Condyle
- a paired fragment of the femur, which is located in its lower part and forms the knee joint. There are medial (closer to the median axis of the body) and lateral (side) condyles. Their fractures are divided into low- and high-energy, depending on the nature of the injury. An isolated fracture of one of the condyles or their combined damage may occur. some fractures are accompanied by the formation of fragments.
Causes of injury
- injury during sports activity;
- falling from height;
- accidents, traffic accidents.
During a car accident, hitting your feet on the front seat or dashboard is of great importance. if the legs are bent at the knee joint, a condyle fracture is more likely to occur. With strong impacts, the direction of the force also plays a role; this injury is characterized by a direct action in the lateral projection of the knee.
Low-energy trauma occurs from a minor impact or a normal fall. The main role here is played by a violation of the structure of bone tissue, which occurs with osteoporosis or as a result of age-related changes.
If an isolated fracture of the lateral condyle occurs, the most likely cause is a forced outward deviation of the tibia. If it moves in the medial direction, the fracture will occur in the area of the medial structure.
How to recognize a fracture of the femoral condyle?
- The main syndrome with this injury is pain. Localization of pain is the knee joint, which becomes smoother and loses its usual contours;
- Internal hemorrhage leads to tissue protrusion, swelling, and pain on palpation;
- Pressing on the patella makes it possible to feel its unusual position and how it “springs” under the pressure of the blood collected inside the joint;
- If the condyle is displaced, this is reflected in the deviation of the tibia to the side;
- The patient cannot make active movements, and passive ones cause severe pain.
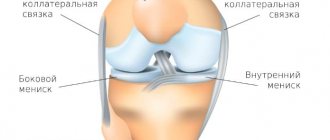
Similar symptoms accompany fractures of the patella, tibial condyles, as well as sprains of the knee ligaments and damage to the meniscus. Therefore, additional diagnostics are required to make an accurate diagnosis. The difference between fractures of the femoral condyles and damage to similar structures of the leg is the fact that in the first case the pain is localized above the joint space of the knee, and in the second - below it.
Osteoma of the condylar process of the mandible
Osteoma is a benign tumor of bone tissue, occurring in 2.7-5.9% of patients with benign tumors of the facial bones. Currently, it is suggested that the number of true osteomas is significantly smaller, since this diagnosis is often mistakenly made in cases of reactive hyperplasia, exostoses of the jaws, and some forms of fibrous dysplasia [3, 17].
Osteomas, as a rule, grow very slowly and painlessly, without making themselves felt for a long time. Their clinical picture is mild and depends on the location and size of the tumor. Developing in the area of the body of the lower jaw, osteomas lead to deformation of the corresponding area, aesthetic and functional disorders. Osteomas of the upper jaw with significant sizes cause exophthalmos, diplopia, lacrimation, impaired nasal breathing and neuralgic pain due to compression of the branches of the trigeminal nerve. When localized in the area of the frontal sinus and ethmoid labyrinth, the tumor is capable of deforming the walls of the sinuses, destroying them, growing into the orbit and cranial cavity [3, 15].
Damage to the condylar process of the mandible is quite rare and is characterized by specific symptoms. Osteomas of this localization present a certain difficulty for diagnosis and surgical treatment, remaining asymptomatic for a long time, but in later stages they can cause severe aesthetic and functional disorders [3, 9, 17].
Osteoma of the condylar process was first described in detail by Eckert (1899), pointing out displacement of the lower jaw, impaired mouth opening, as well as changes in facial contours on the side of the lesion of the condylar process of the mandible among its main clinical manifestations [1]. Subsequently, a few reports were presented in the literature, mainly about isolated observations of this disease [1, 11, 13, 14]. Deboise A. (1981), noting that osteoma is the most common benign neoplasm of the structures of the temporomandibular joint (TMJ), provides only 3 of his own observations [9]. The largest number of clinical observations of osteomas of the condylar process - 23 - belongs to H. Zhang (1997) [18]. The author, however, does not indicate whether in all cases the diagnosis of true osteoma was confirmed histologically.
Clinical observation
Patient K., 36 years old, medical history No. 4408 dated March 19, 2004, was admitted to the maxillofacial department No. 2 of City Clinical Hospital No. 12 in Kiev with complaints of facial deformation due to displacement of the lower jaw, malocclusion, difficulty chewing food, crunching in the left TMJ, moderate pain with increased load on the joint. For the first time, he noticed a facial deformity—a displacement of the chin to the right—in November 2002. Later, a clearer clinical picture emerged; the severity of the displacement and malocclusion slowly progressed until the moment of treatment. Objectively, the patient had pronounced facial asymmetry due to displacement of the lower jaw to the right (Fig. 1).
Rice. 1. The chin is shifted to the right side, a state of physiological rest.
In the pretragus area, the laterally displaced head of the left TMJ was clearly palpated. Mouth opening was up to 4.5 cm, with a crunch in the area of the left TMJ and a Z-shaped deviation of the lower jaw. Lateral movements of the jaw to the right were limited, the bite was oblique, and the midline shifted to the right by 1 cm (Fig. 2).
Rice. 2. In the pretragus area, the laterally displaced head of the left TMJ is clearly palpated.
A series of radiographs (orthopantomogram, radiograph of the mandible in direct projection and in the Haenisch position on the left, computed tomogram of the joint area with 3D reproduction) revealed a shadow of bone density with a size of 2x1.7 cm, associated with the left condylar process and located in the infratemporal fossa. The structures of the left TMJ were preserved, although somewhat deformed. When planning surgical intervention, a stereolithographic model of the patient’s skull was made (Fig. 3), on which the necessary measurements were made and the surgical approach was determined.
Rice. 3. Stereolithographic model of the skull, neoplasm of the left condylar process of the mandible.
On March 23, 2004, the patient underwent surgery: removal of a neoplasm of the condylar process of the lower jaw under endotracheal anesthesia with intubation through the nose. To do this, a preauricular and semicoronal approach was provided to the zygomatic arch, which was then resected and displaced downward on the fibers of the masseter muscle (Fig. 4).
Rice. 4. Surgical wound, coronal access, osteotomy of the zygomatic arch: 1 - zygomatic arch, 2 - osteotomy areas.
The fibers of the temporalis muscle were partially transected and detached, allowing access to the infratemporal fossa, where a bone formation was visualized anterior and medial to the head of the jaw (Fig. 5).
Rice. 5. The area of the infratemporal fossa, access to the tumor has been created.
The tumor is separated from the soft tissues and fixed using a special bone fixation made in the form of a corkscrew (Fig. 6).
Rice. 6. Macroscopic specimen of osteoma of the condylar process of the mandible.
The tumor was removed within the healthy bone. The zygomatic arch is placed in place and fixed with two wire bone sutures. The soft tissue flap was put in place, the wound was sutured in layers. The postoperative period proceeded without complications. Closing of the jaws in the correct position was noted the next day after surgery without any orthopedic measures (Fig. 7).
Rice. 7. State of physiological rest of the lower jaw on the first day after surgery. Closing of teeth in a physiological occlusion with restoration of the midline.
The radicality of tumor removal was confirmed by computed tomography data (Fig. 8).
Fig.8. Facial symmetry, state of physiological rest, 9 years after surgery.
Vertical movements of the lower jaw were fully restored on the 5th day. There was a slight paresis of the frontal and zygomatic branches of the facial nerve, the function of which was completely restored on the 7th day after surgery. Postoperative swelling of the temporal and zygomatic areas persisted for 8 days. On April 2, 2004, the patient was discharged in satisfactory condition with recommendations for rational prosthetics.
On January 16, 2013, patient K. underwent a repeated scheduled examination using clinical and instrumental research methods. The patient did not have any complaints from the TMJ. On bilateral palpation of the TMJ, no crunching or crepitus was observed, and there were no pain symptoms. Objectively: the contours of the face are symmetrical, the maximum opening of the mouth is 4 cm (Fig. 9, 10), the midline of the face is restored, the movements of the lower jaw are not limited, without signs of lateral deviation.
Rice. 9. Maximum mouth opening, 9 years after surgery. Rice. 10. Orthopantomogram, 9 years after surgery.
According to an orthopantomogram and computed tomography in 3D reconstruction mode, the structural elements of the left TMJ have clear anatomical contours and the structure of bone tissue is within normal limits. The relationship between the condylar process and the glenoid fossa ensured the functional stability of the TMJ and was considered acceptable (Fig. 11, 12).
Fig. 11. Computed tomography data. Rice. 12. 3D reconstruction of the skull, 9 years after surgery.
Discussion
Localization of osteoma in the TMJ region is a rare clinical situation. The paucity of clinical symptoms characteristic of osteomas determines the dominance in the clinical picture of nonspecific functional disorders of the TMJ, which makes it necessary to carry out differential diagnosis with other diseases of the joint - hyperplasia of the branch, deforming arthrosis, ankylosis, intra-articular disorders, habitual dislocation, etc. X-ray studies in standard settings are quite informative for making a correct diagnosis, but are clearly insufficient for choosing a method of surgical treatment. To clarify the localization of the tumor, taking into account the changed anatomical relationships, its relationship with the elements of the joint and the nature of structural changes in the latter, it is necessary to conduct computed tomography with 3D reconstruction. A thorough examination allows you to decide on further surgical tactics.
When the osteoma is anteromedial in relation to the condylar process, it is located in the region of the infratemporal fossa. Removing the tumor in this case is associated with significant difficulties, and sometimes even with a risk to the patient’s life. Chen Y. (2003) states that when the tumor is localized in the area of the articular process, in most cases its resection followed by arthroplasty and orthopedic treatment is indicated [8]. Other authors adhere to the same point of view, recommending combining resection of the condylar process with subsequent plastic surgery of the joint, lengthening of the ramus, combined operations on the upper and lower jaw to correct the bite and hardware treatment [4, 7, 18]. At the same time, the above observation indicates that in some cases it is possible and even necessary to remove the tumor while preserving the elements of the joint. This is also evidenced by the data of Piattelli A. (1995) and other authors [11, 13].
It should be noted, however, that when the osteoma is anteromedial in relation to the condylar process (according to the literature, this is the most typical localization), it is located in the region of the infratemporal fossa. This area is surgically extremely difficult to access and is located near vital structures, so removing the tumor in this case is associated with significant difficulties and sometimes even a risk to the patient’s life.
The main anatomical obstacles to reaching the infratemporal fossa are the zygomatic arch, the ramus of the mandible, the parotid gland and the facial nerve - formations that are extremely important in functional and aesthetic terms. Access to the tumor should be sufficient for its radical removal and provide a good overview.
Currently, a number of options for surgical access to the infratemporal fossa have been proposed, more or less satisfying these requirements, but not all of them are appropriate in the case of osteoma of the condylar process.
In 1961, JF Barbosa developed an approach to the infratemporal fossa, which involved performing a Weber-Fergusson incision followed by mobilization of the zygomatic complex and resection of the mandibular ramus [6]. DJ Crockett (1963), using a similar approach, limited the resection of the branch to the coronoid process only [10, 16]. This so-called anterior route is usually combined with maxillary resection and provides a wide view, but at the same time it is very traumatic and unfavorable from a cosmetic point of view. The infratemporal fossa can also be achieved by making a premaxillary incision followed by osteotomies of the mandibular ramus at various levels, rotation or removal of the bone fragment from the surgical site. In case of resection of a section of the branch, the latter can be returned to its place at the end of the operation and fixed in the form of a free autograft [16].
The main anatomical obstacles to reaching the infratemporal fossa are the zygomatic arch, the ramus of the mandible, the parotid gland and the facial nerve - formations that are extremely important in functional and aesthetic terms. In 1985, NR Attenborough proposed the use of a coronal approach to visualize the structures of the pterygopalatine and infratemporal fossa. This method involved making pre-auricular and semi-coronal incisions with subsequent removal of the zygomatic arch and coronoid process [5]. HL Obwegeser improved this technique by combining mobilization of the entire zygomatic complex with osteotomy of the coronoid process. In this case, the zygomatic bone was displaced downward on the fibers of the masticatory muscle, and the coronoid process was retracted upward [12]. In addition to the above, numerous modifications and combinations of access are used depending on the clinical situation [10]. As our experience shows, the use of coronary access is the method of choice when removing tumors localized in the infratemporal fossa. It provides a good overview and freedom of surgical manipulations, avoids injury to large vessels and branches of the facial nerve, and is also most cosmetically acceptable.
We also note that with long-growing bone tumors in the TMJ area, the joint can undergo significant morphofunctional changes that require postoperative orthopedic correction, however, as was shown in our observation, the compensatory capabilities of the joint are quite high, which in some cases with low-traumatic and radical removal tumor allows you to achieve restoration of function without additional measures in the postoperative period.
Thus, observation of the patient in the long term after surgery (9 years), indicating a relapse-free course and the absence of deep functional disorders, confirms the effectiveness of the approaches used to remove the TMJ tumor. Careful diagnosis and surgical intervention using approaches that provide wide access to the infratemporal fossa allowed for radical removal of osteoma of the condylar process of the mandible, while avoiding additional trauma to the anatomical formations of this localization, providing a quick postoperative recovery period and a satisfactory result for 9 years with complete restoration of TMJ function.
Diagnosis of pathology
Diagnosis is carried out on the basis of clinical data and additional research methods. The diagnosis begins with a patient interview and examination. The doctor notes visual signs of fractures characteristic of damage to the condyles. When collecting anamnesis, it is necessary to pay due attention to the nature of the injury received, so the patient must clearly describe it in a conversation with the doctor.
- The gold standard is to take a radiograph. The picture is taken in two projections - frontal and lateral. There are also additional research methods, but they are used less frequently.
- If the X-ray data is uninformative or there are doubts, a tomography is performed using a computer machine.
- Magnetic resonance imaging does not provide the necessary data on the condition of the bone; this method is used if there is a risk of damage to soft tissues and it is necessary to exclude their injury.
Modern methods of treating damage to the femoral condyles
Treatment of condyle injury is carried out in a hospital setting. If a patient is diagnosed with a fracture without displacement of bone fragments, treatment tactics consist of the following steps:
- evacuation of blood from the joint cavity;
- adequate pain relief;
- limb immobilization;
- if necessary, repeat joint punctures.
One of the important principles of treatment is to limit the load on the joint. The patient is recommended to follow a gentle regimen, walking with crutches for 2-3 months from the start of treatment.
If there is displacement of the fragment, manual reposition is performed under local anesthesia - that is, restoration of the anatomical position of the fragment. To do this, the doctor deviates the lower leg in the direction opposite to the injury. Correct movement engages the joint ligaments and the condyle itself “falls” into place. After manipulation, immobilization of the limb is still necessary.
Surgical treatment is required for some types of injury and when conservative methods are ineffective. The operation is performed early after injury and is accompanied by anesthesia.
Blood and small fragments are removed from the joint cavity. after this, the condyle is reduced and the displacement is eliminated. To strengthen the fragment, several metal screws are inserted into it. After suturing the wounds, a plaster cast is applied to the leg from the foot to the upper thigh.
Fractures in the knee joint
Thanks to the advent of new techniques and special materials, the results of surgical treatment of fractures have become better, even in patients with poor bone quality.
Timing of the operation. Most femoral condyle fractures are not treated immediately, with the exception of open fractures. Open fractures are characterized by the presence of communication between the fracture zone and the external environment. Such fractures require immediate surgical treatment.
In most cases, surgery is postponed for 1-3 days in order to choose the most optimal treatment plan and prepare the patient for surgery. Depending on your age and medical history, your surgeon may recommend further testing to ensure there are no significant health problems that need to be addressed before surgery.
External fixation. If there is significant damage to the soft tissue (skin and muscle) in the area of the fracture, or if your health makes you concerned about how you will cope with major surgery, your doctor may temporarily apply an external fixator. During this operation, metal needles or rods are inserted into the bones above and below the level of the fracture, which are fixed to an external fixation device. The latter is a frame that holds the bones in the correct position until you are ready for surgery.
An external fixator is used to temporarily stabilize the fracture before permanent fixation.
When you are ready for surgery, your surgeon will remove the external fixator and perform internal fixation of the fracture using some type of fixator.
Internal fixation. For fractures of the femoral condyles, the following fixation options are most often used:
- Intramedullary osteosynthesis. With this type of fixation, a special metal rod is inserted into the femoral medullary canal, which passes through the fracture area and fixes the fragments in the desired position.
- Bony osteosynthesis. During such an operation, the bone fragments are first returned to their normal position and fixed in this position on the outer surface of the bone with metal plates and screws.
With both fixation options, depending on the type of fracture and the fixator used, one large access or several small ones are performed.
Healed femoral fractures under conditions of extraosseous (left) and intramedullary (right) osteosynthesis.
In comminuted fractures, where there are many separate bone fragments, surgeons usually do not try to put them together like a puzzle. Instead, the surgeon uses a plate or rod that is secured above and below the fracture, leaving numerous bone fragments untouched at all. The goal of this operation is to restore the correct shape and length of the bone. The space between the individual fragments will eventually be filled with new bone tissue, called callus.
In comminuted fractures, the spaces between the individual fragments are filled with new bone tissue.
In cases where delayed fracture healing is expected, such as in elderly patients with poor bone quality, bone grafting may be performed to stimulate callus formation. The material for bone grafting can be taken from the patient himself (most often from the pelvis. It is also possible to use artificial bone substitutes for this purpose.
In the most severe cases of comminuted fractures and low quality bone tissue, when fixation of the fragments is impossible, they are removed and knee replacement is performed.
Fractures after knee replacement. Due to the aging population, the number of knee arthroplasty operations is increasing, and the number of fractures of the distal end of the femur in elderly patients who have previously undergone arthroplasty is also increasing.
Radiographs of a distal femoral fracture in a patient with a knee replacement.
For such fractures, intramedullary or external osteosynthesis is usually performed, as for conventional fractures of the distal femur. In rare cases, the original endoprosthesis is removed and replaced with a different version of the prosthesis. This operation is called revision of the endoprosthesis. It may be indicated when the components of the original prosthesis are destabilized or when it is impossible to fix the fracture using other methods.
Periprosthetic femoral fractures fixed with a plate, intramedullary rod, and also by revision knee replacement.
Surgical complications. You will be given antibiotics before surgery to prevent infection. You will also be prescribed anticoagulants (drugs that reduce blood clotting) to prevent blood clots from forming in the veins of the lower extremities.
Any operation is accompanied by some degree of severe blood loss. The amount of blood loss depends on the severity of the fracture and the nature of the operation. During the operation, the doctor will assess the amount of blood loss and, if necessary, give you a blood transfusion.