A femoral neck fracture is not the only injury to the proximal femur. Intertrochanteric and pertrochanteric fractures occur.
These injuries are no less dangerous and, in the absence of proper treatment and comprehensive rehabilitation, can lead to disability or death.
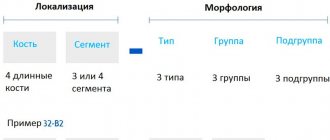
Rice. 1 Schematic representation of different types of proximal femur fractures.
Our clinic has accumulated extensive experience in managing such severe patients. Thanks to the professionalism of our doctors and the use of modern equipment in our clinic, the specialist always achieves a positive result.
Our patients quickly return to their usual active lifestyle.
What are pertrochanteric and intertrochanteric fractures?
There are two anatomical structures located on the proximal femur: the lesser and greater trochanter. They are located below the femoral neck and are presented in the form of protrusions to which the muscles are attached.
In a pertrochanteric fracture, the fracture line passes through these structures, and in an intertrochanteric fracture, the fracture line passes between them.
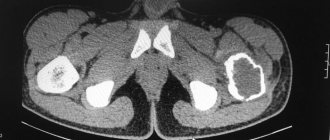
Rice. 2 X-rays of the hip joint. A. intertrochanteric fracture of the femur; b. pertrochanteric fracture of the femur.
Intertrochanteric and pertrochanteric femur fractures can be stable or unstable. In the first case, reposition does not cause difficulties, since the cortical layer of the bone is slightly damaged. In the second situation, treatment is long and complex.
There are seven main types of fractures:
Two types of intertrochanteric:
- Hammered. The joint capsule is not damaged. There is no offset or it is not critical.
- With offset.
Five types of pertrochanteric:
- Hammered. There is no or minimal displacement.
- Impacted with significant displacement. This also includes crushed injuries of the greater trochanter.
- Not impacted with violation of the neck-diaphyseal angle.
- Not driven in without critical displacement. Such damage is often helical.
- Pertrochanteric-diaphyseal with significant displacement. It has a helical line and is accompanied by the presence of fragments.
Rice. 3
Publications in the media
Hip fractures account for 6.4% of all fractures. Classification • Fracture of the proximal femur • Isolated fracture of the greater trochanter • Fracture of the diaphysis of the femur (upper, middle, lower third) • Fractures of the distal femur. Fractures of the proximal femur • Medial (cervical) fracture can be valgus and varus •• Capital fracture (head fracture) •• Subcapital fracture (at the base of the head) •• Transcervical (transcervical) or basal fracture • Lateral (trochanteric) fracture •• Intertrochanteric fracture •• Pertrochanteric fracture •• Isolated fracture of the lesser trochanter Frequency - 25% of the total number of femur fractures. Fractures of the femoral neck and trochanteric fractures are observed mainly in women over 60 years of age • Causes: indirect injury - fall on the greater trochanter • Clinical picture •• Pain in the groin area, aggravated by leg movements •• External rotation of the limb, impossibility of internal rotation •• Shortening limbs •• Pain with axial load (tapping on the heel or in the area of the greater trochanter) •• Symptom of “stuck heel” - the patient cannot lift or hold a raised and straightened leg, but bends it at the knee and hip joints so that the heel slides along the support •• The diagnosis is confirmed by x-ray examination in two projections. A violation of the integrity of the bone is revealed, as well as additional signs: in varus fractures, the greater trochanter is located above the Roser-Nelaton line; in displaced fractures, the Schumacher line, connecting the apex of the greater trochanter with the anterior superior iliac spine, passes below the umbilicus • Complications: false joint of the femoral neck , avascular necrosis of the femoral head
Treatment of femoral neck fractures is predominantly surgical - osteosynthesis with a metal pin, threaded rods, endoprosthetics. In the treatment of intertrochanteric and pertrochanteric fractures, skeletal traction, plaster cast and osteosynthesis are used. Prevention of pulmonary complications, bedsores.
Fractures of the femoral shaft • Causes: direct trauma • Pathomorphology. When the upper third of the diaphysis is fractured, the proximal fragment moves forward and outward, the distal fragment moves inward and posteriorly; a fracture in the middle third is characterized by a displacement along the length • Clinical picture : pain, dysfunction, shortening of the limb, deformity, outward rotation of the foot, pathological mobility • Complications : traumatic shock, fat embolism, significant blood loss • Treatment •• Immobilization is used for birth injuries in children; traction according to Shede •• Skeletal traction for the tibial tuberosity or femoral condyle •• External or internal osteosynthesis •• Surgical treatment is used for open, complicated fractures, with unsuccessful conservative treatment (soft tissue interposition).
Fractures of the distal femur • Causes: direct trauma on the lateral surface of the knee joint, fall onto the knee joint, fall from a height onto straight legs • Pathomorphology. Condylar fractures are intra-articular injuries accompanied by hemarthrosis. In case of supracondylar fractures, the short distal fragment is displaced posteriorly due to the traction of the gastrocnemius muscle, which creates a threat of compression or damage to the popliteal artery • Clinical picture : swelling, deformation, pain, pathological mobility of the fragments. X-ray confirms the diagnosis • Treatment: •• For hemarthrosis - puncture of the knee joint •• Non-displaced fractures - plaster cast •• For displaced fragments - immediate reposition with skeletal traction, if indicated - osteosynthesis •• Surgical treatment if conservative methods are ineffective •• Early prescription of physiotherapy (UHF, magnetic therapy), exercise therapy.
ICD-10 • T93.1 Consequence of hip fracture • S72 Fracture of the femur.
Causes
Such injuries are rare in young people. Damage to the distal femur can occur in the event of an accident, a fall from a height, or in other cases where the force of impact is high.
In old age, even a minor blow or fall can cause injury. An elderly person can receive such an injury without leaving home.
This is due to decreased bone density due to osteoporosis. More often, pathology is registered in women, so they are more susceptible to injury.
Indications and contraindications
The main indications for the use of this method of treatment are unstable fractures of the femur, tibia and humerus in cases where a standard plaster cast cannot provide ideal fixation of bone fragments after immediate reduction. For stable fractures, this method is used when rapidly increasing local tissue swelling is observed.
Contraindications to the use of this method include the presence of inflammatory processes at the site of the wire and the fracture area, damage to large areas of soft tissue, as well as inappropriate behavior of the patient during intoxication and mental disorders. Also, the use of this method is impossible without a mobile X-ray machine.
Symptoms
The symptoms are not much different from a violation of the integrity of the femoral neck. With pertrochanteric fractures, pain and swelling are more intense. A hematoma forms, which can spread throughout the thigh. Support on the limb is impossible; light tapping in the area of injury causes sharp pain.
This indicates that the patient has not just a bruise, but a serious injury that requires emergency medical attention.
A characteristic sign is the shortening of the leg and its forced position, in which the foot is turned outward.
Advantages and disadvantages of this treatment method
Like any other treatment method, skeletal traction has its advantages and disadvantages. The disadvantages of skeletal traction include restrictions on use for the elderly and children, as well as the significant duration of this method of treatment, which can be up to two months. Another serious disadvantage of this method is the possibility of purulent infection during needle insertion. However, this is a rather complicated procedure and any violations can become a serious problem.
But this method has many more advantages, which ensures its widespread use. Thus, this method is minimally invasive, it avoids secondary displacement of fragments, and the rehabilitation time is much shorter. At the same time, the doctor has the opportunity to conduct constant visual monitoring of the injured limb.
Treatment
Depending on the nature of the injury and the patient’s health status, treatment can be conservative or surgical.
In older adults, comorbidities and ability to ambulate before injury should be considered.
Conservative treatment
If reposition is possible without surgery, then conservative tactics are used. If there is no pronounced displacement and numerous fragments, then this method gives good results.
The thigh muscles, even of an untrained person, have great strength, therefore, when they contract, they displace bone fragments. To prevent this from happening, the skeletal traction technique is used. Currently, this method is rarely used.
During traction, control photographs are taken, which allow us to judge the position of the fragments. The process lasts 1.5-2 months, after which the patient can begin to walk on crutches.
Various orthopedic devices are also used to help keep the leg in the correct position and prevent further displacement of bone fragments.
Surgical treatment
In difficult cases and in the absence of contraindications to surgery, the surgical method is used. Fixation of fragments is carried out using metal structures. Within a few days after the injury, the patient can walk on crutches.
The fixation method is chosen individually in each case. There are the following types of osteosynthesis:
- outer;
- submersible; bone;
- intraosseous;
With external osteosynthesis, fragments are fixed through the skin using special nails and knitting needles.
With the submersible method, surgical access is required. When using periosteal surgery, special metal plates are placed on the surface of the fragments and secured with screws.
With intramedullary (intraosseous) osteosynthesis, titanium rods are inserted into the bone canal and locked with screws.
Fig.4. A. intertrochanteric femoral fracture; b. intramedullary osteosynthesis of a femoral fracture with a pin.
Fig.5. A. transsubtrochanteric comminuted fracture of the proximal femur; b. intramedullary osteosynthesis of a femoral fracture with a locking pin.
Leg traction for a hip fracture and other non-surgical methods
The non-surgical treatment plan is approximately as follows:
- Skeletal leg traction for a femoral neck fracture is used for 2-3 months, and weights are also applied. If the fracture is lateral and not displaced, the patient lies in traction for about 10 days.
- After the traction is removed, the patient is allowed to stand on crutches and learn to walk, but should not lean on the sore leg for some time. If an experienced caregiver is nearby, this process is much easier and more effective.
- Exercise therapy after a hip fracture is prescribed literally from the first days of placing the patient on traction. This lesson is usually carried out by a hospital nurse, but a visiting nurse invited to provide care will do the gymnastics more carefully and carefully, since there is only one patient in her care.
Special exercises for a hip fracture without surgery are prescribed; the complex depends on the type of injury, and it must be performed slowly and carefully. The patient himself is still capable of little and is weakened, so during this period the support of a qualified nurse is especially important.
Diaphyseal fractures (damage to the shaft of the femur)
This type of fracture is the most severe injury of all types of injuries to the femur. In addition to the main reasons, it can be noted that athletes often receive it during intense training or competition. Symptoms of a diaphyseal fracture:
- severe pain, swelling and hematoma at the site of injury;
- deformation and shortening of the limb;
- pathological bone mobility.
To prevent the development of traumatic shock and blood loss, emergency assistance must be provided quickly. It consists of securely fixing the injured limb with a splint and administering painkillers.
Flaws
Skeletal traction during a hip fracture is associated with a number of uncomfortable sensations. During the first days, patients complain of severe aching pain in the muscle tissue.
The method has several other disadvantages:
- The procedure carries a risk of infection and subsequent formation of purulent exudate. It is worth noting that in medical institutions only a sterile set of instruments is used. In addition, the installation of the spokes and the hanging of the load is carried out exclusively in compliance with all sanitary standards. Every day the doctor examines the area in which the metal instrument is located. Treatment with antiseptic agents is also carried out regularly. In this regard, the risk of infection is rather a disadvantage not of the method itself, but of the medical institution in which such complications are recorded.
- Prolonged bed rest. The patient needs to remain in the supine position for quite a long time. This is associated with the risk of bedsores and muscle tissue contractures. It is necessary to remain in a lying position until the fusion of bone fragments occurs. Only after the formation of a callus is the needle removed.
- Presence of contraindications. In case of a hip fracture, skeletal traction cannot be prescribed to small children and the elderly.
Despite a number of disadvantages, the method is actively used at present.
Possible complications
Complications can arise for various reasons, which may result in:
- Blood clot formation. This outcome can occur as a result of long-term immobility of the limb. In accordance with this, the patient needs to use drugs aimed at thinning the blood.
- The development of pneumonia due to the use of a large number of drugs and the immobility of the body.
To avoid this outcome, it is necessary to include breathing exercises, which will provide improved blood circulation in the bronchi and lungs. Which in turn contributes to oxygen saturation of the blood and all organs in general. Bedsores and atrophy of the limbs occur during a long stay in a supine position. - To avoid such a complication, you need to include some types of massage that will increase local blood circulation. Physiotherapy will also be beneficial, as it will promote tissue regeneration.
- Digestive problems due to taking medications and prolonged horizontal position. To do this, the patient is offered dietary nutrition that will help not only restore the disturbed intestinal microflora, but also ease the load on the gastrointestinal tract, which begins to work slowly when lying down. In addition, a diet rich in foods rich in vitamins can support the immune system, which also suffers due to the onset of the disease.
Advantages
This treatment method has been used in practice for many years. Every year his technique is improved, which allows him to minimize pain both during the process of hanging the load and after the procedure.
The undeniable advantages of skeletal traction for hip fractures in children over 5 years of age and in adults:
- The patient is under the supervision of doctors and medical staff almost around the clock. The victim can call for help at any time, for example, if severe pain occurs.
- The method completely eliminates re-displacement of damaged bone areas. Contrary to popular belief, the design is extremely reliable.
- Skeletal traction is a minimally invasive treatment method. Due to this, the risk of complications is much lower than after surgery.
- Using this method, it becomes possible to significantly reduce the healing time of bone structures.
Separately, it is worth noting that after traction, the duration of the recovery period is minimal. Soon after the weight is removed and the pin is removed, the patient can begin to perform his daily activities.
The essence of the method
In case of a hip fracture, traction (in the photo below is a schematic representation of the structure) is necessary. This method ensures high-quality and complete fixation of a broken bone.
Initially, the doctor determines the area of the damaged area. A Kirschner wire is then passed through it. This is a medical product made of metal. Immediately before performing this manipulation, the limb is anesthetized. Then a weight is suspended from one end of the broken bone, the weight of which is calculated individually. The bone structures are then compared. As a result, all conditions are created for the successful formation of callus.
Timing of traction
The length of hospital stay directly depends on the severity of the injury and the presence of various types of complications. For a hip fracture, the traction period is about 2 months.
Bone condition is monitored regularly. The doctor assesses the dynamics using x-ray examination. After the formation of a callus, the pin is removed. First, it is shortened on both sides so that its ends are as close to the skin as possible. The limb is then treated with an antiseptic solution. The next step is to remove the spoke. The resulting wounds are treated with medications, then a sterile bandage is applied to them.
After this, the patient is transferred to the fixation method of treatment.
Surgery for an ankle fracture
Ankle fractures are one of the most common reasons for visiting orthopedic traumatologists.
Conservative treatment using plaster immobilization is possible in situations of isolated fractures of the outer or inner ankles without displacement of bone fragments and damage to ligamentous structures. Even in cases of such isolated injuries, the period of immobilization cannot be less than 6 weeks, which ultimately significantly complicates rehabilitation and can lead to longer periods of disability in comparison with surgical treatment. The advantages of conservative treatment of ankle fractures are the absence of risks associated with surgery and anesthesia, as well as the absence of the need to remove metal fixators in the future.
So, the vast majority of ankle fractures require surgical intervention, in the absence of contraindications. Various classifications exist to assist in surgical planning and understanding the relationships between the various anatomical structures in the ankle and foot that may be affected by ankle fractures. The most widespread in international practice, detailed and assessing all aspects of both the injury itself and possible ways of treating it, is the AO classification. You can find it on the website of the International Association of Osteosynthesis.
Unfortunately, this classification is quite complex and cumbersome; we will not present it here in full, since only one third of it, belonging to group A, looks something like this:
Simplifying as much as possible, we can reduce ankle fractures to single/double/triple-malleolar fractures and their equivalents. Conservative treatment is only applicable in cases of unimalleolar fractures. In the conservative treatment of two- and three-malleolar fractures and their equivalents, secondary displacement is almost inevitable, which further leads to disruption of the relationship between the talus and the corresponding articular surfaces of the tibia and fibula, which in turn leads to improper load distribution and wear of the articular cartilage and the formation of post-traumatic arthrosis with severe impairment of the function of support and walking within 1-2 years after the injury. This is precisely what explains the increased interest of orthopedic surgeons in this type of injury over the past 2 decades.
The main goal of surgical treatment of an ankle fracture is to restore the normal relationship of the bones in the ankle joint. Even if the talus is displaced outward by 1 mm, the area of its contact with the tibial plateau decreases by 40%. It turns out that when the outer ankle is fused with a seemingly small displacement of 1 mm outward, 60% of the area will bear 100% of the load.
The second important point is to provide conditions for fracture healing due to close contact of bone fragments and their reliable fixation, preventing movement of fragments among themselves.
The third goal is to avoid immobilization. The plaster cast itself can cause significant harm to its owner in 6 weeks, leading to disruption of tissue nutrition, muscle atrophy, increasing the risk of deep vein thrombosis of the lower extremities, preventing movement in the joint, which can ultimately lead to its contracture. When osteosynthesis is performed correctly, movements in the ankle joint are allowed the very next day after surgery. You can see an article on surgery for an ankle fracture by following this link.
At our center, we try to provide assistance to patients with fractures of any location, including ankle fractures, as quickly and efficiently as possible. A complete preoperative examination and surgery are performed within the first 24 hours after presentation. In most cases, discharge under the supervision of a traumatologist at the clinic occurs on the second day after treatment and surgery. When you contact us, you will have X-rays taken to confirm the diagnosis, and transport plaster immobilization will be applied. Immediately before surgery, antibiotics are administered intravenously for prophylactic purposes. It is possible to use spinal anesthesia or endotracheal anesthesia. In order to reduce the stress from surgery, you will be put into a medicated sleep 10 minutes before the operation, and you will also wake up 10 minutes after its completion. During the operation, the orthopedic surgeon will perform an open comparison of the fragments with their fixation with plates and screws. You will need crutches after surgery, as full weight bearing is still not recommended until the fracture has healed. The next day after the operation, you will be bandaged, taught how to walk correctly with additional support on crutches and what exercises to do to develop movements and strengthen the muscles of the lower leg, after which you can be discharged home.
When an ankle is fractured, a surgical intervention is performed called: open reduction and internal fixation, or osteosynthesis. To access the broken bone, incisions are made outside the projection of large neurovascular bundles.
The broken bone is exposed, bone fragments are compared, and temporary fixation is performed using bone holders, knitting needles, and bone pins. Next, osteosynthesis is performed using plates and screws. The temporary fixation is removed.
Hemostasis is performed, the wound is sutured layer by layer, an aseptic bandage and elastic compression are applied.
After the operation, the leg should be elevated, ice is placed through a bandage on the surgical area (best is a soft rubber heating pad filled with ice and cold water) for 30 minutes every 3 hours. This helps reduce swelling and pain in the intervention area. After surgery, you will be given painkillers and anti-inflammatory medications. On the evening of the day of surgery or the day after surgery, a physical therapy instructor will teach you how to walk correctly with additional support on crutches and show you exercises that you will need to perform to maintain the mass and strength of the lower leg muscles. You will be bandaged the morning of the next day after surgery. After this, you can be discharged under the supervision of a traumatologist at your place of residence. At home, you should also continue to use limb elevation and ice to help swelling and pain go down more quickly. 2 weeks after the operation you will need to come to the clinic to have the stitches removed. After 6 weeks, X-ray control is performed and if there are signs of consolidation, weight bearing on the leg is allowed. It usually takes about 2 more weeks to fully restore limb function. At this stage, it is very useful to work with a physical therapy instructor. Forced (sports) loads on the leg are not recommended until 6-12 months after the injury.
There are a number of complications typical for any surgical intervention and for any type of anesthesia. Surgery for broken ankles is no exception. These include infection, damage to blood vessels and nerves, bleeding, and deep vein thrombosis. Their risk does not exceed 2% of the total number of interventions.
There are also specific complications. These include stiffness of the ankle joint, weakness of the lower leg muscles, and the formation of post-traumatic arthrosis of the ankle joint. These risks largely depend on the morphology of the fracture, the presence of concomitant diseases, such as diabetes, autoimmune diseases requiring steroid medications, and smoking.
The plates and screws used in modern surgical practice are made of either titanium alloy or surgical steel, which do not cause a reaction from the body. Their removal is indicated in cases where they cause irritation of soft tissues due to mechanical damage, in cases of infectious complications, as well as when the patient insists. It is also often necessary to remove the positioning screw after 6-8 weeks when fixing the tibiofibular syndesmosis. Complete removal of metal fixators for ankle fractures is recommended no earlier than 12 months after surgery.
Patient T., 80 years old. Trauma 3 weeks before treatment, she received a fracture of both ankles of the right leg with displacement, subluxation of the foot outward. I contacted the RTP, an X-ray was taken, and a plaster cast was applied. Due to persistent severe swelling and pain, she went to the K+31 clinic.
X-rays in the cast reveal a significant outward subluxation of the talus and a consolidating fracture of the lower third of the fibula.
On the day of presentation, the patient was thoroughly examined, surgical treatment was performed, open reduction, osteosynthesis of the fracture of the lower third of the fibula with a plate, the inner ankle with a screw, the inner ankle was additionally fixed with an anchor.
On control radiographs after surgery, the position of the fragments and metal fixators is correct, and the subluxation of the talus has been eliminated.
The patient was discharged on the 2nd day after surgery for outpatient follow-up care.
Patient L., 50 years old, injured at home, received a closed fracture of both ankles with a dislocation of the foot outward and backward. This case is interesting due to the significant damage to the soft tissue that occurred during the injury and required significant efforts to combat swelling, as well as the morphology of the fracture of the medial malleolus, which broke in one large block along with the posterior edge of the tibia, which required its fixation with a plate and screws.
Due to severe swelling of the soft tissues, a high risk of necrosis of the wound edges and infectious complications, the patient underwent skeletal traction, vascular and metabolic therapy, lymphatic drainage, and physiotherapy for preoperative preparation. After the swelling subsided, on the 3rd day after admission, surgical intervention was performed: open reduction, osteosynthesis of fractures of the outer and inner malleoli with plates and screws.
After 4 days, the patient was discharged for outpatient follow-up treatment. Postoperative wounds healed by primary intention, the sutures were removed after 14 days.
6 weeks after the initial intervention, the positioning screw was removed, and the patient began to actively develop movements in the ankle joint.
The range of motion 8 weeks after injury and surgery for this severe injury is close to full. The patient walks with full support, without using crutches or a cane, does not limp, and is not bothered by pain. Moderate swelling in the ankle joint remains.
You can see another article on ankle fractures here.
Contraindications
Skeletal traction is contraindicated for children under 5 years of age, elderly people over 60 years of age, as well as patients with severe infectious diseases and inflammation of the skin.
Such a procedure can greatly undermine the emotional state of the patient and his loved ones, but you need to reassure yourself that the treatment will not last forever and it is as effective as possible.
You may be interested
in Foot bruiseHow to distinguish a fracture from a bruiseRib bruise without a bruise, what to doWhat to do if you have a bruised tailbone