In some patients, manifestations persist for up to six months after injury.
Tests and diagnostics
In terms of diagnostics, patients are prescribed:
- X-ray of the skull in two projections.
- Echoencephalography.
- Angiography of the brain (to determine vascular disorders).
- CT scan. The main CT sign is displacement of brain structures, which is noted in 100% of cases. The degree of displacement ranges from 5 to 28 mm. On CT, epidural hematomas have a lenticular or lens-shaped shape and are localized in the area of the temporal bone. The subdural hematoma has a crescent shape and crosses the suture lines.
- MRI of the brain accurately determines the location, volume and structure of hematomas, which makes it possible to determine the tactics of surgical treatment.
Where is the best treatment?
Intracerebral hematomas are a very serious problem, associated with high risks of mortality and complete disability. Patients with this diagnosis need to be observed and treated in medical institutions of the highest global level. Some of the best neurosurgical specialists in Europe practice in the Czech Republic.
Central Military Hospital of Prague.
Clinics in the Czech Republic follow only advanced diagnostic principles and cutting-edge technologies for the safe treatment of central nervous system lesions. In addition, the famous republic offers impeccable rehabilitation care for patients after brain surgery.
Czech neurosurgery means the quality of the services provided, as well as their affordable prices. In the Czech Republic, high-tech treatment programs for intracerebral hematomas cost 2-3 times lower than in Israel and Germany.
Diet
Conscious patients do not need a special diet. For unconscious patients, artificial nutrition is provided from the first day to satisfy the need for protein and energy. Tube feeding through a nasojejunal tube is indicated. There are specialized products for tube feeding: Nutrizon , Berlamin , Peptisorb , Peptamen , Berlamin Modular , Nutricomp Standard , Nutricomp Liquid and others.
Consequences of traumatic brain injury and complications
Considering TBI, its consequences and complications, it should be noted that their severity varies from headache to severe neurological symptoms. At different periods of time after a head injury, the following are possible:
- Disorders of consciousness up to coma .
- Meningeal syndrome.
- Post-traumatic arachnoiditis.
- Post-traumatic hydrocephalus .
- Post-traumatic epilepsy .
- Cerebral ischemia.
- Pathological reflexes and paresis .
- Asthenovegetative syndrome.
- Post-traumatic amnesia .
- Post-concussion syndrome , which was mentioned above.
- Akinetic mutism : the patient is awake, but there are no attempts to speak or move.
- Chronic disorders of consciousness - a state of minimal consciousness and a vegetative state.
- Primary post-traumatic dementia manifests itself after recovery from a coma due to severe traumatic brain injury with contusion of the frontal and temporal lobe.
- Persistent neurosis-like syndrome.
- Disorientation and disintegration of speech, behavioral disorders.
- Most patients do not become disabled immediately after receiving an injury, but the consequences of a head injury develop over time - after several months or even years. The long-term period lasts up to 2 years and 70% of victims develop traumatic brain disease and dementia. Post-traumatic dementia can progress over time and resembles Alzheimer's disease . Such complications occur especially often with persistent subdural hematomas.
The operations performed are also accompanied by complications and consequences. The following consequences of removal of a cerebral hematoma can be mentioned:
- Postoperative recurrence of hematomas (especially in chronic subdural hematomas).
- Pneumocephalus (accumulation of air in the skull).
- Secondary hemorrhages into brain tissue.
- The appearance of seizures .
- After surgery, bacterial meningitis (especially after drainage of the ventricles of the brain).
- Pulmonary embolism.
- Thrombophlebitis.
- Septic condition.
- Severe cerebral edema .
Surgical methods for removing VMG
Surgery is indicated in most cases. Its main goal is to save a person’s life and normalize the neurological status. The use of surgery is justified in the following conditions:
- hematomas of any size, accompanied by a pronounced mass effect, cerebral edema, dislocation of the central structures by more than 5 mm;
- lobar and lateral VMGs from 50 cm³ or more in volume;
- medial formations from 20 cm³ and above;
- cerebellar hematomas ≥ 15 cm³;
- progressive deterioration of the patient’s well-being (exception – stage 2-3 coma);
- young age of the patient;
- severe intracranial hypertension when it is impossible to correct ICP conservatively.
The options for surgical treatment are transcranial surgery with direct inspection under microscope control (the standard, most common technique), stereotactic aspiration, and endoscopic removal of the hematoma.
- Transcranial removal. The operation involves direct craniotomy (classical trepanation, often extended) in the projection of the lesion. Next, an encephalotomy is performed in the area of the closest apposition of the VMG to the cerebral cortex. Then they begin to remove the pathological formation, which is carried out by aspiration with washing out the cavity with a stream of saline solution. Heavily condensed elements are removed using special windowed tweezers. Hemostasis is carried out by bipolar coagulation of blood vessels, the use of antihemorrhagic agents (sponges, fibrin-thrombin glue, pads with hydrogen peroxide). A drainage is installed on the wound. The surgical session lasts approximately 3 hours, manipulations are performed under general anesthesia. Direct craniotomy is more common for lobar and cerebellar VMH.
- Stereotactic procedure. Stereotactic aspiration is considered a minimally invasive tactic. However, despite the gentle effect, recurrences of hematomas occur more often after such treatment than after craniotomy. This is explained by the inability to perform thorough hemostasis during stereotactic surgery. The basic type of anesthesia is neuroleptanalgesia. Intervention is performed more often for hematomas of medial and mixed types. The patient's head is pre-fixed in a special stereotactic frame. Next, after placing a small burr hole in the skull, a thin cannula (diameter about 5 mm) is inserted into the hematoma cavity. Through an installed cannula, to which an electric aspirator is connected, pathological contents are evacuated from the brain. Intraoperative control of cannula insertion and therapeutic manipulations is carried out using navigation systems and X-ray equipment. Session duration is 1-3 hours.
- Endoscopic surgery. This is a minimally aggressive neurosurgery tactic that involves removing blood accumulated in the brain tissue under endoscopic control. Anesthesia is usually used by intubation. Access is performed using a surgical device such as trephine, which serves to create a small burr hole in the skull of a round shape. A rigid endoscopic tube is placed into the formed trefination hole. The endoscope tube has a video system that transmits images of brain structures to a color intraoperative screen. The endoscope is carefully brought to the area of interest, then its tidal working system suctions the hematoma and rinses the cavity. Hemostasis is also carried out endoscopically, using monopolar coagulation and defocused laser irradiation. The duration of the procedure is 45-90 minutes.
Russian clinics offer direct craniotomy at a price of 60 thousand rubles or more, stereotactic surgery - 40-60 thousand rubles, endoscopic removal of a hematoma - from 50 thousand to 62 thousand rubles.
After any surgical intervention, a full course of rehabilitation is prescribed, including deep prevention of all possible postoperative complications (infections, thrombosis, pneumonia, etc.). In the majority of cases, after neurosurgery, preventive therapy to prevent epileptic seizures is advisable.
On average, it takes about 6 months for an adult patient to recover after removal of an intracranial hematoma. Depressed functions can be restored completely, but there is no absolute guarantee of this, since everything depends on the initial condition of the patient, age, and the nature and consequences of the intracerebral hematoma at the preoperative stage. In children, rehabilitation usually progresses at a faster pace, and much more often it ends in full recovery.
Forecast
The outcomes of traumatic brain injury can be:
- death;
- lifelong vegetative state;
- severe disability;
- average degree of disability;
- recovery.
The outcome of the injury can be assessed 6 months after the injury. With severe traumatic brain injury, 68% survive and only 8% of patients experience recovery, the rest have neurological disorders of varying severity.
The degree of recovery is influenced by the severity of neurotrauma (duration of loss of consciousness and amnesia) and age. Depending on this, recovery of brain function can be expected from 2 weeks to 9 months. Unfavorable factors for epidural hematomas are: age, anisocoria (or mydriasis), depression of consciousness , hemorrhage volume greater than 30 cm3, intracranial hypertension and displacement of structures greater than 10 mm. When the hemorrhage volume is more than 50 cm3, postoperative mortality increases. The outcome of chronic subdural hematoma also depends on the neurological status before surgery.
The mortality rate for patients who were conscious/stunned before surgery is 5%, and for patients in a state of stupor and coma - 13%. The following treatment outcomes for chronic subdural hematoma are possible: good recovery is achieved in 82% of cases, moderate disability is 14% of cases, severe disability is 2%, and a vegetative state is 1%.
First aid for facial bruises
A facial bruise, regardless of severity, requires emergency assistance. But how to carry it out depends on the seriousness of the situation. So,
- bruise of the soft tissues of the face. A bandage is applied, but not tightly. Ice is also applied to the injury site,
- fluctuation is eliminated with a syringe to avoid blood suppuration in the hematoma,
- profuse bleeding. It is necessary to apply an aseptic bandage to the damaged area. In this situation, the bandage is applied tightly to restrict the flow of blood. If it is necessary to stop the blood from the vessels, then this must be done by pressing the vessel with a finger,
- Asphyxia should be prevented in this way: the victim is placed on his side, face down. Foreign objects are removed from the mouth: blood clots and other contents.
A facial bruise, like any other injury, should not be limited to first aid. Professional medical examination and treatment are required.
[19], [20]
List of sources
- Zhulev N.M., Yakovlev N.A. Mild traumatic brain injury and its consequences. – M., 2004; 127.
- Zotov Yu. V. Complex treatment of severe TBI, taking into account the nature of brain damage and the severity of hypertensive-dislocation syndrome // Bulletin of Surgery, 1996, No. 1, p. 53-56.
- Clinical Guide to Traumatic Brain Injury / Ed. A. N. Konovalov, L. B. Likhterman, A. A. Potapov. T. 1. M.: Antidor, 1998.
- Dzhindzhikhadze R. S., Dreval O. N., Lazarev V. A. Emergency neurosurgical interventions in patients with intracranial tumors // Problems of neurosurgery. – 2011. – Vol. 3. – pp. 62–71.
- Fraerman A.P., Kravets L.Ya., Sheludyakov A.Yu., Trofimov A.O., Balyabin A.V. Compression of the brain in isolated and combined traumatic brain injury. N. Novgorod; 2008; 324 pp.