Lateral epicondylitis, also known as tennis elbow, is the most common elbow overuse syndrome. In this condition, the extensor tendons of the forearm are damaged. These muscles begin in the region of the lateral epicondyle of the humerus. Very often, the attachment site of the extensor carpi radialis brevis is involved in the pathological process.
Remember that only 5% of people suffering from tennis elbow attribute their injury to tennis! The main cause of epicondylitis is chronic contractile stress on the tendon at the origin of the muscle on the humerus. Lateral epicondylitis most often occurs due to repetitive stress involving the upper extremity, such as computer work, heavy lifting, sudden pronation and supination of the forearm, and repetitive swinging movements. It is also found in many other sports, including squash, badminton, baseball, swimming and throwing competitions. Also very often, lateral epicondylitis can be found in people whose profession involves performing frequently repeated movements with the same hand. Those at risk include electricians, carpenters, gardeners, and people with sedentary jobs.
Clinically Relevant Anatomy
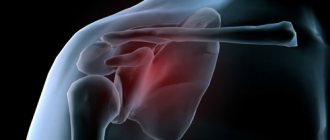
The elbow joint is formed by three bones: the humerus, as well as two bones of the forearm - the radius and ulna. In the distal part of the humerus there are two epicondyles: one is lateral, which is located outside, and the second is medial, it is located inside.
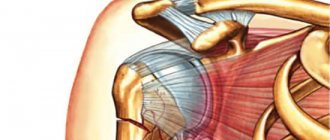
The area of maximum tenderness is usually the area at the lateral epicondyle, where the extensor muscles of the forearm begin. The extensor carpi radialis brevis muscle is most commonly affected, but the extensor digitorum muscle, extensor carpi radialis longus muscle, and extensor carpi ulnaris muscle may also be involved.
The radial nerve also passes in close proximity to this area, which here divides into the superficial radial nerve and the posterior interosseous nerve of the forearm.
Causes of fracture of the lower end of the humerus.
Most often, such fractures occur as a result of three types of trauma: a fall on the elbow joint, a direct blow, such as being hit by a bumper through a door during an accident, and a fall on a straight abducted arm, in which the ulna is wedged into the lower part of the humerus.
In the case of a low-energy fracture due to an ordinary fall, suspicions of osteoporosis always arise. A decrease in bone density leads to the fact that significantly less energy is required to obtain a severe fracture, which in the absence of osteoporosis would only cause a bruise.
Epidemiology/Etiology
Lateral epicondylitis is classified as an overuse injury. This condition can lead to hyaline degeneration of the origin of the extensor tendon of the forearm. Overuse of the forearm and shoulder muscles and tendons, repetitive contractions, and manual work with the arms can all put too much stress on the elbow tendons. As a result, damage occurs in the tissue structure, which in turn leads to pain over the lateral epicondyle. Most often, pain is located anterior and distal to the lateral epicondyle.
Friends, Anna Ovsyannikova’s seminar “Elbow joint and hand (Block 2)” will be held very soon as part of the RehabTeam project. Find out more...
Lateral epicondylitis is five times more common than medial epicondylitis (ratio varies from 4:1 to 7:1). It affects 1-3% of the population, mainly people aged 35-50 years. In patients under 35 years of age, it is necessary to differentiate the diagnosis from damage to the growth plate and referred pain in diseases of the cervical spine. If the patient is over 50 years old, then when making a diagnosis, osteoarthritis and referred pain from the cervical spine should be excluded. According to a study by Nirschl conducted in 1973, among 200 tennis players who were over 30, 50% had some stage of lateral epicondylitis.
Tennis elbow is an injury that is most often associated with professional activities. Risk factors include manual labor, housework, and other activities that involve wrist extension and forearm pronation and supination.
Lateral epicondylitis is equally common in both men and women. Most often, the disease is detected in patients aged 30-50 years. Damage to the lateral epicondyles of both hands is quite rare. Generally, tennis elbow affects the dominant hand. In 20% of cases, the disease persists for longer than a year.
A systematic review identified three risk factors for lateral epicondylitis:
- use of tools heavier than 1 kg;
- lifting weights more than 20 kg at least 10 times a day;
- repetitive, monotonous movements for more than 2 hours a day.
Other risk factors include: overuse, repetitive movements, training errors, body misalignments, flexibility problems, aging, poor circulation, strength deficits, muscle imbalances, psychological factors.
There are several opinions regarding the etiology of lateral epicondylitis:
Inflammation
Despite the fact that the very name of the disease indicates the presence of an inflammatory process, inflammation is present only at the initial stage.
Microfractures
Nirschl and Pettrone attributed the cause to microscopic tears at the origin of the extensor carpi radialis brevis muscle. According to the authors, reparative tissue (angiofibroblastic hyperplasia) is later formed at the site of the ruptures. This process, in turn, can lead to macrotears and structural damage to the origin of the said muscle.
- The assumption that micro and macro tears of the common origin of the forearm extensors are involved in the pathological process was made back in 1936 by Cyriax
- The first to describe macrotears in tendons in a histological report were Coonrad and Hooper
- Histological examination of tissue samples indicates "disorientation, disorganization and disintegration of collagen structures, increase in proteoglycans and volume of cellular contents, neovascularization, as well as partial necrosis." Nirschl named his histological findings angiofibroblastic hyperplasia. This name was later changed to angiofibroblastic tendinosis. The author noted that the tissue he studied was characterized by the presence of unorganized and immature fibroblastic and vascular elements. This loose gray tissue is found in tendon ruptures at various stages, including the extensor carpi radialis brevis tendon.
Degenerative process
Regan et al. studied the pathohistological features of 11 patients with lateral epicondylitis. They concluded that the cause of this condition is more likely to be a degenerative process in the tissues, rather than an inflammatory process. In lateral epicondylitis, there is an increase in fibroblasts, proteoglycans and glycosaminoglycans, vascular hyperplasia, as well as disorganized and immature collagen structures. It has been suggested that repetitive eccentric and concentric overload on the wrist extensor muscles may be the cause of angiofibroblastic tendinosis of the extensor carpi radialis brevis muscle. Epicondylitis is a degenerative condition in which fibroblast activity increases and granulation tissue forms within the tendon.
Circulatory disorders
The extensor tendons of the hand have areas with insufficient blood supply, and therefore the tendon system is not able to adequately respond to the repetitive loads carried by the muscles. As a result, this leads to a decrease in functional tolerance.
Possible complications
If there are complications, you should consult a neurologist.
The most common complication of a shoulder fracture is damage to the radial nerve. This is a particularly sensitive part of the nervous system, running in a spiral on the bone, innervating the muscles of the shoulder, forearm, and hand. Due to nerve damage, paresis occurs - partial impairment of the motor function of the injured arm or paralysis - complete immobilization of the limb. Signs of dysfunction of the radial nerve include:
- difficulties with extension of the wrist, fingers, elbow;
- constantly keeping the arm in a bent position;
- problems with finger movement - a person cannot grasp objects with them;
- decreased sensitivity of the skin in the back of the shoulder, forearm, and hand.
A neurologist treats the complication. The damaged nerve is restored with medications, physiotherapy, and vitamins. If you ignore the pathology, atrophy of the muscles of the right or left arm will develop over time.
Another complication of an epicondyle fracture is a false joint. This occurs due to the fact that a piece of muscle or soft tissue gets caught between the broken bone fragments, which greatly slows down the fusion process. In this case, surgical treatment is resorted to.
Clinical picture
The most prominent symptom of lateral epicondylitis is pain, which can be reproduced by palpating the extensor muscles of the hand at their origin on the lateral epicondyle. The pain may radiate up the shoulder and down the outside of the forearm, in rare cases radiating to the middle and ring fingers. In addition, a common symptom of tennis elbow is decreased flexibility and strength in the extensors of the hand and posterior shoulder muscles.
Read about compression of the ulnar nerve here.
Based on the severity of symptoms, Warren described 4 stages of disease development:
- Mild pain a couple of hours after the provoking activity.
- Pain immediately after completion of the provoking action.
- Pain during inciting activity that increases after the activity ends.
- Constant pain that makes any activity impossible.
In addition, patients note that their grip strength decreases and they also experience difficulty carrying things in their hands, especially when the elbow is extended. This is explained by weakness of the extensor muscles of the fingers and supinators of the forearm. Some patients experience a feeling of paralysis, but this is rare.
Symptoms last on average from 2 weeks to two years. 89% of patients recover within one year without any treatment (the only thing they may do is avoid painful movements and avoid sports injuries).
Prevention
- It is possible to avoid the development of epicondylitis of the shoulder if you load your arms moderately and protect the joints from injury or hypothermia.
- Before physical activity, you need to do a warm-up.
- You should consume foods containing calcium and vitamins more often.
- It is important to get rid of bad habits, since drinking alcohol and smoking contribute to poor absorption and excretion of calcium from the body.
At the first signs of epicondylitis, you should immediately consult a doctor.
Diagnostics
Making a diagnosis begins with determining your activity level, occupational hazards, participation in sports, medications, and other medical problems. During the physical examination, the doctor should feel the structures that form the elbow and other joints. It is also necessary to examine the muscles, bones, skin and nerves. It is very important to understand what types of activities cause certain symptoms and how they manifest themselves.
Research
If there is obvious pain in the lateral area of the elbow, studies are carried out quite rarely. However, in cases of long-standing disease, plain radiographs (in anteroposterior and lateral views) may help detect osteochondritis dissecans, degenerative changes in the joint, or indicate heterotypic calcification.
Another useful tool in the diagnostic process is ultrasound, which can show the extent of tendon damage, as well as the condition of the olecranon bursa.
Read about elbow ligament damage here.
- X-ray: Used to rule out elbow arthritis.
- MRI: ordered if symptoms are related to problems in the cervical spine. An MRI may show the presence of a herniated disc or symptoms of arthritis, both of which cause arm pain.
- Electromyography: needed to exclude nerve compression. There are many nerves in the elbow joint, and when they are compressed, symptoms similar to tennis elbow can occur.
Outcome assessment
- Assessing pain intensity: Numerical Pain Rating Scale (NPRS).
- Visual analogue scale (VAS).
- Upper limb functional index (ULFI).
- Patient Rated Tennis Elbow Evaluation (PRTEE)
- QuickDASH (Disabilities of the Arm Shoulder and Hand) scale.
- Patient Functional Scale (PSFS) – this scale has not yet been validated specifically for lateral epicondylitis, but has been used successfully in conditions such as knee dysfunction, cervical radiculopathy, acute low back pain, mechanical low back pain, cervical dysfunction spine. (Intraclass correlation coefficient (ICC) pain = 0.89-0.99, Functional ICC = 0.83-0.99, Overall ICC = 0.89-0.99).
Survey
The basis for the diagnosis of lateral epicondylitis is tenderness over the area where the extensor carpi radialis brevis and other extensor muscles of the hand begin. The examining physician or physical therapist should reproduce the typical pain syndrome using the following methods:
- Dynamometer and Patient-rated Tennis Elbow Evaluation Questionnaire (PrTEEQ) is a special questionnaire where the patient himself evaluates the condition of his elbow. These instruments help determine the severity of lateral epicondylitis. Using a dynamometer, you can measure the compression force. The PrTEEQ is a 15-question questionnaire that assesses forearm pain and movement impairment in patients with lateral epicondylitis. The questionnaire contains two scales – pain and functional. The patient is asked to rate the level of pain on a scale from 0 to 10, where 0 is no pain and 10 is the worst possible option. On the functional scale, 0 is given if the movement is given without difficulty, and 10 if it is impossible to perform it.
- Cozen's test: The Cozen's test is also known as the wrist extension test against resistance. It is performed as follows: the elbow is stabilized in a position of flexion at an angle of 90 degrees. With one hand, the doctor palpates the lateral epicondyle, and with the other, he moves the patient’s hand into a radial deviation position and the forearm into pronation. The patient is then asked to resist wrist extension. The test is considered positive if the patient experiences sudden, sharp and severe pain over the lateral epicondyle.
- Chair test: The patient stands behind a chair and grasps the back of it. His task is to lift the chair with three fingers - thumb, index and middle, while the elbow must be fully extended. The test is considered positive when pain occurs in the area of the lateral epicondyle.
- Mill's Test: The patient is seated, the arm being tested is relaxed, and the elbow is extended. The doctor passively pronates the forearm while simultaneously flexing the hand at the wrist joint. The test is considered positive for lateral epicondylitis if the patient experiences pain at the lateral epicondyle or more proximally at the musculotendinous junction of the wrist extensor muscles.
- Coffee Mug Test: (By Coonrad and Hooper) - The patient is asked to rate pain on a scale of 0 to 10 while performing a specific activity, such as picking up a full cup of coffee or a bottle of milk.
Classification of humeral condyle fractures.
There are several different classifications of humeral condyle fractures. They can be divided into supracondylar fractures, distal unicondylar fractures, for which Milch proposed a separate classification system, with a fracture of the lateral condyle more often occurring.
Distal humeral condyle fractures can be subdivided depending on what fragments were formed during the fracture according to the Jupiter classification. The 5 main articular fragments include: humeral head, lateral trochlea, lateral epicondyle, posterolateral epicondyle, posterior trochlea, medial trochlea, medial epicondyle.
Classification of humeral condyle fractures AO\OTA
Includes three main types - extra-articular, partial intra-articular and intra-articular fractures and three main subgroups in each type depending on the degree of fragmentation of fragments, displacement, and the structures involved.
The Jupiter classification of humeral condyle fractures examines in more detail the various morphological types of fractures involving both columns of the distal humerus. It distinguishes the following types of fractures:
High T-shaped (above or at the level of the upper edge of the olecranon)
Low T-shaped (at the level of the fossa, above the block)
Y-shaped (2 oblique fracture lines pass through both columns and connect on the block in one line)
H – shaped (multi-fragmented, the block is a separate fragment, high risk of avascular necrosis)
Medial lambda type – fracture of the trochlea and medial column
Lateral lambda type – fracture of the trochlea and lateral column
Treatment
Listen to a podcast about the elbow joint.
Conservative treatment
Conservative treatment of lateral epicondylitis is based on the following principles: pain reduction and inflammation control. The first principle is achieved through rest and avoidance of activities that provoke pain. NSAIDs will help prevent inflammation in the acute stage. It is also recommended to apply ice 3 times a day for 15 minutes, as cold reduces the level of chemical activity and also constricts blood vessels, which helps reduce swelling. An elevated position is also indicated for swelling of the wrist joint or fingers.
The use of a special bandage may be useful, since in this case it will act as an additional attachment point for the muscles and thereby relieve tension in the area of their origin on the lateral epicondyle. The bandage is secured around the forearm (below the head of the radius) and tightened so that the patient is unable to fully contract the extensor muscles of the hand.
Injections should be administered subperiosteally at the origin of the extensor carpi brevis muscle. Such injections give a quick and positive effect. In the first 24-28 hours, the patient's pain may increase. Steroid injections should be administered 1-2 weeks after rest and should be repeated no more than twice. Apparently, the effect of these injections lasts about three months, provided that the patient performs the exercises in parallel.
Surgery
If conservative treatment does not produce results and the symptoms of lateral epicondylitis persist, the patient may undergo surgery. Usually it is decided upon after 6 months of conservative treatment.
In most cases, surgery for tennis elbow removes the damaged muscle tissue and restores the attachment of the extensor muscles to the bone. The optimal surgical approach is different for each patient and depends on many factors, such as the severity of the injury, general health, and the patient's needs.
Open surgery. The most common type of surgery for lateral epicondylitis is open surgery, which involves making an incision above the elbow. This surgery usually takes place on an outpatient basis and does not require an overnight hospital stay.
Arthroscopic surgery. Tennis elbow can be treated arthroscopically, using tiny instruments and small incisions. As with open surgery, it is performed on an outpatient basis.
Physical therapy
There are different types of treatment for lateral epicondylitis, but they all have the same goal: to reduce pain and improve function. General physiotherapy treatment includes:
- Education and consultation on pain control, as well as modification of patient activities.
- Manual therapy: Mulligan – mobilization with movement
- Exercises – stretching and strength.
- Other methods of exposure: ultrasound, transcutaneous electrical neurostimulation (TENS).
- Bandages/splints/patch – no clear evidence of effectiveness.
- Medicines - NSAIDs provide a short-term effect (reduction of pain for 3-4 weeks).
- Corticosteroid injections – short-term effect (less than 6 weeks).
- Rehabilitation taking into account the type of sport and profession.
Evidence base for physical therapy
A study by Nagrale et al. shows that for lateral epicondylitis, Cyriax physiotherapy works better than phonophoresis and exercises. When controlled over time, the results of the group where Cyriax therapy was used were significantly higher in all parameters (p<0.05). Rajadurai et al. show that a supervised exercise program may be the first line of treatment for tennis elbow compared with Cyriax physical therapy. Much more research needs to be done to prove the effectiveness of manual techniques such as Cyriax therapy.
Physical therapy interventions, including elbow mobilization with movement combined with exercises, have been shown to work better than corticosteroid injections alone. True, the effect of physical therapy was greater for 6 weeks, but not for 52 weeks. Recent evidence suggests that combining cervical and thoracic joint mobilization with local therapy improves strength and endurance and reduces pain during exercise. With local therapy of the elbow alone, the results are worse.
Corticosteroid injections have a short-term positive effect, but in the medium term their effect is negative. Data on long-term effects are conflicting. Various treatments, as well as exercise and stretching, have short-term effects. The latter, however, also have a long-term effect.
It has been proven that physical therapy, which includes only ultrasound, massage and exercise, is no better than the “wait and see” method. Modifications to the patient's activities, as well as the use of a special bandage if necessary, help prevent recurrent episodes of lateral epicondylitis.
Extracorporeal shock wave therapy
Shockwave therapy is a treatment modality for multiple tendinopathy that can be used to treat lateral epicondylitis. In ESTW, patients are exposed to strong mechanical wave impulses. Statistical analysis of the visual analogue scale, DASH questionnaire and compression test show a significant difference between the results of the control and study groups both after treatment and after 6 months (P < 0.001). ESWT helped reduce pain, had a positive effect on functional impairment, and also improved compression test scores in patients with tennis elbow.
Although this technique is reported to be safe, there is a potential for hemorrhage and local soft tissue damage from cavitation, and this appears to be more likely at high doses. Studies have shown that in patients with lateral epicondylitis, extracorporeal shock wave therapy provides a significant placebo effect at moderate doses. However, there is no evidence of additional benefit from the treatment compared to placebo. This may account for the significant improvements observed in other studies.
Cyriax Physical Therapy
This is a very common type of intervention that combines deep friction massage with transverse friction with Mill's manipulations, which were successfully used by James Cyriax in the treatment of patients with lateral epicondylitis. Both of the above components of treatment should be used together in the specified sequence. The patient must follow the protocol three times a week for four weeks.
This therapy has several contraindications: an infectious process in the active stage; bursitis, disorders of nervous structures, ossification and calcification of soft tissues, active rheumatoid arthritis, taking anticoagulant drugs. Rajadurai et al. demonstrate that a supervised exercise program may be the first line of treatment for tennis elbow rather than Cyriax physical therapy. Much more research needs to be done to prove the effectiveness of using manual therapy such as Cyriax physical therapy.
Friction massage with transverse friction
Deep friction massage with transverse friction (DTF) is a special type of connective tissue massage that is used when working specifically with soft tissue structures. The clinician should try to achieve pain relief by using DTF techniques at the site of the lesion for 10 minutes until the patient begins to feel numb. The purpose of this procedure is to prepare the tendon for Mill's manipulations. Pain during friction massage indicates that the procedure is being performed incorrectly. There should be at least 48 hours between two massage sessions.
The purpose of deep friction massage with transverse friction is to maintain the mobility of soft tissue structures. Apparently, such massage also has an analgesic effect due to the regulation of nociceptive impulses (according to the gate control theory). The effect is also explained by the fact that the fibrils of connective tissue take the correct position, scar tissue softens, and blood circulation improves. However, research on this topic still needs to be conducted.
The Mill technique is carried out as follows. The patient's arm is supinated and the elbow is bent at an angle of 90 degrees. The area of maximum tenderness is located on the lateral epicondyle and the DTF technique is applied there. The tip of the thumb should be on the epicondyle and directed posterior to the osteotendinous junction. The other hand stabilizes the patient's wrist.
The Mill Manipulation is the most common technique used by physical therapists. It is a low-amplitude trust technique performed at high speed with maximum elbow extension and simultaneous flexion of the wrist and arm. The purpose of the technique is to stretch the scar tissue by breaking the adhesions in the area of the bone-tendon junction, which will make this area mobile and painless. In a certain sense, this technique is used as an imitation of the spontaneous recovery mechanism.
Mill's idea was to move the annular ligament of the radius and replace it. And Cyriax discovered that the tensile force of the annular ligament most affects the flexor carpi radialis. That is why the manipulation should be carried out with a jerk - to open the gap in the tendon and relieve tension from the scar tissue, transforming the gap.
This manipulation can only be used if the patient’s elbow can be fully straightened painlessly, and if the specialist knows the correct technique. To avoid worsening, the patient's wrist should be kept in full flexion. When performing the technique, the patient sits, his injured arm is abducted 90 degrees and is in a position of internal rotation (the articular process looks up). The specialist stands behind the patient, pronates and flexes the wrist with one hand, and places the other hand on the articular process. The patient's wrist must be fully flexed, otherwise the entire tensile force will be placed on the shoulder joint. In the position of maximum elbow extension, the specialist jerks the trust technique with a small amplitude (the so-called “high-velocity low amplitude (HVLA) thrust”).
During this procedure, the patient may experience slight discomfort. The procedure should be performed 2-3 times a week until complete recovery (number of sessions – 4-12).
Physical exercise
Exercise therapy is a specific regimen or plan of physical activity, developed and prescribed to achieve specific medical goals. The purpose of these exercises is to restore normal function of the musculoskeletal system or reduce pain caused by diseases or injuries. Work on developing strength, endurance and mobility should begin once pain and inflammation are under control.
Stretching
The literature on lateral epicondylitis suggests that the most important components of a physical therapy program are strengthening and stretching exercises. This is explained by the fact that the tendons must be not only strong, but also flexible. Stretching exercises are aimed at improving the flexibility of the wrist extensor muscle group. These exercises should be done until the range of motion in the wrist of the injured hand is equal to that of the healthy hand.
The fundamental principle of the stretch phase is that by lengthening the tendon during rest, we can reduce its stretch during movements that cause pain. The best position for stretching the extensor carpi radialis brevis tendon is with the elbow in extension, the forearm in pronation, and the wrist in flexion and in ulnar abduction as far as the patient's condition allows. This exercise should be done for 30-45 seconds 3 times before and after eccentric exercises, as well as during each treatment session with a rest interval of 30 seconds.
Other programs say that stretches for the wrist and finger extensor muscles should be done with the elbow extended and the wrist in palmar flexion. At the point of maximum painless stretching, you should linger for 15-25 seconds. These exercises should be performed 4-5 times a day (2 sets of 10 repetitions). At the first sign of pain, the patient should stop. At this stage of treatment, the patient should perform isotonic exercises once a day according to the following plan:
- Stretching exercise - repeat 10 times (15-25 seconds).
- Isotonic exercises – repeat 15 times (3 sets).
- Stretching exercises - repeat 10 times (15-25 seconds).
- Applying cold – massage the painful area with a piece of ice for 10-15 minutes.
Eccentric exercises
There are three main principles of eccentric exercise: load (endurance), speed (speed), and frequency.
- Load (endurance): Increasing the load ensures that the tendon is subjected to more stress, which forms the fundamental basis for the development of the exercise program. The basis of all exercise programs is this principle of progressive overload. Based on the patient's symptoms, the load in eccentric exercises should be gradually increased. Without this increase, there is a high risk of re-injury.
- Speed (quickness): Speed (quickness) is also one of the fundamental principles of a successful eccentric exercise program. With each session, the speed of the exercises should increase. Consequently, the load on the tendon will increase, which will stimulate the mechanism of injury. However, practitioners should be careful to ensure that patients perform eccentric exercises slowly to avoid pain.
- Contraction frequency: The third principle of eccentric exercises is contraction frequency. In the literature you can find a variety of variations of sets and repetition schemes. According to doctors, the patient can normally perform 3 sets of 10 repetitions without overloading the damaged tendon. The elbow should be fully extended, the forearm should be pronated, and the arm should be supported. The greatest results in strengthening the wrist extensor tendons are achieved in this position. Please note that this is a recommendation and the frequency of exercises should be selected individually for each patient.
Exercises with expander bands
Exercises with elastic bands (or light weights) should be performed every day 3 times for 10 repetitions. The patient fixes one end of the tape under his feet (or in another way), and holds the other end with his free hand. You can also use small dumbbells.
The patient begins the wrist flexion exercise, then does wrist extension and very slowly returns to the starting position. This exercise is concentric and eccentric for the wrist extensors.
Controlled exercises consisting of static stretching and eccentric strengthening are thought to have the greatest effect in reducing pain, strengthening, and improving function. After the patient has mastered this exercise, he can move on to a different color (tighter) band, or take on additional weight.
In one study, subjects were divided into groups A and B. In group A, patients underwent a supervised program of therapeutic exercises, including static stretching of the extensor carpi radialis brevis followed by eccentric strengthening of the extensor carpi muscles. Group B was treated with Cyriax physiotherapy. Group A, which completed a 4-week supervised exercise program, showed significantly greater improvements in pain reduction and functional status than those treated with Cyriax therapy.
Exercises with Flexbar
Exercises with the Flexbar® resistance stick are a useful and effective eccentric exercise for patients with lateral epicondylitis. This resistance band is easy to use at home and is an excellent example of true “evidence-based practice” in physical therapy. Exercises with it are performed in stages:
- Grasp one end of the FlexBar® with your affected (right) hand. Make sure your wrist is fully extended.
- With your healthy hand, grab the other end of the resistance band.
- Use your healthy wrist to twist while holding the FlexBar®.
Exercises with the FlexBar® resistance band should be done daily, performing 3 sets of 15 repetitions. It should take 4 seconds to complete one repetition, with a 30-second rest between sets. Once the patient can perform 3 sets of 15 repetitions, they can move on to the FlexBar with a higher level of eccentric resistance. Treatment should continue until the patient experiences regression of symptoms, which on average requires about 7 weeks of therapy and 10 clinic visits.
Taping
Taping with rigid tape (so-called diamond taping) may be useful in reducing pain, improving grip strength and functional characteristics of the elbow joint.
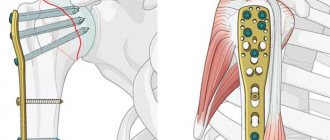
Features of using pins
During intraosseous surgical treatment, pins are inserted into the medullary cavity of the long parts of the tubular bones. The advantages of the technique are low trauma, the ability to put a load on the injured limb after just a few days. The operation is performed for transverse bone fractures with sufficient volume of the bone marrow cavity. For more durable fixation, pins with holes for screws are used, which are passed through the bone. This is BIOS, that is, blocked intramedullary osteosynthesis. Self-locking Fixion pins are also used. They allow you to perform the operation as quickly as possible and are used even for comminuted fractures.
External fixation devices (percutaneous technique)
The technique allows you to reposition and carefully fix the fragments without exposing the fracture area. Its essence is to pass rods or knitting needles through the bone tissue, which are fixed externally in a special apparatus. Now there are monolateral, circular, sector, semicircular, bilateral and combined devices. Preference is often given to rod models. The use of external fixators is an indispensable method of treating highly sensitive injuries, such as mine explosions and gunshots, which are accompanied by significant damage to both bones and soft tissues. The peripheral blood supply to the limb must be preserved.