A hip fracture in the area of its anatomical narrowing is a common injury characteristic of older people suffering from osteoporosis. Such injuries account for 6% of all fractures. Special exercises will help restore limb mobility and return to the usual rhythm of life after a hip fracture.
Objectives of the rehabilitation period
During the recovery stage after a fracture of the femoral neck, it is necessary to solve a number of problems:
- Improve blood and lymph circulation in the damaged area;
- Resume impulse transmission along damaged nerve fibers;
- Accelerate bone healing;
- Prevent muscle atrophy;
- Return supporting function to the leg;
- Prevent the development of complications associated with prolonged bed rest (thrombosis, embolism, bedsores, congestive pneumonia);
- Maintain efficiency and ability to self-service;
- Normalize the patient's emotional state.
With the right approach, physical therapy (PT) can solve all these problems. Gymnastics helps strengthen the muscle frame and prevent congestion in the blood vessels and lungs.
Impact on hip joints with hands
The next component of treatment is applying pressure to the joint with your hands. Its goal is to activate blood circulation in the affected area, restore the elasticity of the adjacent tendons, the elasticity of the joint capsule and provide conditions for joint regeneration.
This requires a chiropractor or someone close to the patient, since self-medication is not allowed here.
Procedure 1
It begins with tapping on the upper posterior edge of the ilium (Fig. 2, a). (A large nerve passes through this place, usually inflamed with coxarthrosis.) It is performed through tightly, forcefully pressed fingers (this technique is called percussion). The stronger the inflammation, the lighter and weaker the blows should be. Then, to cause a rush of blood, several strong slaps are applied with the palm of the hand.
The procedure relieves nerve inflammation and activates regenerative processes in the joint.
Procedure 2
Similar to the previous one, but performed in the area of the head of the hip bone (Fig. 3, a). The blows are applied through the fingers, hard enough, but so as not to cause excessive pain.
During the procedure, salt deposits in the joint capsule, adjacent tendons and in the joint itself are broken down. As a result, joint mobility increases, its nutrition improves and pain decreases. The procedure also ends with vigorous spanking.
Procedure 3
The hand is placed on the front of the thigh, just below the groin, and pressed firmly (Fig. 3, b). Energetic but careful blows are delivered with the wrist or the edge of the palm through the hand.
The main effect is aimed at the rubbing surfaces of the joints. Spanking is not recommended.
Procedure 4
Similar to the previous one, but the hand is placed on the back of the thigh, just below the gluteal fold (Fig. 2, b).
Ends with spankings. All this is repeated, starting from the 1st procedure, 8-10 times.
Indicators of correct procedures are the complete absence of bruises, bruises, pain and slight redness of the skin immediately after the session. A slight increase in pain in the joint is allowed the day after the procedure.
Particular care must be taken when treating coxarthrosis that developed after a femoral neck fracture. Moreover, the older the patient, the more careful it is.
How often should the procedures be done? They are usually held once a week. Then - once a month or once every 2-3 weeks, according to indications. In the most severe cases, accompanied by severe inflammation or swelling - once every 10-14 days. Then, when the disease is alleviated, according to the previous scheme.
Recovery stages
Rehabilitation after a fracture of the anatomical narrowing of the femur is no less long than after a pelvic fracture. It can last from 3 to 12 months. Moreover, it is not always possible to achieve the desired level of recovery.
Helpful information!
The duration of the entire recovery period and each rehabilitation stage depends on the age of the patient, the severity of the fracture, the presence of concomitant diseases, and the method of treatment (surgical or conservative). If at a young age the function of the injured leg is completely restored after 3 months, then weakened older people are forced to remain on bed rest all this time.
First period
At this stage, the patient spends most of the time in a supine (or semi-recumbent) position. In the most acute period (the first few days from the moment of injury) and for 3-5 days after surgery, it is permissible for patients to do only breathing exercises. It normalizes the processes of ventilation of the lungs and saturates the entire body with oxygen. After 5 days (and sometimes earlier), you can begin light - active and passive - gymnastic elements that can be performed in a lying position.
The length of time spent on bed rest is highly variable. But even if this stage is delayed, you cannot increase physical activity on your own. Any expansion of the regimen should only occur with the permission of a physician.
Second period
When the patient is allowed to sit and stand, a new stage of rehabilitation begins.
Note!
At first, all exercises are performed half-sitting, supported by pillows, and sitting, since the body must adapt to an upright position. If you get up too quickly or abruptly, there is a high risk of developing orthostatic collapse - a sharp drop in blood pressure.
When the patient can easily remain in a sitting position for a long time, he can gradually learn to stand up. At first, you should lean only on the uninjured limb.
In the same month, you can start walking: first with the help of crutches and walkers, and later with the support of a cane. A doctor or exercise therapy instructor should definitely help you learn new skills.
Third period
The final rehabilitation stage starts from the moment the patient is transferred to the general regime. The most important thing for this stage is to learn to move without aids, become independent in everyday life and return to work.
This can also take a long time, even in young patients, because too much stress is placed on the femur. To speed up recovery processes, training should be carried out using available means, special exercise equipment, and visiting the pool.
Rehabilitation
Recovery from a hip fracture usually takes three months to one year, depending on how severe the injury is and the patient's condition. Proper rehabilitation is very important - it helps protect the body from thrombosis, infections, and bedsores. A crossbar is attached above the patient’s bed, which will allow him to independently rise and roll over without affecting the injured area. In addition to exercises, breathing exercises are also required, which helps saturate the blood with oxygen and protect against congestion.
Rehabilitation should begin no later than 12 days after surgery. You can't just sit still and wait for the bone to heal. The doctor must develop an individual program for the patient.
After surgery, therapy consists of the following parts:
- Psychological support that will help the patient prevent nervous breakdown due to constant stay in bed.
- A diet aimed at replenishing calcium and vitamins in the body.
- Special exercises for hip fractures.
- A massage that will help maintain muscle tone and blood circulation.
- Physiotherapy.
- To relieve symptoms, the patient may be prescribed painkillers and sedatives.
Features of recovery in elderly patients
In old age and old age, all metabolic and, accordingly, recovery processes slow down. As bone density decreases, fracture healing becomes more difficult. The problem is that surgical treatment is often contraindicated for this category of patients. After all, they suffer from various chronic diseases, osteoporosis, which does not allow the metal plate to be firmly fixed on the femur. And with conservative treatment tactics, rehabilitation is less effective.
Elderly patients have a significantly higher risk of developing life-threatening complications: congestive pneumonia, pulmonary embolism, sepsis due to infected bedsores. This is why they require constant care:
- It is necessary to regularly turn them over in bed, change the position of the head and limbs. This will prevent the development of bedsores and thrombosis;
- You can purchase a special anti-decubitus mattress. However, note that it does not eliminate the need for turns;
- The skin should be regularly washed and treated with antiseptic solutions, especially in areas that have been in a compressed state for a long time - the back of the head, sacrum, shoulder blades, heels;
- To prevent aspiration pneumonia, feed the patient only in a sitting or semi-sitting position supported by pillows. Otherwise, food particles may enter the respiratory tract and cause inflammation;
- At the stage of late rehabilitation, special devices will help facilitate adaptation to everyday life: a frame above the bed that you can grab onto and stand up, special handles and chairs in the bathroom that make self-service easier, something like a railing in the hallway.
Examples of exercises
The tasks below must be completed three times a day. The number of repetitions depends on the patient’s well-being and the characteristics of recovery. On average, the number of approaches ranges from 5 to 10.
Breathing exercises for patients on strict bed rest
The first weeks after a hip fracture, breathing exercises are performed without getting out of bed.
- Press the palm of your right hand to the anterior abdominal wall, place your left hand on the sternum. During inhalation, only the right arm should rise, and when exhaling, lower. This is the process of diaphragmatic breathing.
- Inhale air through your nose and at the same time spread your arms to the right and left, exhale through your mouth, hug yourself with your arms and bring your lower jaw closer to your chest.
- Inhale through your belly, keeping your hands clasped on your abdominal wall. At the exhalation stage, pull in your stomach, stretch your arms forward, turning them with your palms facing forward and without releasing the lock.
- Place your hands on the front surface of the ribs. Exhaling, say a sharp sound “Ha!”, stretch your arms in front of your chest, palms forward, so that a right angle is formed between the back of the hand and the forearm. As you inhale, return to your previous position.
- As you inhale, lift your shoulders up and hold your breath for 4-5 seconds. and exhale.
Exercises while lying on your back
- Squeeze your hands into fists, pull your feet towards you, and at the same time tense the muscles of your arms and legs. Freeze in a clamped state for 4-5 seconds. and relax.
- As you inhale, rise slightly in bed, leaning on your elbows, exhaling, relax and lower yourself back onto the bed.
- Pull your toes toward and away from you alternately.
- Place a cushion under your knees, turn both legs in and out with a small amplitude.
- “Draw” circles with your outstretched toes clockwise and counterclockwise.
Exercises in a sitting position for semi-bed rest
- Lower your legs from the bed so that they do not touch the floor and dangle them a little in a relaxed state.
- Place your feet on the floor. Bring your knees in and out.
- Now connect and spread your legs completely - both knees and shins. The soles slide along the floor.
- In the same starting position, cross your legs. Either the right or the left leg should be brought forward.
- Imitate walking in a sitting position, raising your feet slightly above the floor.
Attention!
If, while performing a set of exercise therapy exercises, a sharp pain appears in the leg, the training should be stopped and the doctor should be informed about this.
Standing workouts
- Place your feet shoulder-width apart and place your palms on your waist. Turn your body left and right.
- From the previous starting position, lean forward, alternately trying to reach the opposite foot with your fingers.
- Stand up straight, extend your arms parallel to your body. As you inhale, move them apart and as you exhale, lower them.
- Simulate walking in place without lifting your toes from the support.
- Now actually start walking in place, but lift your feet off the floor just a little bit.
A set of breathing exercises for the recovery period
- Spread your legs wider, bring your arms forward slightly and gently bend your elbows and wrists so that they form a circle. Inhale through your nose and exhale through your lips in an “O” shape.
- Bend your knees slightly, keep your arms parallel to your body, bending your hands so that your palms face the floor and your fingers forward. As you inhale, extend one arm forward, the other remains down. As you exhale, swap them. Hold your breath and return to the starting position.
- Interlock your fingers, raise them in front of your chest, bringing your hands closer to your sternum and spreading your elbows to the sides. Inhaling, lift one leg up, trying to reach your knee with the same hand. As you exhale, relax. Duplicate with the other leg.
Yoga asanas for the late period of the rehabilitation stage
When performing exercises from eastern practices, not only muscle strength increases, but also balance is restored, which is extremely important for older people. You need to stay in each position for about a minute.
- Ananda Balasana. Lying on your back, pull your knees towards your stomach. Wrap your fingers around the outside of your feet. Spread your knees so that they are slightly wider than your torso. Straighten your legs slightly so that your shins are at right angles to the floor, and pull your feet towards you. The legs should put light pressure on the arms, and the arms should provide resistance.
- Setu Bandhasana. From the previous starting position, place your arms straight above your head. We place our legs closer to the pelvis and across its width. Now let’s lift our pelvis up, resting on the floor only with our shoulder blades and soles of our feet.
- Balasana. Get on your knees, keeping your feet together. Sit on your heels, lower your torso down onto your legs, stretch your arms forward and place them loosely on the floor. Relax.
Massage
After damage to the femoral neck, several massage techniques are effective. During the period of immobilization, massage is possible only for the uninjured leg: knead the area of the thigh, lower leg, and leg joints. If the treatment is carried out using the open method, without the need to wear a splint, then the area of the injured joint and thigh muscles can be massaged from the first days after surgery. However, the massage should be gentle, in the form of stroking.
The duration of the procedure for a healthy limb is a quarter of an hour, for a sick limb – 7 minutes. Starting from the second stage, the massage becomes more active, kneading, rubbing, and vibration are added.
To prevent complications from the lungs, percussion massage of the chest is very important. It involves lightly tapping different areas of the chest. The patient must first take a drainage position: lying on his stomach or leaning forward. This allows you to remove phlegm from the bronchi and improve local blood flow.
Of course, rehabilitation after a hip fracture is a long and complex process; recovery classes are carried out both in the hospital and at home. However, if you follow the basic principles of exercise therapy - gradualism, systematicity and regularity - there is a high chance of completely restoring the function of a broken leg.
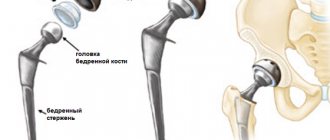
Diagnosis and treatment for hip fracture
The essence of surgical treatment is the introduction of special structures into the fracture - knitting needles, rods or screws, each of which is selected taking into account the nature of the injury. If indicated, partial or complete joint replacement may be performed. This operation is called prosthetics.
Surgical intervention should preferably be performed as early as possible, literally on the first day after injury. However, if there are contraindications, the dates may in some cases be postponed. Sometimes the patient needs to spend some time in traction.