Achilles tendon
- one of the main tendons that are responsible for the full movement of a person.
Without it, it is impossible to bend the foot and turn it inward - movements that occur when walking. Given the constant daily stress, the Achilles tendon
is susceptible to injury and inflammation.
They occur especially often (about 6 times more often) in men. Also, people of postmenopausal age are predisposed to diseases and ruptures of the Achilles tendon
.
Is it possible to protect yourself from the problem and what to do if the Achilles tendon hurts
? Read below.
general information
Achilles tendon ruptures most often occur in athletes and active people between the ages of 30 and 55.
This age group is at risk because these patients are still quite active, but over time their tendons tend to become stiffer and gradually weaken. As a rule, this occurs when performing actions that require sudden acceleration or a change in direction of movement (for example, basketball, tennis, etc.). Patients usually describe a sharp pain in the heel area, as if they had been “struck with a stick in the Achilles tendon area.” Acute rupture of the Achilles tendon is diagnosed upon examination of the patient; radiography in this case is of little effectiveness.
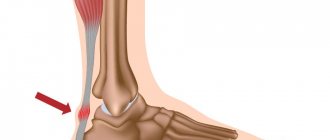
The Achilles tendon is the largest and strongest tendon in the body (Figure 1). It can withstand a load of 2-3 times your body weight during normal walking, so restoring normal function of the Achilles tendon is extremely important.
An Achilles tendon rupture can be successfully treated either non-surgically or surgically. In both cases, this must be treatment in compliance with all rules and regulations. Recent studies show that non-surgical and surgical treatments for Achilles tendon ruptures produce similar results.
Surgery may result in a slightly faster recovery and a lower rate of re-rupture. However, surgery can be associated with very serious complications, such as infection or problems with postoperative wound healing.
Therefore, conservative treatment may be preferable for people suffering from diabetes and vascular diseases, as well as heavy smokers.
Figure 1: Achilles tendon
How to stretch the Achilles tendon for a child with cerebral palsy
The Achilles tendon can be stretched and strengthened at any age, regardless of the cause of its injury. There are entire complexes that allow children with cerebral palsy to develop the Achilles tendon:
- Stand with your feet together , then rise and fall on your toes as many times as possible. It is recommended to stand on a step platform or step so that the heel hangs down a little. An adult must secure the child to avoid falling,
- Take a step back, leaning on your front leg, while keeping your back leg straight and on your toes. The heel of the hind limb should be lowered to the floor, while the knee is straightened. If the child simply performs this exercise, then he can take a wider step,
- Sit with your feet in front and reach your toes with your hands. If the child succeeds, then invite him to lift his leg by the toes, supporting the knee with the other hand,
- Lie on your back, lift your leg bent at the knee, press it to your body. Grab your ankle with both hands and pull your foot towards you until you feel tension in the Achilles and calf muscles.
An expanded complex for a child with cerebral palsy will be prepared by a specialist to reduce the likelihood of complications.
Mechanism of injury and clinical picture
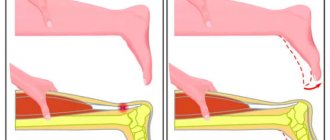
Tears typically occur when an athlete puts stress on the Achilles tendon in preparation for a push-off. This can happen when there is a sudden change in direction, when starting to run or preparing to jump (Figure 2).
Tears occur because the calf muscles create enormous forces through the Achilles tendon as the body moves. At the time of injury, patients feel a sharp pain in the back of the leg or foot, many describe this feeling as if they were hit from behind with a stick, often a clicking sound is heard.
After an injury, an area of retraction or deformation appears along the Achilles tendon, swelling, and hematoma. Patients walk with a limp on the injured limb and cannot stand on their toes. Partial rupture of the Achilles tendon is not common.
Painful tendinitis (inflammation) of the Achilles tendon or a partial tear of the calf (calf) muscles as they attach to the Achilles tendon can also cause pain in this area. The pain of an Achilles tendon rupture may subside quickly, and the injury may be considered a sprain upon initial evaluation in the emergency room.
Rice. 2. Mechanism of injury - a sharp change in the direction of movement to the maximum load of the Achilles tendon
Figure 3: Maximum walking load - heel rise
Preventing Achilles Injuries
The only effective protection against Achilles tendon injury is strong muscles in the lower legs, calves and feet. The stronger they are, the less stress on the tendon. So the first preventative measure is to do exercises to strengthen potentially weak muscles.
Source: runningmagazine.ca
- It is good to strengthen your muscles using the BOSU balance platform. You can do balance exercises on it. For example, just stand on it and keep your balance. Gradually you can move on to platform squats.
- To strengthen your calves, calf raises from the floor or from a platform will be good. If the exercise is done from a platform, then the heels should be suspended, they should be lowered down until tension is felt or pain appears and held for 10-15 seconds. Repeat the movement 15-30 times.
At the next stage, you can complicate the task: perform the exercise on one leg or add a little weight.
- Exercises with a fitness band. Sitting on the floor or on a chair, you need to throw an elastic band over your foot, thus creating resistance, and pull the sock away from you. Hold the stretched foot for 10 seconds, then pull the foot towards you, stretching the calf.
- Stretching is another of the main methods of prevention. She should follow exercises, jogging, or better yet, make stretching a companion to all her workouts: elastic muscles will also protect you from other injuries.
One of the well-known exercises for stretching the calves: standing against a wall, rest your hands on it, lean towards the wall at an angle so as to feel the stretch and tension in your calves. Then bend your knees alternately. The stretching moment can be maintained for a minute.
- Stretch from the platform. This is similar to calf raises, with the only difference being that you need to do the lowering alternately, on each leg separately, and stay at the bottom for about a minute.
- To prevent the appearance or recurrence of inflammation of the Achilles tendon, it is also worth polishing your running technique. Watch the SBU complex with video.
- Watch your diet. The diet should be rich in foods with vitamin D, proteins and collagen, magnesium and calcium.
Foods rich in collagen: chicken and turkey broth, beef, fish, seafood (especially rich in collagen), nuts, cereals like oats, rice, etc., legumes (lentils, peas, beans, etc.), berries, fruits, also dried fruits.
Products rich in magnesium and calcium: milk, cheeses, fish, seaweed. Also, these microelements can be taken together with dietary supplements.
- Increase your training volumes gradually, ensuring the correct balance of load and rest. Follow the rule of a maximum of +10% to volumes every week.
We also advise you to take a closer look at another popular problem among track and field athletes: “Runner’s Knee” - how to diagnose, treat and prevent injury
Clinical examination
An Achilles tendon rupture can be diagnosed quite easily during an examination by a specialist. The most common location of ruptures is 2.0-5.0 cm above the site of attachment of the tendon to the heel bone. The main way to determine the presence or absence of an Achilles tendon rupture is to perform the Thompson test .
The patient is placed on his stomach so that his feet hang freely over the edge of the couch, after which the doctor squeezes the calf muscles. If the integrity of the tendon is not compromised, the foot will rise [plantarflexion]. If there is a tendon rupture, there will be no movement.
Often patients mistakenly believe that their tendon is working normally if they can move their foot up and down. However, this is only possible in a sitting position because the adjacent muscles and tendons are not damaged.
When you try to lift your leg up in a standing position and transfer your body weight to the injured limb, pain and weakness will appear. If an Achilles tendon rupture occurs, it will be incredibly difficult for the patient to stand on their toes for any length of time - this is called the STAMP test . Sensitivity and blood circulation in the foot and ankle are usually not affected.
Diagnosis of Achilles tendinitis
Before making a diagnosis, the specialist examines the patient and studies the complaints received from him.
The following methods are used to confirm tendinitis:
- MRI. The information value of this method is noted in advanced stages of the disease (it is possible to find out whether fluid has accumulated in the affected area) and in the presence of scar changes;
- Radiography. The presence of Achilles tendonitis can be determined by x-ray. It becomes possible to detect pathological manifestations caused by the presence of calcium deposits;
- Testing for the presence of breaks. The ability to flex the joint while lying on the stomach is assessed. In this case, it becomes possible to determine the etiology and localization of the pain syndrome;
- Research in laboratory conditions.
Research methods
In acute tendon rupture, a clinical examination is often sufficient to make a diagnosis. Radiography can be useful only if there is a suspicion of an avulsion fracture of the calcaneus (a situation in which the Achilles tendon is torn from the heel bone with its fragment).
The rupture can be seen on ultrasound or MRI. However, these studies are not needed for acute ruptures unless there is some uncertainty about the diagnosis. These examination methods are very useful for old ruptures or chronic diseases of the Achilles tendon.
Treatment
A ruptured Achilles tendon can be treated either non-surgically or surgically. Both treatment methods have their advantages and disadvantages. Recent studies have shown that non-surgical and surgical treatment of Achilles tendon ruptures provide equivalent results.
The choice of treatment method depends on the individual case and patient. It is important to understand that Achilles tendon ruptures must be treated. Neglected (ignored) rupture of the Achilles tendon leads to negative consequences, such as chronic pain syndrome, lameness, and dysfunction of the injured limb. In addition, old ruptures are much more difficult to treat, and the treatment results are worse, and the rehabilitation period also increases.
The doctor only helps nature restore the integrity of the Achilles tendon; his task is to create comfortable conditions for the regeneration process, namely, to bring the torn ends of the tendon closer together and, for the time necessary for recovery, immobilize them. With a conservative method of treatment, the doctor seeks to bring the ends of the tendon closer together by positioning the foot; with an operative method, the doctor sews the ends of the tendon together with threads.
Non-surgical treatment
With this method of treatment, the foot is brought out and fixed in the equinus position (the foot is in the position of maximum plantar flexion). In this position of the foot, the free ends of the Achilles tendon are brought together as closely as possible. For this, a plaster (polymer) bandage or a rigid articulated section for the ankle joint with the ability to adjust the angle and a heel pad can be used.
With conservative treatment, rehabilitation can be more aggressive - patients are allowed partial weight-bearing on the injured limb from the first day, but full weight-bearing is allowed only 6 weeks after the injury. Modern rehabilitation protocols aim to mobilize patients as early as possible while protecting the injured tendon from significant stress that could cause the healing tendon to rupture or sprain.
It is extremely important that with this approach it is possible to preserve the function of the lower leg muscles. It is necessary to monitor the condition of the tendon throughout the entire period of non-surgical treatment. This can be done through clinical examination and/or ultrasound. If there is evidence of tendon end dehiscence or nonunion, surgical treatment should be considered.
The main advantage of non-surgical treatment is the absence of incisions and punctures in this area, therefore, there can be no problems with wound healing or infection. Wound infection after Achilles tendon surgery can lead to serious complications, so for many patients, especially those with diabetes, vascular disease, and patients who smoke for a long period of time, non-surgical treatment should be considered.
The main disadvantage of non-surgical treatment is that recovery may be a little slower. Full recovery occurs 2-4 weeks later than with surgical treatment. In addition, with conservative treatment, the risk of recurrent tendon ruptures increases. Recurrent ruptures usually occur 8-18 months after the initial injury.
Open Achilles tendon repair
Achilles tendon repair is most often performed through a skin incision made in the projection of the tendon rupture along the back of the leg. The site of the Achilles tendon rupture is reached, then the unfibered ends are sparingly trimmed, cleaned and prepared for stitching. The foot is brought to the position of maximum plantar flexion so that the tension on the tendon is minimal and the torn ends of the tendon are brought together as close as possible, after which suturing occurs. After suturing the ends of the tendon, the wound is thoroughly washed, bleeding is controlled, the skin is sutured, aseptic dressing, elastic compression and immobilization using a plaster splint or a rigid cut. Cold locally. (see Fig. 1).
A possible disadvantage of open Achilles tendon repair is the problem of wound healing, which can lead to a deep infection that is difficult to resolve or a painful post-operative scar.
Figure 1: Open repair of an Achilles tendon rupture
Minimally invasive method for Achilles tendon reconstruction
Another method of Achilles tendon repair is through a “mini” skin incision. In this case, a small horizontal incision 1.5-2.0 cm long is made in the projection of the tendon rupture. The free ends of the tendon are mobilized and brought out into the wound, the dislocated ends are sparingly trimmed, cleaned and prepared for stitching.
Through skin punctures, the ends of the tendon are stitched at a distance of 2.0 - 4.0 cm from the rupture site, the foot is brought to the position of maximum plantar flexion so that the tension on the tendon is minimal, and the torn ends of the tendon are brought together as closely as possible, then stitching occurs.
After suturing the ends of the tendon, the wound is thoroughly washed, bleeding is controlled, the skin is sutured, aseptic dressing, elastic compression and immobilization using a plaster splint or a rigid cut. Cold locally.
Advantages of this technique include less soft tissue damage, less scar tissue, and better cosmesis. Disadvantages include a higher risk of injury to the sural nerve because, unlike open surgery, sutures are placed without exposing the entire length of the tendon, making it difficult to see whether the nerve is in the surgical site.
The nerve that is potentially damaged will cause numbness along the outer surface of the dorsum of the foot, near the little toe. It is possible that the tendon suture itself may not be as strong as with the open technique, which may lead to faster re-rupture. (see Fig. 2)
Figure 2: Minimally invasive method for Achilles tendon repair
The benefits of Achilles tendon surgery include the following:
- faster recovery
- possibility of early range of motion in the lower leg muscles, therefore the rehabilitation program can be more aggressive
- lower percentage of re-rupture (percentage of re-rupture is significantly lower in patients after surgery (2-5%) than in those who underwent conservative treatment (8-12%)
Possible complications of surgical and conservative treatment
- asymmetrical gait (leading to pain in other areas)
- deep vein thrombosis of the lower extremities
- pulmonary embolism
- Achilles tendon nonunion
- repeated ruptures
Complications after surgical treatment
Non-healing of wounds
Although usually a common complication for most surgeries, complications in wound healing are especially problematic in Achilles tendon repairs. Because in the area of the Achilles tendon there is little surrounding soft tissue, and this area of skin has a notoriously poor blood supply. Therefore, any kind of wound healing problem can easily affect the tendon itself. For most patients, there is approximately a 2-5% risk of developing a wound healing problem. However, this risk increases significantly in smokers and patients with diabetes.
Infection
Deep infection after Achilles tendon repair can be a huge problem. Often an infection occurs if there is a problem with wound healing, allowing bacteria from the outside world to infect the repaired Achilles tendon. Treatment may require not only antibiotics, but also the possible removal of all suture materials and, in some cases, removal of the tendon. Smokers and diabetics are at increased risk of serious wound infection after Achilles tendon repair surgery.
Nerve damage/neuritis
Numbness of the skin in the area of the postoperative scar is a fairly common complication. A more serious problem is damage to the nerve that controls muscle function or sensory control. This can happen when a nerve is involved in a suture or damaged by an instrument during surgery. Damage to one of the nerves in the foot often results in neuritis (painful inflammation of the nerve). The initial injury to the nerve may be relatively minor, such as: a nerve that is stretched when soft tissue is retracted during surgery; or a nerve that becomes entangled in scar tissue that forms in response to post-operative bleeding. This type of nerve irritation creates symptoms such as numbness and/or a burning sensation along the nerve. Localized nerve damage is often associated with a surgical incision, and pressing on the area of nerve damage can cause sharp pain or discomfort along the path of the nerve.
First aid for sprains
If you have a foot injury, you should never engage in self-diagnosis or self-medication. Incorrectly selected methods and, as a result, an unfused tendon will not allow you to fully engage in sports and will cause pain and discomfort for a long time. If an injury is detected, you should immediately call a doctor or take the victim to an emergency room.
Before a specialist appears, the leg must be immobilized and a splint applied, trying to do this with the toe extended. If you don’t have the necessary tools at hand, you can use an elastic bandage to secure the limb, and place a thick pad under it to ensure the drainage of fluid.
© charnsitr — stock.adobe.com
To relieve pain use:
- Anti-inflammatory tablets (Nise, Diclofenac, Nurofen and others) and antihistamines (Tavegil, Suprastin, Cetrin and so on). If they are not at hand, you can take any painkillers (Analgin, Paracetamol).
- A bag of crushed ice or a special medical cold pack. The first or second must be wrapped in cloth to prevent hypothermia of the limb. The duration of exposure should not exceed 15 minutes every hour.
- Alcohol treatment of wound edges if the skin is damaged and a sterile bandage to protect it from infections.
Rehabilitation after Achilles tendon rupture
Standard recovery
For the first 6-8 weeks, the leg is immobilized in a cast or brace to allow the tendons and surrounding tissue to heal properly. In addition, the tendon needs to be protected because the healing Achilles tendon may still be too weak to withstand the stress of normal walking. After 6-8 weeks, the patient's foot is placed in a replacement boot, often with a slight heel lift, to take some of the pressure off the Achilles tendon.
From this point on, the patient can begin to walk, but at a slow pace. Physiotherapy and physical therapy aimed at developing movements and strengthening the tone of the lower leg muscles usually begins 6-8 weeks after surgery. The heel lift is gradually removed over several weeks, returning the foot to a neutral position. In the case of standard recovery, the patient can wear regular shoes again 9-14 weeks after surgery.
More aggressive sports rehabilitation after Achilles tendon rupture is indicated for young patients and professional athletes, provided they are disciplined.
Below is an approximate step-by-step rehabilitation plan that will help you recover faster and more effectively after an Achilles tendon rupture.
Ideally, rehabilitation is most effectively carried out in specialized centers under the guidance of professional rehabilitation specialists.
Week 0-2
The shin is fixed at an angle of 20 degrees of plantar flexion (or a heel pad with a 2 cm rise is placed under the heel in the orthosis). Axial load on the leg is prohibited. Walking within the apartment with the help of crutches. In case of surgery, dressings are performed during this period. Prevention of thrombosis.
Week 2-4
The tibia is still in plantar flexion. The exercises begin, several times a day without a splint. The exercises involve gentle rocking movements (up and down) of the ankle joint, trying to keep the Achilles tendon in a neutral position (90 degrees). In addition, inversion and eversion of the foot and lower leg are performed with slight plantar flexion. Axial load on the leg is prohibited. Walking with crutches. Prevention of thrombosis.
Week 4-6
It is allowed to increase the load on the leg. Walking with a measured load on the operated limb. Continue to do the exercises mentioned above and also wear the splint day and night. Prevention of thrombosis.
Week 6-8
Remove the instep under the heel and continue to wear the splint. The exercises progress: slowly stretching the tendon 90 degrees. Resistance exercises are added to strengthen the lower leg muscles. Prevention of thrombosis.
Week 8-12
Gradually wean off the splint and use crutches as needed. Range of motion, stability and proprioception are gradually optimized. Exercises on a balance pad are added.
It is important to understand that in order to return to your previous activity, you must wait for the Achilles tendon to fully heal.
How to avoid Achilles pain?
Injuring the Achilles is especially dangerous for athletes. Inflammation of the Achilles takes a long time to go away and mercilessly throws you out of the training process for at least several weeks, not to mention a rupture.
Here are simple tips on how to avoid Achilles tendon injuries when playing sports:
- If you decide to start running for the first time, start with walking. Walk 3-4 km several times a week until your muscles adapt to the load
- If you are overweight and decide to lose weight by running, also start with walking. Protect your Achilles from unnecessary stress
- Try to get rid of excess weight
- For training, be sure to purchase running shoes with appropriate pronation. They will save your feet from injury.
- Always do a warm-up - the muscles must warm up before loading
- Don’t shock your body with a sudden load: increase your training volume by no more than 10% per week
- Cool down after training to help your body recover faster
- In cold weather, run in long socks that cover your ankles to avoid Achilles colds.
- Eat right: a healthy diet will ensure productivity and muscle recovery
- Strengthen your ankle with special exercises
- Rest from training 1-2 days a week: let your body recover
Preventing Achilles Tendon Injury
Following these simple steps will help you significantly reduce the risk of Achilles tendon injury.
- warm up before starting your workout
- use sports warming ointments before training
- exercise in specialized shoes
- use custom orthopedic insoles
- Balance your level of physical activity with your age and fitness level
- After training, be sure to stretch
- use cold after stretching
- If you experience discomfort during or after physical activity, consult a doctor