The neck refers to the proximal part of the shoulder, which accounts for about 6% of all cases of skeletal fractures in middle-aged and young patients. Almost 50% of joint injuries in the elderly population are associated with this structure. In 75% of cases, humeral neck fractures occur in people over 60 years of age. According to statistics, women are twice as likely to be injured due to osteoporosis during postmenopause. The proximal part of the bone has a small cortical layer due to age. In the area of the surgical neck there is a transition to the head - the place of attachment of ligaments and muscles.
Types of fractures and symptoms
The main mechanism of injury is a fall on the elbow or resting on the palm of an outstretched hand. The limb may be abducted, adducted, or neutral at the moment of landing. When colliding with a surface, the shoulder turns out, deviates and moves backward. The impact force displaces the head in the direction of the glenoid fossa, and it hits the scapula or acromion process with a bang. Depending on the position of the arm, there are three types of fractures: impacted, abducted, and adducted.
Impacted fracture
For impacted fractures of the humeral neck, the arm remains in a neutral position. Under the action of an external force along the axis of the humeral diaphysis, its lower fragment is embedded in the upper one. Transverse damage is formed. The fragments may not move in the longitudinal direction, but more often they open at a posterior angle.
Adduction fracture
The injury occurs when the humerus is adducted and is therefore called adduction. Adducting injury is usually complicated by displacement of fragments. The central one is retracted and turns outward, and the peripheral one migrates upward, outward or forward and in relation to the first one, turns around. The angle between the fragments opens back and inwards. The adduction fracture is often impacted, where the body of the bone is embedded into the humeral head. Less often, fragments are completely separated and displaced relative to each other.
Abduction fracture
The name suggests the mechanism of injury - the humerus at the moment of landing was in abduction from the body. The formed central fragment is rotated inward and adducted. Peripheral - rotates medially, moves forward and upward. The angle between the fragments opens back and out. The outer edge of the bone may penetrate the head, forming a wedge fracture. Without penetration, the fragments are displaced and separated. Abduction type injuries are the most frequently reported.
Common reasons
In almost 90% of cases, a fracture of the surgical neck of the humerus was provoked by a fall to the ground from a height of one's height. Older people are injured more often. Typical causes of injury in young patients are injuries from road traffic accidents or falls during sports activities.
Intra-articular injuries of the anatomical neck occur rarely, and only in the elderly. More often, the fracture line passes through or under the tubercles on the humerus. The combination of transtubercular and subtubercular fractures is a group of fractures of the surgical neck of the humerus.
It is believed that at the time of injury, the head is dislocated, and the humerus is broken by axillary traction and impact, as well as subsequent contusion on the edge of the socket.
SURGICAL TECHNIQUE
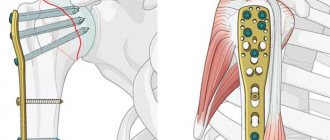
PROXIMAL SHOULDER PLATE
New three-dimensional standard in shoulder osteosynthesis
- Optimal anatomical structure
- Reduced risk of subacromial impingement
- 3D subchondral support
- Lightweight soft tissue attachment
Simplified soft tissue fixation
- The unique design of the holes for the ligatures allows the tuberosity to be restored after fixation of the head of the humerus
- Holes for ligatures allow repeated threading for strong fixation of soft tissues
Guide technology
- Pre-installed disposable drill guides
- There is no need for intraoperative assembly, which significantly saves time
- The conductors are color coded for easy plate identification: red - right lime - left
Diagnostics
It is difficult to recognize a closed fracture if the displacement of the fragments is insignificant. Patients exhibit the following complaints:
- pain that gets worse with movement;
- swelling, bruising;
- displacement of the axis of the shoulder joint;
- lag of the elbow from the body.
The contours of the joint are usually preserved. The traumatologist feels the shoulder, and when pressing on the proximal end of the bone, pain appears. Light blows to the elbow towards the shoulder also cause increased pain. Adduction fractures are easier to detect visually when the fragments are displaced: a protrusion forms on the outside and in front, and a sharp edge appears on the side of the axillary line. Abduction fractures externally resemble a dislocation of the joint along the retraction of the shoulder. Active movements are completely impossible, and when they are performed, a crunching sound is heard. If the fragments are separated, then the rotation of the humerus occurs with a stationary head.
Impacted fractures are more difficult to diagnose because the symptoms are mild: swelling, pain when pressed, tapping on the elbow are the main manifestations. Non-displaced fractures manifest themselves under axial load and rotation, limiting function. When fragments are separated, normal movements are sharply limited, and pathological mobility within the joint is noted.
In surgical neck fractures, the axillary nerve is sometimes damaged by fragments in the armpit. The complication is identified by swelling, venous stagnation, sensory disturbances and drooping of the upper limb.
If damage to the shoulder neck is suspected, an x-ray examination is performed to rule out dislocation, bruise and sprain. Pictures are taken in anteroposterior and axial projections to identify displacements and their angles.
Pelvic bone cancer
Primary tumors of the pelvic bones are rare tumors of bone tissue, while both osteosarcomas (tumors originating from bones) and chondrosarcomas (tumors originating from cartilage tissue) are equally common.
In rare cases, sarcoma of the hip joint occurs. This pathology occurs more often in men than in women.
Symptoms of pelvic bone cancer include:
- Dull pain in the buttock and pelvis, which is sometimes accompanied by a short-term rise in temperature;
- As the disease progresses, pain during walking and physical activity begins to increase;
- Over time, when the tumor reaches a large size, swelling and protrusion are found on the skin, while the skin becomes thinner, due to which a vascular pattern becomes visible;
- In the final stages, when the tumor compresses the vessels and nerves, the pain begins to radiate to the groin, thigh, perineum, and spine;
- When the hip joint is affected, painful contractures and limited mobility occur.
First aid
First aid consists of providing the victim with peace, making him sit up and providing support for the shoulder. In case of bleeding, apply a tourniquet above the site of injury.
Emergency assistance includes:
- injection of a 1% novocaine solution into the hematoma (an allergic reaction is excluded), at the same time a puncture of the joint is performed for hemarthrosis;
- the patient is given sedatives and administered narcotic analgesics for severe pain;
- the shoulder and joint are immobilized using a bolster in the armpit, the arm is fixed with a scarf or Deso bandage;
- the wound surface is covered with an aseptic bandage until the shoulder is fixed, the brachial artery is clamped or a tourniquet is applied.
You cannot displace bone fragments or compress the wound yourself.
Which doctor should I contact?
The victim is hospitalized in the trauma department. The doctor examines the shoulder and performs testing. When the neck of the humerus is fractured, there is no characteristic springy resistance to movement, as with dislocations.
The shoulder is anesthetized, closed reduction is performed, and fixed with a splint or thoracobrachial bandage. Be sure to monitor the position of the bones using x-rays when the plaster dries and after 7 days.
Treatment
Elderly patients with impacted fractures do not undergo reduction. Reposition is indicated for large angular displacement, if health conditions allow.
Reduction is not required in several cases: the fracture is not impacted, there is slight displacement due to an abduction fracture, there are fragments of the humeral head. Nonunion is rarely recorded in young patients if the fragments have been completely corroded and soft tissues have been damaged.
Young people require reduction even with moderate displacement and angulation. This is especially necessary for adduction fractures, the improper fusion of which will disrupt the functionality of the joint.
Impacted fractures without signs of displacement
Impacted fractures can be treated with a bandage if the fragments are not displaced. The arm, bent at the elbow at an angle of 60 degrees, is suspended freely. The shoulder is numbed to relax the muscles and gradually restore the axis of the humerus. Fusion is helped with the help of therapeutic exercises from the second day. From the fifth day, joint movements are allowed in a lighter position - bending forward. Pendulum swings are allowed, the shoulder is adducted and abducted. The amplitude is increased gradually.
To fix the arm, use a cotton gauze scarf, and place a cushion or pillow in the armpit. Massage is used above the fracture site to improve lymphatic and venous drainage, and physiotherapeutic procedures are used to relieve spasm and pain.
Displaced fractures of the surgical neck of the humerus
Reposition of fragments is carried out by two traumatologists. The arm, bent at the shoulder 30–45 degrees, is moved to the side 90 degrees, the elbow is bent 90 degrees. The shoulder is turned outward 90 degrees and the bone is pulled along the articular axis.
To perform traction, place your foot near the patient's armpit. The traumatologist manually sets the fragments at the fracture site. To fix the combined fragments, a thoracobrachial bandage is used. The shoulder remains abducted 90 degrees, the forearm is flexed 90 degrees, and the hand is extended 160 degrees. Reduction tactics for adduction fractures involve primary reduction of angular displacement. The bones are then aligned in a similar manner.
For abduction fractures, splints and percutaneous or skeletal traction of the limb are used. A splint is installed to align the central and peripheral fragments and completely align the articular axis. Without traction, the shoulder abduction function is impaired.
Surgery
Surgical treatment is carried out using an arthroscope, which involves making 2-3 incisions. Indications for surgery are related to the inability to perform reposition:
- large displacement of fragments;
- herniation of the tubular bone into the head;
- rotation of the cartilaginous surface of the head outward and disruption of articular congruence.
Indications for surgery are fracture-dislocations of the humeral head with abduction impacted fractures of the humerus neck with displacement of the greater tubercle, which interferes with muscle function. A fractured head of the humerus is an indication for surgical treatment.
To fix the fragments, external osteosynthesis or percutaneous compression with the Ilizarov apparatus is used. When the greater tubercle is torn off, fixation with a screw or wire is used.
When performing the operation, the incision is made from the acromioclavicular joint along the deltoid-pectoral groove downwards to the pectoralis major muscle. Most often they rely on immersion osteosynthesis with screws, T-shaped and angular plates, and thermomechanical shape memory clamps.
Shoulder arthroplasty
There are indications for replacing the shoulder joint with an endoprosthesis after a fracture:
- anterior and posterior fracture-dislocations;
- head crushing;
- impression fractures;
- fractures of the glenoid cavity of the scapula with fragments.
Depending on the degree of damage to bones and articular surfaces, different types of prostheses are used. Superficial endoprosthetics involves replacing the humeral head. Unipolar prosthetics – the head or glenoid cavity of the scapula.
Total endoprosthetics are performed when both the humerus and the glenoid cavity are affected. Prostheses are anatomical, repeating the shape of bones, and reverse. Reversible types are used when the function of the rotator cuff is impaired. In a reverse endoprosthesis, the concave socket is located on a stem in the humerus.
Fractures of the upper (proximal) part of the humerus
The humerus is the bone that is located between the elbow and the shoulder girdle. Usually the shoulder is the part of the body that is located between the neck and the shoulder joint, but this is incorrect: the shoulder is located lower.
The humerus, like all tubular bones, consists of three parts: upper (proximal), middle (diaphysis) and lower (distal).
The upper (proximal) part of the humerus has a rather complex anatomy and, together with the scapula, forms the shoulder joint. In the proximal part of the humerus, a hemispherical head is distinguished, due to which movements in the shoulder joint are possible. The head is covered with cartilage. Below the head there is a narrowing - the anatomical neck. Under the anatomical neck there are two tubercles - large and small, to which the muscles are attached. The teres minor, infraspinatus, and supraspinatus muscles are attached to the greater tubercle (they rotate the shoulder outward and hold it in the joint). The subscapularis muscle is attached to the lesser tubercle (rotates the shoulder inward). All these muscles form the so-called rotator cuff. Between the tubercles there is a groove in which the tendon of the long head of the biceps brachii passes. Under the tubercles there is another narrowing, which is called the surgical neck. You can read more about the anatomy of the humerus and shoulder joint on our website.
A fracture of the humerus can occur in any of its parts: proximal, middle (shaft) and distal. As a rule, the fracture is localized in one part, but sometimes the fracture line passes through two (for example, the fracture affects the proximal and middle parts of the bone). Each option has its own characteristics, so we will describe them in separate articles.
When does a fracture occur?
Most often, a fracture of the proximal humerus occurs in older people who have osteoporosis, i.e. the bone has little strength. However, a fracture of the proximal humerus can also occur in young people.
A typical injury that causes a fracture is a fall on the arm, but a fracture can also occur from a direct blow to the top of the shoulder. In addition, there are so-called avulsion fractures and fracture-dislocations, which you can read about in a separate article on our website.
Symptoms
Immediately after the fracture, the victim feels pain in the shoulder joint, movements become sharply painful, but more often, shoulder movements are completely impossible. The shoulder may become deformed.
Loss of sensation in the hand, forearm, or shoulder may occur. Numbness or a feeling of pins and needles can be caused both by damage to the nerves during a fracture, and as a result of swelling, which almost always occurs during a fracture.
A few hours after the injury, swelling occurs; later, about a day later, a bruise appears in the area of the shoulder joint (it is mistakenly called a hematoma, but in fact it is just a bruise - the subcutaneous fat is saturated with blood). Over the course of several days or even weeks, this bruise may increase in size and “slide” down, even to the hand.
First aid:
First, make sure the victim is completely safe.
If the patient is unable to walk, call an ambulance. In other cases, you can get to the doctor yourself by taxi - which can be much faster.
Do not try to move your injured arm. This can cause damage to blood vessels, nerves and soft tissue.
If bone fragments protrude from the wound (open fracture), do not try to set them back.
If there is an open fracture, apply a sterile bandage (stop any car that should have sterile bandages in its first aid kit).
Do not apply a tourniquet! Simply bandage the wound tightly and place your hand above the level of the victim's heart.
If it is difficult to apply a bandage, simply cover the wound with sterile wipes or a bandage until the ambulance arrives.
If medical help is not available and the patient must be moved, immobilize (immobilize) the injured limb using temporary splints or a brace.
Temporary splinting can be done using planks, branches, cardboard or rolled up magazines. Avoid applying excessive pressure to your hand.
Suspend your arm from a scarf. A scarf is a piece of fabric with tied ends, worn around the neck and supporting the injured arm.
Headband
What types of fractures are there?
There are several typical types of fractures:
Avulsion of the greater tubercle, fracture of the anatomical neck, fracture of the surgical neck, avulsion of the lesser tubercle, intra-articular fracture (splitting of the head), fracture dislocation.
Each of these typical options can be combined with the other, so that a particular patient may have a combination of, for example, avulsion of the greater tuberosity and a fracture of the surgical neck, or any other option. In addition, the fracture can be impacted - if one fragment is pressed into another. To describe the variety of possible fracture options, traumatologists most often use the Neer classification, which distinguishes one-, two-, three- and four-fragment fractures.
As we have already mentioned, muscles that have different directions are attached to the tubercles. Because of this, bone fragments often shift in the direction where the corresponding muscles pull them.
Typical displacements of tripartite (three-part) fractures. On the left - avulsion of the lesser tubercle and a fracture of the surgical neck, on the right - avulsion of the greater tubercle with a fracture of the surgical neck. The greater tubercle migrates upward and backward.
A large tubercle displaced upward and posteriorly will interfere with abduction, since in this case it will simply collide with the acromial process of the scapula, limiting movement.
A completely severed greater tubercle may move into the subacromial space, and in this case, it will also be impossible to move the arm to the side in the future.
The greater tubercle displaced into the subacromial space (marked with a red arrow)
In general, there are a lot of options for fractures of the proximal part of the humerus; you can read more about them on our website.
Diagnosis
The diagnosis of a fracture of the proximal humerus is made based on the results of examination and additional research methods (x-ray, computed tomography). During the examination, the doctor will ask you about the circumstances of the injury. Try to be as detailed as possible, but at the same time succinctly tell about what happened. Be sure to report the symptoms described above if you have them (numbness, etc.).
The exact nature of the fracture cannot always be determined from radiographs, since there are many types of fractures, and on simple radiographs the fragments are often layered on top of each other. However, an anteroposterior radiograph is always taken first. If the fracture is simple, then this is enough, but if the fracture is complex, then it is necessary to perform either radiography in additional projections (oblique, axial, etc.) or computed tomography. Radiographs in additional projections are technically complex and often require that the hand be given a special position, and this is often impossible due to severe pain. Therefore, surgeons often prefer computed tomography.
In any case, performing a CT scan before conventional radiographs is not always advisable. Magnetic resonance imaging is less informative than computed tomography in diagnosing the nature of the fracture, but sometimes, if the doctor suspects damage to the ligaments or tendons, this study is also performed.
How to treat fractures of the proximal humerus?
There are two main ways to treat fractures - conservative (without surgery) and surgical. The choice of treatment method is made taking into account the nature of the fracture, displacement of bone fragments, the patient’s lifestyle, and concomitant diseases.
All fractures of the proximal humerus can be divided into two types:
- those that can be successfully treated conservatively, i.e. without surgery and
- those that are better to operate on.
Non-surgical treatment is advisable for simple fractures without displacement or with minimal displacement of fragments (less than 1 centimeter). In addition, conservative treatment is indicated in cases where, for various reasons, the patient’s arm did not function before the injury (after a stroke, for example).
The hand is immobilized using special splints made of plaster or modern hardening materials. There are also modern orthoses that are much more comfortable than a conventional plaster splint. The specific type of orthosis or cast that is appropriate is determined by the nature of the fracture. The timing of immobilization is also determined by the nature of the fracture. Usually, with conservative treatment there is more long-term immobilization than with surgical treatment.
In other cases surgical treatment , which allows you to eliminate the displacement, fix the fragments and begin movement in the shoulder joint earlier.
The type of fixation of fragments is determined by the nature of the fracture. When the greater tubercle is torn off, it is often fixed with wire or a screw and wire.
Fixation of the greater tubercle with wire.
For more complex fractures, fixation is performed with an intramedullary pin or plate.
Fixation of the fracture with the PHILOS plate from Synthes.
The requirements for plates for fixation of proximal humerus fractures are very high. They must be made of high-quality alloys, have a large margin of mechanical strength, the screws must be locked in the holes of the plate, and the plate itself must have additional holes for suturing the rotator cuff tendons and ligaments of the shoulder joint. All these features determine their high cost, which in our country can easily exceed 1000 US dollars.
On the left - osteosynthesis with screws, on the right - osteosynthesis with an Arthrex plate with holes for suturing the tendons of the rotator cuff
Osteosynthesis with an intramedullary pin is usually a less traumatic operation, but it has its limitations. As a rule, the choice in favor of an intramedullary pin occurs in simpler fractures without avulsion of the tubercles, or in cases where the fracture line extends to the diaphysis. However, intramedullary osteosynthesis is also possible for more complex fractures, but technically this operation is very difficult.
In elderly patients, one of the main difficulties associated with proximal humerus fractures is osteoporosis. The bone is soft, “sugar”, and ordinary screws in such bone easily cut through and the entire structure becomes unstable.
In addition, in elderly patients, comminuted fractures often do not heal at all, even with ideal reduction (comparison of fragments) and fixation, due to the fact that the blood supply to the head decreases with age. Therefore, if the doctor evaluates the blood supply to the head in an elderly patient as insufficient, then it is not osteosynthesis that is performed, but endoprosthetics - i.e. the joint is replaced with a new artificial one.
Shoulder endoprostheses from Zimmer® (Anatomical Shoulder™, inverse and reverse)
Complications
In addition to the fact that the operation eliminates the displacement of bone fragments, it also has disadvantages. In particular, the main complications of surgical treatment are:
Osteolysis (resorption) of the head. This complication is caused by insufficient blood supply to the head of the humerus, which, being deprived of nutrition, gradually dissolves. Typically, this complication occurs when osteosynthesis is performed instead of the recommended primary arthroplasty. However, this choice is not without meaning, since osteosynthesis is an attempt to “save” the joint. In any case, the risk of osteolysis must be assessed individually for each patient and surgery should be planned based on this assessment. This complication can occur both after surgery and after conservative treatment.
Head perforation with screws. If screws that are too long are used during osteosynthesis, they will perforate the articular surface of the head and interfere with movements in the joint. This is a technical error and can only be avoided by carefully following the rules for performing the operation. In particular, the operating room must be equipped with an electron-optical converter (EOC), which allows the surgeon to take radiographs in several projections and ensure the correct position of the screws.
Impingement syndrome. This is impingement syndrome, where a mechanical obstruction interferes with movement in a joint. Most often, impingement syndrome of the shoulder joint is caused by a collision of a displaced greater tubercle or the upper edge of an incorrectly positioned plate on the acromion process of the scapula.
Frozen shoulder. Sometimes this complication is also called adhesive capsulitis, although these concepts are not entirely synonymous. This complication can occur both after surgery and after conservative treatment. The complication is manifested by a sharp limitation of movements.
Infectious complications – osteomyelitis. To prevent this complication, it is necessary to comply with the requirements of asepsis, and the patient should receive antibiotics for prophylactic purposes (prescribed intravenously 30 minutes before surgery). The incidence of this complication is less than 1%
Rehabilitation
In the postoperative period, the arm is usually immobilized with an abduction orthosis or a plaster cast, and painkillers such as paracetamol or aspirin or ibuprofen may be prescribed.
After normal fusion of the fragments, the function of the shoulder joint is gradually restored, but the significant severity of the injury itself sometimes does not allow the function of the joint to be restored completely.
With stable bracing, exercises to increase range of motion and strengthen muscles can be started as soon as pain subsides. Control examinations by a doctor and control radiographs are required, the frequency of which is determined by the attending physician. During these examinations, the doctor makes recommendations on expanding the rehabilitation program or, conversely, advises stopping the exercises.
You can see sample exercises for rehabilitation on our website (click to go).
What questions should you discuss with your doctor?
- What are my individual risks of complications during surgical and conservative treatment? Which treatment method will allow me to count on maximum success in my case?
- How will this injury affect the function of the hand in the future?
- Can any of my individual factors affect the outcome of treatment (concomitant diseases such as diabetes, etc., bad habits)?
- Which implant for osteosynthesis is optimal for this type of fracture?
- How fully can I take care of myself after the operation?
- When can I return to work if my job involves...?
- When should follow-up examinations and x-ray examinations be carried out?
| The author of the article is Candidate of Medical Sciences Sereda Andrey Petrovich The article is intended exclusively for comprehensive information about the disease and its treatment tactics. Remember that self-medication can harm your health. See your doctor. |
Treatment of humeral neck fractures in the elderly
Elderly people often have absolute contraindications to surgery: atrial fibrillation, malignant hypertension, diabetes mellitus. Elderly patients undergo pain relief and fixation of the shoulder with a bandage. Exercise therapy begins in the early period to restore muscles and joint mobility.
In old age, comminuted fractures heal less well due to poor blood supply. Sometimes endoprosthetics is chosen instead of osteosynthesis if surgery is permissible. Contraindication is osteoporosis. During surgery, minimally invasive techniques and fixatives are used that do not injure soft tissues and bones. Fixation with a plate in old age is used with the expectation that it will remain in the bone for a long time.
Causes of the disease
Today medicine is not yet able to answer this question. The number of patients with primary bone cancer pathology from year to year either remains the same or grows, but does not decrease. The only exceptions are patients with secondary lesions of bone tissue: in this case, the percentage of people with cancer depends on the location of the primary tumor and timely treatment.
But it should be noted that primary bone tumors occur mainly in people 10-20 years of age, and the incidence is higher among patients who smoke.
Recovery time
After surgical repair, the shoulder is fixed with a splint. In any case, from the third day after reposition and fixation of the shoulder, the patient is forced to move his fingers, bend and straighten the wrist and elbow joints. Surgical sutures are usually removed after a week. Movements in the shoulder are allowed from the 20th day . Metal elements during osteosynthesis are removed after three months.
With a conservative approach, immobilization lasts from 6 to 8 weeks, but after a month the plaster is removed and the arm is fixed on an abduction splint. The average rehabilitation period is 3–4 weeks, and full working capacity is restored after six months. The patient is forced to raise his arm on the splint to avoid pain.
In older people, recovery times are much longer and are usually associated with poor blood supply. Therefore, in old age, daily exercise and physiotherapeutic methods of regeneration are necessary.
Rehabilitation period
After undergoing conservative or surgical treatment, rehabilitation follows, during which the patient restores physical activity. Breathing exercises, finger exercises, and joint development (shoulder and elbow) are required. In addition, the patient is assigned to undergo:
- magnetic therapy;
- electrophoresis;
- phonophoresis;
- salt bath;
- mud therapy;
- hydrotherapy;
- massage.
During the recovery period, the patient needs to eat well and eat foods that contain sufficient amounts of calcium and vitamin D3. For a speedy recovery, the load on the arm should be applied gradually, and if painful sensations occur, stop the exercises and try again later.
Possible complications
Complications usually involve damage to the muscles and axillary nerve, which impairs the function of the shoulder. Complications after operations occur much less frequently: resorption of the humeral head in older people due to poor blood supply, perforation of the humeral head with screws. If the plates are installed incorrectly, impingement syndrome develops - a collision of the greater tubercle displaced by a fracture and the acromion process. Frozen shoulder syndrome becomes a complication even after a conservative approach as a result of insufficient rehabilitation.
Care and rehabilitation
Rehabilitation involves improving blood supply and outflow of venous blood from the fracture area, muscle restoration.
Patients are instructed to move their fingers and hand from the first day. After 3–4 weeks, the thoracobrachial bandage is replaced with a splint, passive movements in the elbow become permissible, then active ones.
Exercise therapy is carried out under the guidance of a methodologist. The set of exercises includes ideomotor loads (mental direction of impulse), isometric muscle tension, moving the palm on the table surface using a cart or light movements on a hammock.
Loads are given for 20 minutes, but up to 5-6 times a day. When the patient can raise his arm above the splint and hold the position for up to 20 seconds, immobilization is stopped and active rehabilitation of the muscles of the shoulder girdle begins. It takes 8–10 weeks to restore working capacity.
Thoracobrachial bandage
Patients are concerned about the question of how to sleep with a cast. The Deso bandage allows you to sleep on your back or healthy side without displacing bone fragments. In case of injury to the right hand - on the left side. Immobilization continues as long as required until the formation of a primary callus. With a thoracobrachial cast, a pillow is placed under the elbow of the broken limb while lying on the healthy side to avoid sagging and pain. If pain occurs during sleep, do pendulum movements while standing.
Exercise therapy in the second period of treatment for a shoulder fracture
The second, functional stage of recovery lasts 3-6 weeks. By this time, a callus has formed at the site of the fracture, which traumatologists at the Yusupov Hospital confirm using x-rays. The goal of rehabilitation at the second stage is to restore the previous range of passive and active movements. The set of exercises is expanded, but the starting position remains the same. The patient is offered the following set of exercises:
- stretch your upper limbs forward in front of you so that they are parallel to the floor;
- move your arms to the sides from the starting position;
- raise your shoulders to a horizontal level;
- move your bent arms to a horizontal level, supporting them with your healthy hand;
- clasp your fingers and swing your hands up and down;
- spread your arms to the sides to a horizontal level.
The patient can move both arms to the sides, bent at the elbow joints, move the elbows in a circle, and move the elbows back. From a standing position with your arm thrown over your back, you can perform pendulum-like swings back and forth. Sliding along the body, you should raise your bent arms. You need to rotate your upper limbs around the longitudinal line.
At this time, water procedures are especially useful. Rehabilitation specialists recommend that the patient, while visiting the pool, perform various movements of the limbs, exercises simulating breaststroke and freestyle swimming, crossing the arms in front of the chest and pulling back. Staying in water puts additional stress on the muscles, while at the same time making the process of doing exercises painless. Water gymnastics improves blood circulation and increases the effectiveness of training.