Sharp pain in the arch of the foot or the inside of the ankle, including when touched. Visible signs of inflammation where the tendon is located. Stiffness of the ankle joint.
Are any of the above symptoms familiar to you?
If so, you likely have dysfunction (tendinitis) of the tibialis posterior tendon.
How to diagnose, treat and prevent?
You are probably in a state where running is almost impossible. You are in pain all the time, and most likely, after trying to run through the pain in the hope that it will go away, you realize that it is time to start healing.
That's why we've put together a guide to help you get back to running as quickly as possible and prevent the injury from recurring in the future.
- General introduction, extent of injury, etc.
- Signs and symptoms
- Anatomy
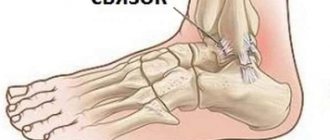
The tibialis posterior tendon is a little known but extremely important anatomical structure on the medial ankle. The tendon itself is not much thicker than a pencil, but it plays an important role in stabilizing your foot.
The lower attachment of the tendon is in the tarsal area, then the tendon passes along the medial malleolus (the large bump on the inside of the ankle) and attaches to the tibialis posterior muscle, which is located deep inside the calf.
The tibialis posterior muscle and its tendon play a critical role in supporting the arch and stabilizing your foot.
Every time you run or walk, the tibialis posterior tendon anchors your ankle, helping to maintain the configuration of your foot as you push off the ground. It also helps you turn your foot so that you can turn your foot inward (for example, so you can place your weight on the outside of your foot).
The hallmark of tibialis posterior tendon dysfunction is pain localized to the inside of the foot and ankle, sometimes extending several centimeters up the calf. There may be some swelling around the tendon, and the area may be tender or painful when you press on it. You may experience pain when you lift the inside of your foot off the ground, but the best diagnostic test is to lift one leg onto your toes.
Stand on your injured foot with your leg fully extended at the knee joint, and use your calf muscles to lift yourself up onto your toes.
Single-leg calf raises are painful or impossible if you have tibialis posterior tendon dysfunction.
This may seem strange - why does raising your toes cause pain in the area of this tendon?
The fact is that this tendon plays the role of a stabilizer of the foot.
Think of the arch of your foot as a suspension bridge and the tibialis posterior tendon as a taut steel cable that supports it. Without a strong, properly functioning tendon, the arch of your foot cannot remain elevated, your ankle joint cannot remain locked, and your calves cannot transmit force through your foot joints.
People with severe cases of tibialis posterior tendon dysfunction can barely lift their heel off the ground.
Diagnostics
The doctor diagnoses the foot based on anamnesis, visual examination, instrumental and laboratory tests.
- The doctor interviews the patient. Finds out when the first signs of pain appeared and the presence of concomitant diseases.
- The examination involves palpation of the limb, during which the nature of the pain is determined. In addition, it is necessary to pay attention to swelling of the ankle, measure the flexion amplitude of the foot and exclude damage to the tendon.
- X-ray. Radiography for this pathology is not very informative. It will help diagnose calcific tendonitis, when salt deposits have formed.
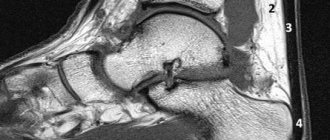
- Ultrasound (see Ultrasound of joints - why do it, what will it show), MRI, CT. These methods allow you to examine sections of tissue layer by layer and determine the presence of tears and changes in the structure of the tendons.
- Laboratory research. A general and biochemical blood test is performed, which can reveal the presence of infection and inflammatory process.
Based on the data of clinical, instrumental and laboratory studies, a final analysis is performed and treatment is prescribed.
MRI revealed ankle tendinitis
What happens if an injury is left untreated?
Although it's not the most well-known injury (it ranks as the 26th most common injury, according to one study), tibialis posterior tendon dysfunction (sometimes also called tendonitis) can be an injury that's extremely difficult to get rid of.
Moreover, if the injury is not treated, it will get worse over time. In some cases, it can become so severe that the arch of your foot becomes compromised, resulting in a deformed foot.
As tibialis posterior tendon dysfunction worsens, the arch height decreases and the foot becomes more inward-turned when you bear your body weight on it because the tendon can no longer provide an adequate degree of support. As a result, the tensile load on the tendon increases. This creates a vicious cycle in which the lower arch and increased pronation of the foot puts more stress on the tendon, which in turn damages it even more, leading to an even lower arch and more inward rotation of the foot, and the cycle repeats.
Causes of injury
Due to the relative rarity of tibialis posterior tendon dysfunction, especially among runners, the causative factors of this injury are poorly understood. Some researchers, such as Melissa Rabbito and her colleagues at the University of Calgary, have suggested that having a naturally high arch protects against tendon dysfunction, but runners with any arch height can develop this injury.
Beyond that, it's unclear what puts you at risk for developing tendon dysfunction. In the general population, the injury is most common among overweight middle-aged women, but this does not provide any insight into the causes of injury among runners. It's not even clear whether gender matters.
For example, a 2002 review that classified injuries of more than 2,000 runners found 8 men with tibialis posterior tendon dysfunction, but only 3 women.
Tibialis Posterior Tendonitis Severity Stages
Doctors break down tibialis posterior tendon dysfunction into 4 stages:
- Stage I is characterized by damage or inflammation of the tendon but no change in the shape of the foot.
- Stage II: The tendon begins to lengthen and the arch of the foot gradually becomes lower. At this stage, you will probably not be able to perform a single leg calf raise.
- Stages III and IV: The tendon may be partially or completely torn, leaving the foot and ankle with permanent deformity.
Treatment methods
The doctor prescribes treatment for ankle tendinitis depending on the cause, type, nature, degree of development of the pathology and the general condition of the patient. Traumatic tendinitis is treated on an outpatient basis. In the first hours after injury, ice is applied to the affected area.
If the disease is caused by other factors, eliminate both the symptoms of inflammation and the causes that provoked it. An important criterion in the treatment of tendonitis is immobilization of the ankle using a special bandage or splint.
Then complex treatment is prescribed:
- drug therapy;
- physiotherapy;
- physiotherapy;
- folk treatment.
If conservative treatment is ineffective, surgical intervention is indicated. Methods such as arthroscopy are used (see Arthroscopy of joints - what is it and why is it used), washing out salts through punctures, redressing (carried out under general anesthesia). You can see how the surgery is performed in the video in this article.
Drug therapy
Drug treatment is prescribed immediately after diagnosis. The doctor prescribes anti-inflammatory drugs that eliminate inflammation, which leads to a decrease in swelling and a decrease in pain intensity. In addition, medications are prescribed to eliminate the pathology against which tendonitis has developed.
Table No. 3. Medicines in the treatment of tendinitis:
| Group of drugs | Expected effect |
| NSAIDs - Diclofenac, Movalis, Celebrex | Prescribed for any type of tendinitis to relieve pain and eliminate inflammation. Can be used intramuscularly and in tablet form. |
| Antibiotics - Tavanik, Flexid | Indicated for traumatic and infectious tendonitis. They have an antimicrobial and anti-inflammatory effect. |
| Corticosteroids - Metipred | Used for severe tendinitis to relieve inflammation and swelling. |
Most drugs can be bought in pharmacies without a prescription. The price of such medicines is quite reasonable. Each medicinal package contains instructions for use of the drug. But in this case, self-medication can only do harm.
Research-Backed Treatment Options
Due to the progressive degenerative nature of tibialis posterior tendon dysfunction, the first step is to ensure that no further damage is caused.
You should see a podiatrist or podiatrist who has experience working with runners to make sure you are still in the first stage of the injury. Because the treatment discussed below may worsen the injury if you are already in the second stage. More severe cases of injury often require orthopedic foot and ankle braces to relieve stress on the tendon, and stage III and IV injuries usually require surgery.
Fortunately, there have been a number of studies that have demonstrated that tibialis posterior tendon dysfunction can be successfully treated with conservative measures. According to these studies, the treatment plan should consist of the following important steps.
Reducing stress on the tendon
If you are trying to run with this injury, stop!
There is no need to increase the risk of developing permanent damage to the arch of the foot. The tibialis posterior tendon heals slowly; probably because the part of the tendon that passes through the medial malleolus has a poor blood supply. Therefore, you should take a break from training and try to minimize other activities that damage the tendon. Cross-training activities such as swimming and cycling are okay as long as they do not cause pain.
We know this isn't what you want to hear, but you risk being out of action for much longer if you continue to train. You can maintain your fitness level during 6 weeks of not running.
Use of orthopedic shoes and insoles
This is also done to reduce stress on the tendon.
All studies performed used custom orthotics and shoes to provide additional arch support, which reduced stress on the tibialis posterior tendon.
In one study, participants were asked to wear custom-made orthotic shoes and insoles for at least 90% of their waking hours for 6 months. In other studies examining running injuries such as plantar fasciitis, standard orthotics such as SuperFeet or PowerStep have been found to be just as beneficial as custom ones.
Orthotics help support the arch of the foot by reducing stress on the tendon.
Calf stretch
In 3 separate studies that successfully treated posterior tibialis tendon dysfunction with conservative methods, calf stretching exercises were also used. The standard protocol consists of 3 sets of 30 seconds of continuous calf stretches against a wall, with either a straight leg or a bent knee, 2 times a day.
You should be stretching both calves, and if you have an inclined footrest, you should use it to stretch the muscles as best as possible. A 2009 study by Cornelia Kulig of the University of Southern California emphasizes that you should wear orthotics or regular shoes with orthotics when performing stretching exercises.
Strengthening exercises
A 2006 article by Richard Alvarez and a team of physicians and physical therapists at the University of Tennessee College of Medicine suggests a comprehensive rehabilitation program for stage I tibialis posterior tendon dysfunction.
The program consists of 2 stages. In the first phase, the exercises are aimed at increasing overall muscular endurance with the help of a movement such as “sole connecting” in a sitting position, and 3 exercises with a rubber band: turning the foot in and out, as well as ankle flexion.
For the last 3 exercises, use a band that provides only light resistance and aim for high reps.
Initially perform the “connection of soles” exercise in 4 sets of 25 repetitions every day, and within 2 weeks reach 12 sets of 25 repetitions. After this, you should aim to reduce the number of sets and increase the number of repetitions until you can do 300 repetitions without taking a break.
Exercises with a rubber band are also performed once a day. Alvarez and his colleagues recommend doing 200 repetitions, starting with the weakest band and taking breaks as needed. Gradually you should be able to complete all 200 repetitions without stopping.
When you can perform 200 repetitions without discomfort, move on to using a stiffer band. Placing a towel under your foot will help you move more smoothly, and holding the band at a 45-degree angle for inward-outward foot rotation exercises will target the right muscles. Do not rotate your leg while performing exercises; all movement should occur at the ankle joint.
Exercises with a rubber band should be performed in orthopedic or regular shoes, but with orthopedic insoles. Make sure all movements are performed slowly.
Kulig's study used a specially designed eccentric strengthening machine for the tibialis posterior tendon, but the exercises in Alvarez's study may be a valid substitute. Although in Kulig's study, only the sole-inward rotation of the foot was performed in 3 sets of 15 repetitions with the greatest tolerable resistance, 2 times a day.
It probably makes sense to do both approaches, doing 3 high-rep weak band exercises once a day for endurance, and a 3 x 15 hard band outswing in a 3 x 15 pattern twice a day for strength.
Tibialis anterior tendon problems
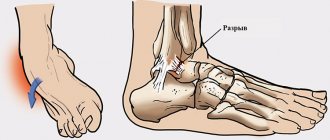
Tibialis anterior tendon ruptures are most often localized within 2-3 cm of its insertion point.
The cause of rupture may be tendon degeneration due to long-standing impingement caused by osteophytes of the talonavicular, scaphocuneiform, and metatarsocuneiform joints, or contact with the extensor retinaculum.
The tendon that is initially damaged most often undergoes ruptures, which is usually associated with a disruption of its blood supply.
Spontaneous rupture of the tibialis anterior tendon (arrows) most often occurs within the distal 3 cm of the tendon.
Ruptures most often occur in men aged 50-80 years, and their number increases with age.
Until the moment of rupture, the patient does not make any complaints.
Shortly before a rupture, patients may notice a small nodule appear in the area of tendon degeneration.
Tibialis anterior tendon tears usually occur as a result of sudden plantar flexion of the foot.
In younger, more physically active patients, an episode of trauma usually occurs, usually not severe, and the rupture is characterized by the appearance of acute pain in the corresponding area.
A patient with a rupture of the tibialis anterior tendon. A, In the plantar flexion position of the feet, no obvious signs of tendon rupture are visible. B, When the foot is dorsiflexed, there is no contour of the tibialis anterior tendon on the anterior surface of the right ankle joint.
A factor that provokes a rupture can be, for example, going down an inclined surface.
At the time of the rupture, the patient notices limited dorsiflexion of the foot, which most often forces him to seek medical help soon after the injury.
In older patients, the rupture occurs without trauma, and they often seek help only weeks or months after the rupture with complaints of foot drop.
Often these patients do not even remember what caused the rupture, and elderly patients do not even know that such a rupture occurred.
Patients often describe a clicking sensation followed by a brief episode of sharp pain in the anterior ankle followed by swelling in the area.
A rupture of the tibialis anterior tendon may be accompanied by the formation of a “tumor” on the anterior surface of the ankle joint.
In the first few hours after injury, patients may experience difficulty walking, but the pain decreases fairly quickly.
Patients may experience poor gait coordination, foot flopping, and an inability to walk without touching the toes. Over time, atrophy of the tibialis anterior muscle develops.
But wait! There is something else!
Stage 2 of Alvarez's program, which begins after 3 weeks of the Stage 1 program, adds single-leg calf raises, toe walking, and rocker exercises to begin using the tibialis posterior tendon in a more functional manner.
Single leg calf raises are performed exactly the same as in the diagnostic test.
Stand on one leg and slowly raise your toes as high as possible, using your hand on the wall for balance. Lower yourself down slowly and under control. Start with a few reps and work your way up to 50 calf raises over time. As with the resistance band exercises, wear orthotics or regular shoes, but with orthotics.
Toe walking is a fairly simple exercise: walk forward on your toes, keeping your heels high off the ground. Start with 8 or 10 meters and gradually increase the distance until you can walk 100 meters.
Finally, Alvarez's program includes exercises to improve balance. Standing on the round swinging platform on your injured leg, swing so that one end of the platform drops to the floor and return back, 20 times in one direction, then in the other, moving clockwise and then counterclockwise.
Perform a total of 2 sets of 20 repetitions for each direction.
When performing any exercise, you should stop if severe pain occurs. Unlike some other tendon injuries, exercising despite the pain is not a good idea in this case!
Alvarez's rehabilitation program lasts 16 weeks (including a 2-week rest period before starting the rehabilitation exercises), and the program in Kulig's study lasted 10-12 weeks, so plan to do the exercises daily for at least 3 months.
Other possible treatment options
Because tibialis posterior tendon dysfunction has not been sufficiently studied, there is little information about additional treatments. Cold application (especially after exercise) is often recommended, both by runners and in the scientific literature. Rolling the calf muscles with a massage roller can also be useful, as relaxing tight calves will reduce the load on the tendons.
If these measures do not help, you should see a physical therapist who can determine if you have any other weaknesses in strength or flexibility that are contributing to your tendon dysfunction.
If your condition does not improve after several months of conservative treatment, you should consult a podiatrist or podiatrist and discuss the possibility of surgery. There are dozens of different surgical techniques that can help repair a damaged or torn tendon, so you should definitely discuss this with a doctor who has extensive experience.
Conservative Treatment Options for Tendonitis
These are methods that are quite simple, inexpensive and can be used at home.
- Wear supportive shoes and orthotics at all times, even when just walking around the house. Talk to your doctor or podiatrist about whether you can use hard, standard insoles or whether you need custom ones.
- Calf stretch, 3 x 30 seconds, with the leg straight and the knee bent, for both legs, 2 times a day. Use an inclined footrest if you have one.
- Exercise “connecting the soles” once a day. Start with 4 sets of 25 reps and work your way up to 12 sets of 25 reps over 2 weeks. After that, start decreasing the number of sets and increasing the number of repetitions until you can do 300 repetitions without taking a break.
- Exercises with a rubber band, 1 time per day (except for the 4th). For the first 3 exercises, switch to using a stiffer band once you can comfortably do all 200 reps without stopping.
1. Flexion at the ankle joint, 200 repetitions. Use a towel to reduce friction under your foot.
2. Turn the foot with the sole inward, 200 repetitions. Use a towel and place the resistance band at a 45 degree angle.
3. Turn the foot with the sole outward, 200 repetitions. Use a towel and place the tape at a 45 degree angle.
4. Turn the foot inward with a band as hard as you can comfortably handle, 3 sets of 15 repetitions, 2 times a day. Progress to using a stiffer tape over time. Use a towel and place the tape at a 45 degree angle.
- Functional exercises performed once a day are added after 3 weeks.
1. Single-leg calf raises, gradually work your way up to 50 repetitions.
2. Walking on your toes, start with 8-10 meters and gradually work your way up to 100 meters.
3. Balance on a swinging round platform: Swing one edge to the floor and return to a balanced position, 20 times, 5 changes of direction. First perform the exercise clockwise, then counterclockwise.
- Applying cold, especially after exercise. Try 10 minutes of massage with a cooled hard object, then a 10 minute break and another 10 minutes of cold. The procedure can be repeated every 2 hours.
Aggressive Treatment Options
These methods are more expensive and less likely to achieve results, but may be useful in some cases.
- Custom orthotics ordered from a podiatrist or podiatrist. Although they can be expensive, they can provide better support for your foot.
- See a physical therapist for a personalized rehabilitation program and to discuss other non-invasive treatments.
- See your podiatrist or podiatrist to discuss the possibility of surgery.
Returning to Running After Tibialis Posterior Tendonitis
Because tibialis posterior tendon dysfunction has a reputation for permanent damage if not properly treated, return to running should be gradual.
No scientific research has offered any advice for returning to running, but you should be very careful to start with very short, easy runs, tapering off if pain occurs. A physical therapist with experience working with runners can help you develop a customized program if needed.
What is pathology: classification of tendinitis
Tendinitis is an acute inflammatory or dystrophic disease. Pathology has a complex classification.
Table No. 1. Classification of ankle tendinitis:
| By mechanism of origin | Tendinitis can be:
|
| By shape | There are acute and chronic tendonitis. |
| Due to development | Autoimmune, traumatic, infectious, parasitic. |
| By the nature of the exudate | Serous, purulent, calcifying. |
Men are susceptible to this disease more often than women.