Achilles tendonitis
Achilles tendonitis is a collective term that includes both tendonitis of the Achilles tendon itself and insertional tendonitis, retrocalcaneal bursitis and Haglund's disease.
Achilles tendonitis is a widespread pathology. The Achilles tendon is the largest and most powerful of all tendons in the human body, it also experiences the most significant stress during walking, running, and jumping and is the most frequently damaged of all tendons.
In simple terms, tendonitis is an inflammatory lesion of the tendon. Inflammation is a major form of the body's natural response to injury, and is characterized by swelling, pain and loss of function.
Tendonitis of the Achilles tendon itself, or non-insertional tendinitis, is characterized by degenerative changes, micro-tears, thickening and swelling of the body of the Achilles tendon. This type of tendinitis is most common in young, active people.
Achilles tendonitis
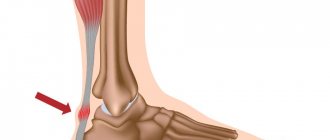
Insertional Achilles tendonitis refers to the same process, but in the area where the Achilles tendon attaches to the heel bone. Insertional tendonitis is also common in older, inactive patients.
Insertional tendonitis of the Achilles tendon
Both in the case of tendonitis of the Achilles tendon itself and with insertional tendonitis, if the process lasts long enough, calcification of the damaged tendon fibers can occur. With insertional tendinitis, this often leads to the formation of bone spurs, sometimes called heel spurs.
Diagram of the location of the Achilles tendon and its attachment to the heel bone
Most often, Achilles tendonitis cannot be attributed to a specific injury. The problem develops over a long period of time as a result of constant overload of the tendon. That is, tendinitis usually forms against the background of excess load, but excess load is determined by a number of provoking factors.
1) A sudden increase in training volume, such as increasing the running distance by a mile every day for a week, which does not provide the opportunity to adapt to the increasing load.
2) Stiff, rigid, insufficiently elastic calf muscles - with a sharp increase in load, they create additional opportunities for damage to the Achilles tendon.
3) The presence of a bone outgrowth – Haglund’s deformity – leads to additional trauma to the Achilles tendon closer to the insertion site.
4) A sudden change in training regimen, for example a sharp transition from long jogging to sprinting or team sports.
The most common symptoms of Achilles tendinitis are: pain and swelling, tightness in the Achilles tendon area that is detectable in the morning, pain in the projection of the tendon and heel bone that increases with exercise, severe pain in the Achilles tendon area the day after training, thickening of the tendon, formation bone spike in the area of attachment of the Achilles tendon, swelling in the tendon area is observed constantly and worsens during the day after exercise. As tendonitis progresses, the risk of spontaneous Achilles tendon rupture also increases. During examination, it is necessary to determine the point of greatest pain; with insertional tendinitis, the pain is determined in the area of attachment of the tendon to the heel bone; with tendinitis of the Achilles tendon itself, it is often located 3-4 cm above the attachment site. Also, upon examination, it is important to determine whether there is limitation in dorsiflexion of the foot.
The most common tests used to diagnose Achilles tendonitis include radiography, sonography, and MRI. X-rays are readily available and can detect such gross changes as calcification of the tendon, the formation of a bone spike in the area of its attachment, and bone damage to the heel bone itself. MRI is indicated if invasive treatment methods are planned, as well as to determine the extent of damage to the tendon itself. Planning surgical tactics is extremely difficult if the level and extent of damage is not determined in advance, which leads to a significant increase in the volume of intervention. Ultrasound research methods in experienced hands are not inferior in sensitivity to MRI; unfortunately, sonography specialists of a sufficiently high level are difficult to find.
Conservative treatment of tendinitis is characterized by a long duration - from the start of treatment to the therapeutic effect, it usually takes 3-6 months. Conservative treatment is also not very effective - about 40-50% of patients are satisfied with the treatment.
Rest is the first and perhaps decisive factor in conservative treatment; reducing the level of physical activity allows you to avoid pain and additional trauma to the tendon. At the same time, you can stay in shape by using an exercise bike, an elliptical trainer, swimming and other sports that do not involve significant stress on the Achilles tendon.
The second important point is the cold. Cryotherapy using ice wrapped in a towel for 20 minutes as needed throughout the day is highly effective in reducing pain and swelling. If you use a rubber or plastic heating pad for freezing, you can give it the shape of a tendon, which increases the efficiency and comfort of its implementation.
Ibuprofen and naproxen can also reduce pain and swelling, but they do not reduce the severity of degenerative changes. With long-term use, the risk of side effects and complications increases.
In the conservative treatment of tendonitis, special importance is attached to exercises aimed at stretching and developing muscle balance in the lower leg muscles.
Stretching the calf muscles and Achilles tendon.
Stand directly in front of the wall, place your arms straight against the wall, place one foot in front and the other behind you, gradually squat without lifting your feet from the floor. Hold the maximum squat position for 10 seconds, then straighten your legs. Repeat 20 times a day.
Stretching the calf muscles and Achilles tendon
Eccentric muscle training refers to exercises that involve tensing a muscle while lengthening it. This type of exercise can cause additional damage to the Achilles tendon if not performed correctly. It is best to perform them under the guidance of a physical therapy instructor.
For double-sided heel drop, you will need a ladder. You need to stand on the edge of two adjacent steps with the toes of your feet. This position allows your heels to move up and down without hitting the steps. Hold the railing with your hands to maintain balance. First stand on your toes, then slowly lower your heels down to the maximum point, stay in this position for 10 seconds, repeat 20 times a day.
Eccentric calf training
A more challenging version of this exercise is to perform it on one leg or with additional weight.
Steroid injections into or around the Achilles tendon are not recommended due to the possibility of dystrophic changes and subsequent rupture.
In the fight against Achilles tendonitis, it is important to choose the right shoes. The most suitable option would be shoes with a soft back or no back at all. A small heel will reduce the tension on the Achilles tendon and reduce the load on it. In an acute situation, when the pain is extremely severe, it is recommended to wear a special orthosis that completely eliminates movement in the ankle joint.
Extracorporeal shock wave therapy has been proven to be effective and free of side effects in a number of studies. There are two treatment options - low-intensity, which requires 3 procedures, and high-intensity, which requires one procedure, but is accompanied by severe pain, which requires the use of anesthesia.
In 30-40% of cases, conservative treatment does not bring relief within 3 months; in such cases, the question of surgical intervention arises. Surgical treatment, according to various authors, is effective in 80-95% of cases. It is necessary at the preoperative stage to determine the presence of concomitant diseases: Haglund's deformity, retrocalcaneal bursitis, insertional tendonitis, as well as the depth and extent of the tendon involved in the pathological process, as this affects the surgical tactics. The access is dictated by the points of greatest pain, so if the pain is located more medially, it is advisable to use the medial approach and vice versa. It is necessary to determine whether the pathological process involves the paratenon, the tendon, or both. For paratendinitis, the surgeon excises all adhesions and also removes scarred areas of the paratenon. After the operation, a 3-5 day period of immobilization follows, followed by the development of movements and physical therapy.
For tendinitis involving less than 50% of the tendon thickness, a percutaneous longitudinal tenotomy can be used using a narrow number 11 or 15 scalpel. After longitudinal puncture of the skin, the blade is directed proximally and the foot is dorsiflexed, then the position of the blade is reversed and plantarflexion is performed. 5-7 similar cuts are used. The technique can significantly reduce the risk of infectious complications; according to the author of the technique, it is effective in 70% of cases.
A minimally invasive method for treating Achilles tendonitis – percutaneous longitudinal tenotomy
The main principle of operations for tendinopathies is the excision of scar adhesions and removal of degenerative tendon tissue. After excision of the thickened, scarred paratenon (tendon sheath), the calf fascia on either side of the Achilles tendon is released. Then several longitudinal sections of the tendon are made, which, on the one hand, makes it possible to detect areas of mucinous degeneration which are then removed, on the other hand, it helps to stimulate the remaining tenocytes to proliferation and synthesis of intercellular substance, and on the third, it promotes angioneogenesis (growth of new vessels). If less than 50% of the Achilles tendon is involved in the pathological process, the degenerative area in the thickness of the tendon is excised in the shape of an ellipse, followed by its longitudinal suturing.
With severe tendinosis (long-term tendinitis), a problem often arises associated with the involvement of more than 50% of the tendon thickness in the pathological process. If 50-80% of the tendon thickness is involved, the tactics are determined by the preferences of the surgeon, the patient and the volume of future sports loads. If more than 80% of the tendon thickness is involved in the degenerative process, plastic surgery is required, for which a tendon transfer, VY plastic, reduction of an inverted flap, or the use of an allograft can be used.
The most commonly used tendon transfer is the flexor hallucis longus tendon. This intervention is contraindicated if the patient plans to engage in rock climbing or ballroom dancing, since these sports require maximum plantar flexion strength of the first toe. A medial approach is used, the tendon is freed from all adhesions, the degenerative areas of the paratenon and tendon are removed, and the deep fascia of the leg is incised, allowing access to the belly of the flexor hallucis longus. The flexor hallucis longus tendon is isolated and cut at the level of the fibrous canal in the area between the medial and lateral tubercles of the posterior surface of the talus. The tendon should be transected as distally as possible. The flexor pollicis longus tendon, depending on its length, is fixed to the heel bone either with an anchor or inserted into a tunnel and fixed with an interference screw.
Release of the Achilles tendon from its paratenon, removal of paratenon scar tissue
Excision of degenerative areas of the Achilles tendon
Dissection of the deep layer of the fascia of the leg, isolation of the tendon of the long flexor of the big toe
Transposition of the flexor hallucis longus tendon to the insertion of the Achilles tendon, preparation of the Achilles tendon for the longitudinal suture after removal of degenerative areas.
Longitudinal suture of the Achilles tendon
Achilles tendon paratenon suture
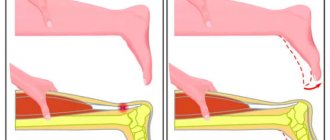
VY plastic surgery (in Russian literature - dovetail) may be necessary when more than 80% of the tendon thickness is involved in the degenerative process over 2-3 cm. With such a significant defect, it is difficult to compare the fresh ends of the tendon. For VY repair, a wider approach will be required, extending proximally to 12-15 cm. After preparing the Achilles tendon for anastomosis, the degree of tendon length deficiency is determined using a reverse springiness test (both legs are bent at an angle of 90° at the knee joint, then the the angle of passive plantar flexion of the feet on the healthy and damaged side, normally it should be 15-20°); when the foot is brought into a normal position, the extent of the defect is assessed. After this, a V-shaped incision (“dovetail”) is made to correct the missing length. After performing the anastomosis, a repeat test for “springiness” is performed for control purposes.
The fresh ends of the Achilles tendon are stitched; when trying to match them, excessive tension is determined, which can lead to overcorrection and subsequent equinus of the foot, suture failure
A V-shaped incision is made proximal to the site of the Achilles tendon rupture, after which it becomes possible to compare and suture the ends of the Achilles tendon at the site of its rupture
After suturing the tendon at the site of its rupture, the missing length is assessed using the “springiness” test, after which the Achilles tendon is sutured at the site of the V-shaped incision and lengthened.
For even larger defects, 3-5 cm or more in length, plastic surgery with an inverted flap or the use of an allograft may be required. If, after releasing the proximal Achilles tendon and gradual traction for 10 minutes, the defect between the ends of the tendon is 5 cm or more, it is advisable to perform plastic surgery with an inverted flap. For this purpose, the incision is extended proximally by 25 cm in order to expose the fascia of the leg over a significant extent. Then, at a distance of 2 cm from the edge of the tendon, a U-shaped flap with a thickness and width of 1\1 cm and the required length is cut out proximally from the fascia (for example, for a defect of 6 cm, it is necessary to use a flap 12 cm long: 6 cm defect + 3x2 cm for the crossed area). In order to reduce the thickness in the area of tendon duplication, it is advisable to turn the tendon inward rather than outward, the distal area of the formed fascial defect is sutured to reinforce the graft origin.
A significant Achilles tendon defect is detected in a normal foot position
Defect length 6 cm
The marker indicates the upper limit of the graft collection site, taking into account the length of the defect and the length of the duplication - 12 cm
Allocation of a site for transplantation
Reduction of the transplanted area
Estimation of the length of the lowered section
The transplanted area is carried out medially to reduce the thickness of the duplication
Surgical treatment of insertional tendonitis involves excision of the retrocalcaneal bursa and protruding sections of the calcaneus, as well as removal of degenerative areas of the tendon. Subsequently, tendon reinsertion may be required using anchors or interference screws. For optimal visualization, a central transachillary approach to the distal portion of the tendon can be used. If the tendon is involved in the process over a significant length, plastic surgery using the above methods may be required.
Medial transachillary approach
With the help of gomens, the tendon is pulled apart
Excessive bone tissue is excised using an oscillating saw.
Excessive bone tissue is excised using an oscillating saw.
The removed bone fragment is shown, an anchor is installed in the calcaneus to strengthen the subsequent longitudinal suture of the Achilles tendon
X-ray showing the size of the resulting bone tissue defect and the location of the anchor in the heel bone
Longitudinal suture of the Achilles tendon using threads from an anchor fixator
In uncomplicated cases when plastic surgery is not required, in the early postoperative period the use of a U-shaped + anterior splint bandage in an equinus position made of plaster or a polymer bandage for 10 days is indicated. After removal of the sutures, walking with full load in a neutral position is allowed in a special rigid orthosis.
Rigid adjustable ankle orthosis
From weeks 6 to 12, passive and active range of motion is developed with isometric exercises. Swimming is allowed from week 3, exercise on the elliptical trainer is allowed from week 4. From week 12 you can start light training. Full recovery will take an average of 3-6 months.
After plastic surgery, a more gentle rehabilitation regime is required. For the first 10 days, the use of a U-shaped + anterior splint bandage in an equinus position (25-45 °) made of plaster or a polymer bandage is indicated. Then wearing an orthosis in the 20° equinus position is indicated for another 6 weeks with a gradual transition to a neutral position with a dosed load, while active dosiflexion of the foot is allowed as far as pain syndrome allows in the position of flexion in the knee joint. Swimming begins at 6 weeks; at 12 weeks, immobilization in the orthosis stops and training on an elliptical trainer is allowed. Full recovery may take 6-9 months.
Surgical treatment of tendonitis is characterized by good early postoperative results in 85-90% of cases, but over time, patients often note the return of the pathology, especially in cases where they continue to actively engage in sports.
Tendon hygroma
Hygroma
- a connective tissue round formation originating from the synovial membrane of a tendon or joint. It is often localized on the hand, and it is in this area that it often causes discomfort.
There is no clear view of the cause of this disease. There is a connection with injuries and physical stress, but in some cases, hygroma appears without any apparent reason. In this case, a slight bulge of the skin forms, as if there is a pea or cherry inside.
The favorite localization of the formation is the area of the wrist joint, although it happens that it appears in other places. Hygroma comes from the membranes of the joint, which, due to weakening of the ligamentous apparatus, protrude between the ligaments and tendons surrounding the joint and form a characteristic subcutaneous formation.
It can exist for a long time without causing any discomfort, but over time pain sometimes appears. Worries especially often appear in people who have to work a lot with their hands. Since the hygroma is associated with the joint, it happens that fluid flows into its cavity. Then for some time it may seem that the formation has disappeared, but, as a rule, after some time it appears again.
NON-SURGICAL TREATMENT
Often conservative treatment methods are ineffective in the vast majority of cases. They try to puncture the hygromas - suck out the liquid with a syringe and inject various substances into it. In this case, the cavity collapses for a while, but the shell itself does not disappear anywhere, and the liquid sooner or later accumulates again.
An absolutely terrible and painful method is crushing the hygroma. In this case, the liquid is forced into the joint cavity, or the membrane of the hygroma ruptures and the contents pour into the tissue. Over time, at best, the hygroma reappears in the same place. At worst, an inflammatory reaction may develop in the area of the injured hygroma, leading to suppuration.
SURGERY
In modern orthopedics, there are 2 methods of surgical treatment of hygroma:
Without an incision and through an incision.
In the first case, the procedure is performed through a puncture. Under ultrasound control, a needle is inserted into the hygroma cavity, a laser light guide is inserted through it, and the cavity is processed with a special laser. Under the influence of heat, the capsule escapes and contracts. And over the next few weeks it resolves.
Excision of hygroma. This is a classic treatment method, but somewhat outdated today, giving the least number of relapses. The key to a successful operation is complete excision of the hygroma capsule with reliable suturing of the latter. The postoperative period can last from 10 to 20 days depending on the extent of the operation.
If you have a hygroma on your arm in the form of a lump, then you need to make an appointment with an orthopedist by phone or through the online appointment system on the website.