Ankle sprain is a common sports injury, and 20% of patients with an acute ankle sprain subsequently develop chronic ankle instability. There are 2 million lateral ankle sprains reported annually in the United States, including injuries to the anterior talofibular ligament, calcaneofibular ligament, and/or posterior talofibular ligament. The literature highlights the high level of permanent disability and relapse.
Following an acute ankle sprain, difficulties with postural control, proprioception, muscle reaction time, and muscle strength commonly occur, which can lead to chronic ankle instability (CAI). Inability to jump and land within 2 weeks of a lateral ankle sprain, poor dynamic postural control, and poor performance on a function assessment 6 months after the first episode indicate a high likelihood of developing CNHS. Chronic instability includes mechanical instability (movements exceeding normal physiological limits) and functional instability (subjective feelings of instability associated with sensorimotor or neuromuscular deficits).
Clinical picture
Patients with CNHS have a history of recurrent ankle sprains or more severe inversion injuries. Therefore, they take special precautions when carrying heavy objects, strenuous activities, and walking on uneven surfaces.
CNHS is characterized by a number of disorders that can be assessed by a variety of sensorimotor indicators. It is obvious that in CNGS there is conscious perception of afferent somatosensory information, reflex reactions and deficits in efferent motor control. The specific origin of these disorders, localized to the ankle ligaments or to the spinal or supraspinal levels of motor control, remains to be fully elucidated. It is clear that both inverse and direct mechanisms of motor control are altered in ankle instability.
Read about ankle syndesmosis sprain here.
The main identified causes of CNGS are: a decrease in proprioceptive abilities due to the loss of mechanoreceptors and a decrease in the strength of the muscles that perform inversion and eversion of the foot. When a lateral ankle ligament sprain occurs, the injury affects not only the structural integrity of the ligaments, but also the various mechanoreceptors in the joint capsules, ligaments, and tendons located around the ankle complex. Collectively, these receptors provide feedback regarding joint pressure and tension, ultimately providing a sense of joint movement and position. Through afferent nerve fibers, this information is integrated, along with data from the visual and vestibular systems, into a complex control system that regulates posture and coordination. When afferent input is altered following injury, the corresponding corrective muscle contractions may be altered. Thus, injury to the mechanoreceptors surrounding the ankle joint during lateral extension may contribute to the development of functional impairment and chronic instability.
Proprioception
Proprioception is described as part of the sensory information collected in the central nervous system from mechanoreceptors found in the joint capsule, ligaments, muscles, tendons and skin. Injury to ligamentous tissues containing mechanoreceptors can lead to proprioceptive deficits and, consequently, the development of CNGS.
Muscle weakness
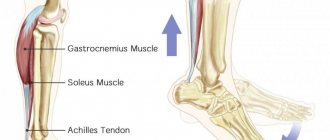
In addition to sensorimotor impairment, researchers suggest that peroneal muscle weakness is also associated with ankle instability. Lack of eversion strength reduces the ability of the associated muscles to resist inversion and return the foot to a neutral position and thus prevent an inversion sprain. In patients suffering from chronic hepatitis C, non-concentric, but eccentric weakness of the muscles responsible for eversion of the foot was revealed. Other investigators have identified deficits in concentric inversion force in patients with chronic hepatitis C. They gave two explanations for the causes of invertor muscle weakness. First, it may result from selective reflex inhibition of the ability of the ankle inverters to initiate movement in the direction of the initial injury. The second reason may be deep dysfunction of the peroneal nerve, which is a consequence of its overstretching. Another theory the researchers have considered is that the pool of motor neurons associated with the invertor muscles became less excitable to lateral ankle extension, while the pool of motor neurons associated with the evertor muscles did not. greatly affected.
Rehabilitation treatment after ankle ligament injuries
It is very important to consider a course of rehabilitation treatment for such injuries in order for the function of the ankle joint to be restored to the maximum extent. Upon discharge from the hospital, the patient receives a detailed plan of rehabilitation measures. Rehabilitation treatment includes a course of physiotherapeutic treatment, shock wave therapy, a set of active and passive exercises aimed at strengthening and stretching the muscles with partial load on the joint, and exercises to develop movements in the joint. In addition, at the Central Clinical Hospital of the Russian Academy of Sciences, on the basis of the rehabilitation treatment department, a biomechanics laboratory has been created, in which patients undergo rehabilitation after various injuries of the musculoskeletal system, incl. professional athletes. On its basis, various walking parameters are studied, and an optimal rehabilitation plan is developed in accordance with the data obtained.
Predictors of CNGS
Doherty believes that a combination of the SEBT balance test and the Foot and Ankle Ability Assessment Test (FAAM) can predict the likelihood of developing CNHS.
- The SEBT balance test (especially the posterolateral direction) has a very significant predictive ability for CNSH.
- The FAAM test (especially the activities of daily living subscale) can be used as an objective assessment of recovery from acute lateral sprain. A low score on the questionnaire, especially in combination with a deficit in movement in the posterolateral direction on the SEBT balance test, indicates a high risk of developing CNHS.
Diagnostics
Mechanical instability of the ankle is associated with ligamentous laxity, while functional instability of the ankle is associated with deficits in postural control, neuromuscular impairment, muscle weakness, and decreased proprioception. The diagnostic criteria for CNHS were recently updated by the International Ankle Association and may include seven subgroups, including a combination of mechanical instability, incidence of dislocation, and sensation of instability.
During the physical examination, hindfoot motion should be noted and peroneal muscle strength checked. The ligaments should be tested for signs of laxity. Stability tests such as the anterior drawer sign test and the talar tilt test should be performed. In patients with CNHS, proprioception is often abnormal; 86% of patients with a grade III ankle sprain have a peroneal nerve injury, and 83% have a tibial nerve injury. To test proprioception, a modified Romberg test can be used: the patient stands on the unaffected leg with the eyes open and then with the eyes closed, and this is repeated with the injured leg.
Listen also to the podcast: Foot and ankle.
An MRI should also be performed to diagnose CNGS. In this case, ligament damage will be indicated by swelling, tearing of fibers, waviness of the ligament, or lack of visualization. The ankle joint should be in a neutral or slight plantar flexion position to help straighten the anterior talofibular ligament and calcaneal fibular ligament. Limitations of MRI include cost, time, availability, motion artifact, and inability to accurately predict the development of CNHS.
Diagnosis of rupture of the ligamentous apparatus of the foot and ankle joint in the clinic
An experienced traumatologist can make a diagnosis after studying the patient’s complaints, studying the medical history and an objective examination. When the anterior ligaments are torn, the foot moves forward freely. If the collateral ligaments are torn, the lateral mobility of the foot increases. The examination is provided by a traumatologist in comparison with a healthy joint.
Our doctors have all the necessary skills and knowledge for quick diagnosis. If necessary, they prescribe instrumental studies.
Treatment
To select the correct treatment, it is essential to distinguish between functional and anatomical instability. Unlike an acute ankle sprain, treatment for CNHS may require surgery. Before undertaking any surgical procedure, it is strongly recommended that all conservative treatment options be used. During the rehabilitation phase, neuromuscular and proprioceptive training should be carried out, as well as orthopedic devices, if necessary.
Friends, the seminar “Lower limbs, diagnosis and therapy, analysis of walking and running” will take place very soon. Find out more...
Because research has demonstrated that repetitive ankle injuries cause neurosensory, proprioceptive, and mechanical impairment, exercises that improve proprioception, balance, and functional ability are indicated in addition to strengthening exercises.
Conservative treatment
Balance training
Problems found in patients with CNHS include impaired postural control and joint position awareness, as well as increased instability. Changes in the functioning of the sensorimotor system are believed to underlie these problems. Balance training is an important part of modern rehabilitation protocols for chronic hepatitis C. The effect of balance training on the sensorimotor deficits characteristic of CNHS was determined. These include postural control, dynamic balance, joint position sense, and segmental spinal reflexes. Performing the SEBT Balance Test has been suggested as an excellent rehabilitation exercise for balance training in CNHS.
Progressive load
Isokinetic muscle strengthening has been shown to have a positive effect on functional capacity, muscle strength, and ankle proprioception.
Orthotics
Docherty recommends the use of orthoses in individuals with chronic hepatitis C for high-risk sports. Individual needs should be taken into account, such as risk of dependence, potential for inappropriate use, cost, etc.
Surgical intervention
When conservative methods do not have the desired effect, surgical intervention should be considered. Damaged ligaments are repaired using tendon grafts or local tissue. Surgical methods include the Broström procedure, which primarily repairs damaged ligaments. Lengthening in primary repair by repositioning the tendon protects the injury and adds stability. Arthroscopy is also effective in the diagnosis and treatment of chronic hepatitis C.
Associated damage
CNGS is often associated with lesions arising from associated factors. They do not necessarily occur with chronic hepatitis C, and if they do occur, they do not occur simultaneously. Associated lesions that may accompany CNS include complex regional pain syndrome, neuropraxia, sinus tarsus syndrome, ligamentous disorders such as peroneal tendinopathy, dislocation or subluxation, impingement syndrome, fractures such as fracture of the anterior process of the calcaneus, fibula bone and lateral process of the talus, articular mouse and osteochondral lesion of the dome of the talus or distal tibia.
Sinus tarsus syndrome
Sinus tarsi syndrome is common among basketball and volleyball players, dancers, and overweight people. It is also common in patients with flat feet and overpronation deformities. This condition includes pain and tenderness in the sinus tarsus, i.e. in the area of the lateral part of the hindfoot. It can result from a single or multiple ankle sprains. The syndrome is diagnosed by exclusion, although MRI may show signs of inflammation. Sinus tarsi syndrome is treated with primary ligamentous repair, tendon augmentation, or both.
Osteochondral defects
Osteochondral defects are damage to the talus bone. These may include swelling of the cartilaginous layers and intraosseous cyst-like lesions or even fractures of the bony layers and cartilage. Osteochondral defects can result from traumatic injury or repetitive trauma. Clinically, there is swelling, instability of the ankle joint and prolonged pain. The exact mechanism is not fully understood. Surgical treatment depends on the nature, size and location of the lesions.
Peroneal tendinopathy
Peroneal tendinopathy is a chronic inflammation of the peroneal tendon that results in weakness of the active stabilizers of the ankle. This occurs when a person performs repetitive activities that irritate the tendon over a long period of time. Additionally, improper training and wearing poor shoes can cause peroneal tendinopathy. People who have hindfoot varus are more likely to develop this condition. In most cases, the disease is treated conservatively, but surgical treatment using an open method or endoscopy is gaining popularity.
Subtalar joint instability
Subtalar joint instability is a disease whose etiology is still unknown. Diagnosis is difficult. It may have symptoms of CNGS. Clinically, patients with subtalar joint instability exhibit increased internal rotation. The condition is treated with tendon transfer or tenodesis, such as the Chrisman–Snook procedure, or alternatively with anatomical ligament reconstruction.
Surgical treatment of ankle ligamentous injuries
If all these measures are ineffective - persistent pain, swelling, a feeling of instability in the joint, repeated injuries, as well as complete damage to the external or internal complex of the ligamentous apparatus of the ankle joint, surgical treatment is indicated - restoration of the ligaments (ligament plastic surgery) to prevent the above complications.
Depending on the degree of damage, one of the surgical methods is used:
- suturing the ligaments (if they are in place, but deformed)
- periosteal valve (if ligaments are torn or not visible)
- transplantation of tendons and ligaments, the use of plantar material, or tendons to replace 2-3 ligaments; when performing these interventions, absorbable (absorbable) materials are used for fixation
The operation is performed under arthroscopic control (using a video camera inserted into the joint, its cavity is examined). Thanks to this, it is possible to diagnose and eliminate problems not only with damaged ligaments, but also inside the joint during one surgical intervention.
Immediately after the operation, the joint is fixed with a plaster cast so as not to subject it to unnecessary stress. This will lead to a speedy recovery. The sutures are removed after 12-14 days. After the sutures are removed, restorative treatment can begin. After 4 weeks, the cast can be replaced with a semi-rigid U-shaped ankle orthosis. Walking without crutches with full weight bearing on the joint is possible after a few weeks.