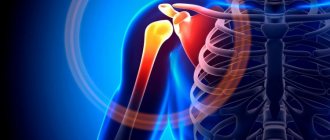
Osteoarthritis belongs to the group of diseases of non-infectious nature. Accompanied by the destruction of cartilage tissue that covers the surface of the joints. The inflammatory process is either absent or mildly expressed. According to WHO statistics, the disease occurs at different stages in 10% of the population in different countries. At the initial stage, pain is tolerable. As it progresses, the functionality of the shoulder joint decreases. Osteoarthritis is also called “deforming arthrosis.” It is common in the group of rheumatoid diseases.
Information about the disease
Arthrosis of the shoulder joint is an extremely unpleasant phenomenon that changes the usual way of life. Chronic degenerative disease affects cartilage tissue. The earlier a pathology is detected, the easier it will be to cure it and save yourself from the consequences and complications. In advanced cases, patients have to decide to replace joints with endoprostheses. Women over 40 years of age and during menopause are at risk. According to statistics, men experience arthrosis half as often.
Key points:
- Patients suffering from painful shoulder symptoms that last 3-4 years may find it extremely difficult to treat adhesive capsulitis/scapulohumeral periarthritis/frozen shoulder (FS).
- Currently, research continues to understand and study the pathology of frozen shoulder.
- Effective clinical protocols for treating frozen shoulder include a multi-model approach, a variety of modalities including intra-articular injections, physical therapy, manual therapy, home exercises, and a stretching program.
“Frozen shoulder” (adhesive capsulitis) is a unique and “mystical” pathology. Characterized by severe shoulder stiffness, pain, and loss of range of motion. Signs and symptoms usually begin gradually and get worse over time. Patients sometimes experience functional limitations that can last 3-5 years. It is estimated that 5% of the population will experience frozen shoulder during their lifetime. The spread of adhesive capsulitis is most common in women, obese people and diabetics.
What are the causes of osteoarthritis?
Osteoarthritis of the shoulder develops gradually. Initially, a person is bothered by discomfort and mild aching pain, but gradually the head of the bone and the glenoid cavity of the scapula undergo degenerative changes in the cartilage tissue. This occurs due to functional and mechanical overload. Cartilage must be resilient and elastic, but with deforming arthrosis these properties are lost. Impaired joint mobility is a direct consequence. Gradually, more and more surrounding tissues are involved in the process, and the pain becomes constant. The causes of this condition can be injuries, metabolic disorders in the body, excess weight, low physical activity, and pathologies of the musculoskeletal system. Do not forget about age-related changes and genetic predisposition.
Shock wave therapy: panacea or myth?
The shock wave therapy technique is used in the treatment of pathological changes in joints and cartilage; it is suitable for the treatment of shoulder pain. Shock waves are essentially high-energy sound waves that are specifically sent to the affected tissue areas. The liquid media of the body itself transfer the energy of wave impulses. Solid, foreign bodies are destroyed under the influence of shock waves.
The method helps with inflammation in the shoulder joint. It starts metabolism, causes mechanical irritation of tissues, and promotes their restoration.
Stages of shoulder osteoarthritis
The disease has 2 stages of development, which determines the severity of the deformation process. A correct diagnosis can be made only after an instrumental examination of the patient. Osteoarthritis of the shoulder joint of 1st degree is manifested by a slight narrowing of the joint space and single bone outgrowths. At this stage, moderate pain appears, which occurs mainly after physical activity. It is important that at the initial stage, patients have a good prognosis for recovery.
Osteoarthritis of the 2nd degree of the shoulder joint is characterized by an even greater narrowing of the joint space. Dead parts of cartilage tissue fall off, creating mechanical trauma. Getting between the bones, they intensify the inflammatory process. The pain syndrome becomes constant, joint mobility is completely impaired, which leads to the abandonment of many usual activities in everyday life. When the pathological process is advanced, the arm muscles undergo atrophy.
Prevention methods
The main preventive method is reasonable physical activity. If professional duties require stress, you need to remember about rest and relaxation. It is also important to monitor the condition of the spine, because incorrect position of the neck and back for a long time can also cause the disease. Excessive sports loads can lead to sprains, torn ligaments and muscles, and other types of injuries - so it is better to conduct training under the guidance of experienced trainers.
Remember: with glenohumeral periarthritis of the shoulder joint, the pain can be so severe that it will prevent you from doing your usual activities. It is better to prevent a disease than to treat it.
If the disease does affect you, and you are bothered by pain when raising your arms or putting your hand behind your back, do not put off visiting a doctor. The sooner therapy is started, the greater the chance that you will be able to get rid of unpleasant symptoms quickly and completely.
Registration for treatment of glenohumeral periarthritis in our clinic in Moscow is made by calling the numbers listed on the website. Waiting for you!
Information about treatment methods and diagnostics
At the earliest stage, it is difficult to determine the disease. For this reason, people seek medical help already at an advanced stage of osteoarthritis of the shoulder joint. Diagnosis begins with an analysis of the patient’s complaints (history collection). To make a diagnosis, an X-ray and ultrasound of the joints, CT or MRI will be required. The main task is to identify typical degenerative changes. Radiation methods make it possible to determine the condition of the joints long before the onset of pain, which already indicates the fact of deformation of the cartilage tissue.
How often to take a course of injections
Unlike drugs with hyaluronic acid, Noltrex has a much more prolonged effect. It is recommended to administer it at intervals of 9 months to 2 years, depending on the degree of damage to the shoulder joint. The medicine is of synthetic origin, therefore it is not detected and is not rejected by phagocytes - the immune cells of the body. This explains the long-term therapeutic effect.
Of course, any treatment for arthrosis will be effective only if the load on the joint is reduced. In the case of a shoulder, the prognosis is always favorable, especially if you seek help in a timely manner, without waiting for critical symptoms. “It will hurt and stop” - with this diagnosis, such an option, unfortunately, is excluded.
Shoulder pain does not always indicate the onset of arthrosis. Sometimes the reason is, indeed, a joint overwork, an uncomfortable position during sleep, or being in a draft. But much more often, pain is caused by other serious diseases, such as cervical osteochondrosis or glenohumeral periarthritis. Do you feel discomfort? Consult a specialist!
How can osteoarthritis be treated?
Osteoarthritis of the shoulder joint requires complex treatment. Ointments with an analgesic effect alone are not enough. Treatment consists of several stages:
- drug therapy (NSAIDs, corticosteroids, chondroprotectors, B vitamins, therapeutic blockades);
- physiotherapy (phonophoresis, myostimulation, shock wave and laser therapy, ozone therapy);
- physical therapy and massages.
For shoulder osteoarthritis, therapeutic exercises are carried out at the stage of pain reduction. The training is gentle. By strengthening the muscles, future attacks of osteoarthritis are delayed. What exercises can be performed should be shown by a physical therapy specialist. For people with this diagnosis, it is recommended to include in the diet foods rich in collagen compounds: meat, bananas, seafood, watermelon, dried fruits.
Shoulder pain (between old cliches of glenohumeral periarthritis and new data on NSAID therapy)
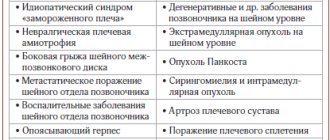
Pain syndrome, different in etiology and pathogenesis, develops both independently and against the background of other diseases and is the main reason for visiting a doctor, regardless of the nature of the disease. It forms all known types of pain: nociceptive, as the most significant and triggering a cascade of reactions, as well as psychosomatic and psychogenic. Pain develops, as a rule, gradually, slowly, often as a result of systematic muscle strain against the background of a decrease in general physical activity, but sometimes vice versa, with activity that is not comparable with the capabilities of the muscles. The pain is disturbing both at rest and during movement, rarely changing in intensity and character. In this case, overt or hidden depressive reactions can play a certain role in maintaining, and often intensifying, the pain syndrome. This significantly limits the patient’s usual life [1,2]. In 1872, S. Duplay first described shoulder pain under the term “scapulohumeral periarthritis.” The name “periarthritis,” which was apt at the time of this author, later became a hindrance in the study of pain in the shoulder joint. The doctor, making a diagnosis of “scapulohumeral periarthritis,” frees himself from the search for clinical symptoms that allow him to deepen and detail certain manifestations of the disease in this area. Under this name they began to hide ignorance of the causes of pain, and the diagnosis of “periarthritis of the shoulder joint” became, in the figurative expression of JN Pender, “a waste paper basket.” The variety of lesions of the paraarticular structures of the shoulder joint is associated with the peculiarities of its anatomical structure, which is multi-axial, hanging, and spheroidal. A large range of movements in the shoulder joint is achieved due to the developed, but fragile and easily vulnerable auxiliary periarticular apparatus. The articular fossa, although it is expanded due to the fibrocartilaginous articular lip, remains small, the joint capsule is weak and thin. The large subacromial bursa allows for smooth gliding between the rotator cuff (which primarily provides stability to the joint and depends on the muscles that make it up) and the inferior surface of the acromion process. Its expansion in the lateral direction forms a subdeltoid synovial bursa. The shoulder girdle is somewhat strengthened by the flat, synovial acromioclavicular joint, which allows the collarbone to slide along the acromion process. The stability of the acromioclavicular joint is ensured by the coracoclavicular and acromioclavicular ligaments [3]. Pathology of the shoulder and the broader concept of the shoulder girdle, considered in the structure of soft tissue diseases (M70–M79 ICD-10), occurs at the age of 40–70 years, the prevalence is 10% of those visiting a doctor at a therapeutic appointment. Moreover, this pathology occurs more often among women than among men. This group includes the most common pathology of the shoulder joint (M75) in the form of adhesive capsulitis of the shoulder, clinically manifested by periarthritis or the most pronounced articular functional disorders of movement with the characteristic “frozen shoulder” syndrome, as well as biceps tendonitis, calcific tendinitis of the shoulder, bursitis, retractile capsulitis and rotator cuff syndrome. Numerous proposals for the classification of periarticular lesions of the shoulder joint consider “subacromial syndrome”, but this does not solve the issue of creating a more or less complete classification according to the nosological principle of pathological processes that cause pain in the shoulder joint [4]. The causes of periarthritis of the shoulder joint are not completely clear, primarily due to the diversity of its clinical variants. Often, shoulder pain is provoked by acute direct and indirect trauma, chronic microtraumatization of the structures of the shoulder joint, including the muscle capsule, and weakening of the ligamentous apparatus of the shoulder and acromioclavicular joint with prerequisites for the development of reflex antalgic contracture. The disease usually occurs during or after physical exertion associated with professional sports or work, accompanied by prolonged stereotypic movements in the shoulder joint. The disease is provoked by age-related changes in soft tissues, congenital defects or structural features of the joint, skeleton, ligamentous-muscular apparatus (short coracoacromial ligament, crescent acromion, hypermobile syndrome, disturbances in the alignment of the head of the humerus in the joint) [5]. Risk factors for the development of adhesive capsulitis include female gender, old age, a history of shoulder injury and surgery, as well as diseases such as diabetes mellitus, heart and lung pathology, cerebrovascular accident and hemiplegia, and thyroid disease. Damage to the shoulder joint is observed in osteoarthritis, inflammatory rheumatic diseases involving the joints, including crystalline arthritis. That is, the pathogenesis of various forms of periarthritis of the shoulder joint includes infectious, degenerative-dystrophic processes, immune mechanisms of inflammation, and metabolic and neurotrophic disorders that have not yet been fully studied. The development of periarthritis of the shoulder joint can be caused by acute myocardial infarction, damage to the lungs and pleura, pathology of the gallbladder and other diseases of the internal organs. The chronological relationship of the occurrence of periarthritis of the shoulder joint after acute cerebrovascular accident served as the basis for the Pan-European Consensus Meeting on the Management of Patients with Stroke (Helsingborg, Sweden, November 8–10, 1995) to recognize frozen shoulder syndrome as one of the key indicators of stroke complications. To clarify the nature of the lesion in periarthritis of the shoulder joint, various propaedeutic approaches are used in the study of pain. Pain, muscle weakness and limitation of movement can be assessed by asking you to raise your arms or each arm individually above your head. Palpation definition of “pain pattern” according to I.I. Rusetsky with the definition of the most painful points - “the peaks of the pain pattern.” The use of the old palpation diagnostic method makes it possible to successfully differentiate some nosological forms included in the group of periarthritis of the shoulder joint [6]. Pay attention to muscle atrophy and neurological symptoms. Rarely, some swelling of tissue in the anterior or superolateral region of the shoulder joint can be noted, caused by synovitis of the glenohumeral joint. And the study of synovial fluid obtained during puncture of the shoulder joint allows us to classify these changes into inflammatory, non-inflammatory and septic. Each type of synovial fluid change is characteristic of a spectrum of diseases. Careful palpation of the muscles and tendons of the shoulder with complete relaxation of this area helps to establish signs of inflammation of the synovial bursae or tendons, most often when the subacromial bursa or the tendon of the long head of the biceps muscle is affected. In the topical diagnosis of pathological changes in the structures of the shoulder, the Dowborn test, also called the “painful arch symptom”, “collision symptom”, impingement shoulder syndrome, is effective. The occurrence of pain during arcuate abduction and lifting the arm up to a position from 60° to 120° across the side in the frontal plane suggests pinching of the subacromial bursa between the acromion and the greater tubercle of the humerus and the development of inflammation. Pain when raising the arm up to 160°–180° is explained by the pressure of the humerus on the acromial clavicular joint and in most cases suggests the presence of osteophytes, which is usually confirmed by x-ray examination [3,7,8]. It should be noted that osteoarthritis is rarely localized in the peripheral region of the articular surface of the head of the humerus, although the acromial clavicular and sternoclavicular joints are often susceptible to this process. In the topical diagnosis of damage to the muscles that make up the rotator cuff, the most indicative test is using resistive active movements: the patient’s arm is lowered along the body and bent at the elbow joint forward at an angle of 90° and fixed by the doctor, limiting its movements. Pain in the shoulder when the patient tries to bring the hand medially to the abdomen indicates damage to the subscapularis muscle. Pain that occurs when trying to abduct the hand to the lateral side indicates damage to the infraspinatus and teres minor muscles. Pain when trying to move the arm upward suggests a pathology of the supraspinatus muscle. Pain in the shoulder when trying to perform a supination movement with the hand indicates tendinitis of the tendon of the long head of the biceps [7]. Retractile capsulitis is difficult in diagnostic terms, as well as in treatment and prognosis. It is characterized by isolated damage to the fibrous part of the joint capsule and is accompanied by excessive tension, contraction (retraction) and a decrease in the volume of the joint cavity. The resulting severe pain, accompanied by a sharp limitation of all movements in the joint, allows us to characterize this condition as a “frozen shoulder.” A reduction in the intra-articular space, a sharp limitation in the extensibility of the capsule and smoothing of its normal inversions are established with contrast arthrography, arthroscopy, and computed tomography of the joint [7]. Ultrasound provides valuable information for diagnosing the pathology of the soft tissue structures of the shoulder with the ability to differentiate the above pathological conditions [6,9,10]. Unlike periarthritis of the shoulder joint, when the cervical spine is affected, the pain usually spreads along the entire length of the arm, including the hand, is accompanied by sensory and motor disturbances, and intensifies with active and passive movements and with percussion of the cervical spine. Damage to both shoulder joints can begin either simultaneously or delayed in time. In this case, one of the reasons for damage to the second shoulder is increased compensatory mechanical overload. The duration of periarthritis of the shoulder joint depends on the clinical variants. The disease progresses from several weeks with possible spontaneous recovery to a chronic, permanent or recurrent course over many years with a questionable prognosis [1,10,11]. Treatment of pathological conditions in the shoulder and upper shoulder girdle comes down mainly to the fight against pain. Local soft tissue damage in the shoulder girdle makes local therapy attractive at the first stage, which is pathogenetically determined and clinically effective. The effect is directly on the lesion, and the optimal therapeutic concentration of the drug is quickly achieved in the affected lesion, which reduces the need for systemically prescribed pharmacological agents and reduces the side effects of medications in general on the body [12]. Also, the use of heat or, conversely, cold in treatment does not contradict (it all depends on how the patient tolerates these procedures, what he expects from them and what previous experience he has). But the first place still remains the use of warming ointments, applications of ointments containing non-steroidal anti-inflammatory drugs (NSAIDs): creams and ointments. To obtain a clinical effect when using NSAID-containing ointments, it is necessary to use them for a sufficiently long time and observe the frequency of applications. As a rule, the doctor advises applying an amount of the drug from 3 to 7 cm 3-4 times a day to the affected area [4,12]. The disadvantage of the application method is the low amount of medicinal substance that penetrates the tissue, on average up to 5% of the total amount used. The degree of penetration of the drug depends on its lipophilicity and proper hydration of the stratum corneum of the epidermis. The barrier functions of the skin, including changes in pH gradients, make it difficult for the drug to penetrate deep into the tissues. Physiotherapeutic methods of treatment are actively used as local therapy, both independently and in combination with other therapeutic agents. Widely used physical factors reduce pain, muscle spasms, inflammatory processes, improve microcirculation and trophism, and have a beneficial effect on metabolic processes in joint tissues. Among the various methods of physiotherapeutic treatment, it is recommended to use medicinal electrophoresis, which combines the therapeutic effect of both the most used physical factor - direct electric current, and the medication administered with its help. The administration of drugs using electrophoresis is painless and is not accompanied by damage to the skin. The effect of drugs is noticeably enhanced due to their administration in ionized form. On the other hand, we must remember that not all drugs can be used for electrophoresis, since under the influence of electric current their structure and, consequently, pharmacological properties can be changed. With a clear topical diagnosis, local therapy in the form of injection of anesthetics with glucocorticoid drugs into the lesion gives a rapid positive clinical effect. With local therapy, a sufficient local therapeutic concentration of the drug is achieved, which reduces the need for systemically prescribed pharmacological agents [1,8]. Novocaine or lidocaine is currently widely used as a local anesthetic for local therapy. J. Travell (1989) recommends adding glucocorticoids to the novocaine solution when infiltrating pain points for the following reasons: the patient has symptoms of connective tissue inflammation, the development of post-injection pain and allergic reactions as a response to the administration of novocaine [3]. But, as many years of practice have shown, local therapy and physiotherapeutic methods, as a rule, are auxiliary or additional, and the main treatment consists of the use of non-steroidal anti-inflammatory drugs (NSAIDs) with the simultaneous use of physical therapy to develop movements in the affected shoulder joint. Careful monitoring of patients is important: the effect and tolerability of therapy, assessment of quality of life and the degree of impairment of motor activity [5,6]. Ibuprofen is a widely used NSAID. The main principle of its action is the inhibition of the synthesis of prostaglandins, which play an important role in the triggers of inflammation and pain transmission processes. Ibuprofen is part of the combination drug Nurofen Plus, the second component of which is codeine. Both active ingredients in Nurofen Plus are well known and have been used in clinical practice for a long time. Moreover, the same half-life of ibuprofen and codeine, which is 2–2.5 hours, is favorable for their combination, and codeine, even in minimal doses, acting on the opiate receptors of the central nervous system, enhances the effect of ibuprofen. This allows adequate effective pain relief to be achieved while reducing the dose of NSAIDs and with minimal adverse reactions. The purpose of this work was to determine the possibility of using, assessing the effectiveness and tolerability of a combination drug - Nurofen Plus (Boots Healthcare International), one tablet of which contains the active ingredients: 200 mg of ibuprofen and 10 mg of codeine phosphate. For the period 2002–2005 57 patients with PPS were examined. Preliminary studies have been previously published [13]. Patient information and clinical trial data were obtained for each patient and entered into charts. Assessment of the severity of articular syndrome, including criteria for the presence of reactive synovitis, was confirmed by ultrasound examination of joints (LOGIC-500 apparatus) [3]. A 10-day open study with an independent evaluator was conducted in 45 (29 women and 16 men) patients with PPS with moderate and mild pain. The daily dose of Nurofen Plus was 800 mg of ibuprofen and 40 mg of codeine. Unilateral lesions were diagnosed in 38 (21 on the right, 17 on the left) patients, bilateral – in 7 (all men). Most patients were aged >39 years (40%). The majority of patients suffered from chronic shoulder pain (more than 3 months) (68%), 7 of them had a recurrent course with a disease duration of more than 5 years. Among the concomitant pathologies in the patients included in the study, cardiovascular diseases were diagnosed in 9, arterial hypertension was most often noted in 10, chronic kidney disease, including urolithiasis (in 11), chronic gastritis (in 12), allergic reactions on antibiotics (in 3). Prior to the inclusion of patients in the study, as well as after its completion, the dynamics of laboratory indicators were evaluated: HB, ALT, AST, C - Reactative protein, the number of peripheral blood leukocytes, ESR, and a general urine analysis was performed. The criteria for exclusion from the study were patients with exacerbation of chronic gastritis, peptic ulcer of the stomach or duodenum, chronic colitis or Crohn's disease, as well as chronic constipation and clinically significant syndromes of blood pathology, liver and kidneys (serum creatinine level> 300 μmol/l), malignant neoplasms, pregnancy or planned pregnancy, anamnesis bronchial asthma attacks, current acute rhinitis and urticaria, or hypersensitivity to NSAIDs and acetylsalicylic acid. The effect of therapy was evaluated after 10 days (final point) according to the following clinical parameters: joint pain during movement, at rest, night pain and degree of impaired function of the affected shoulder joint according to the visual analogue scale (your in mm), as well as the degree of limitation of active and passive movements, based on the functional activity of the patient in points (0 - there is no restriction, 1– weak, 2 - moderate and 3 - pronounced restriction). After the study, separately patients and the doctor evaluated the effect of treatment: significant improvement, improvement, lack of effect and deterioration. The nature and severity of adverse reactions was recorded in the map of side effects, which was filled during planned visits to the attending physician on the 3rd and 10th days of the study. Observation of the development of adverse reactions lasted another 15 days after taking the last dose of the drug. It was planned that adverse reactions will be evaluated by patients as mild, moderate or severe, and the attending physician - as not related to the drug, possibly associated with taking the drug or associated with the drug. The drug was canceled with the development of adverse reactions, insufficient effects, deviations from the research protocol, not fulfilling the patients with the patient, the impossibility of monitoring patients or insufficiency of information about it. For all patients in 5 days (flushing period) before the intake of Nurofen Plus, previously used NSAIDs were canceled, as well as patients were included in the study a month after the intra -sub -human administration of glucocorticoids. Thus, in total, the effect of therapy in 52 affected joints was estimated. Throughout the treatment period, there was no intra -articular administration of steroids and taking other drugs with an analgesic effect. The 10 -day course of treatment 40 (89%) of 45 patients was completely completed. 2 patients stopped taking the drug after 4 and 8 days in connection with persistently pronounced hypertension against the background of constant use of captopril 10 mg, another 1 patient - after 5 days due to hospitalization for the planned operation of the prostate adenoma. In 9 patients, dizziness was observed mainly 1.5–3 hours after taking the drug by 5–6 days of treatment. In this connection, 2 (6%) patients abandoned the further administration of Nurofen Plus on the 5th and 6th day of treatment, respectively. Based on the analysis of the dynamics of the main clinical parameters (Table 1), the analgesic efficiency of Nurofen Plus has been established, which was confirmed by statistically significant differences between the data when comparing the results. The pain at rest decreased from 44.8 ± 4.0 to 25.2 ± 1.2 mm, pain during movement - from 55.4 ± 7.7 to 22.1 ± 2.8 mm, night pain - 23.8 ± 4.5 to 11.5 ± 3.07 mm and palpation pain from 38.9 ± 4.1 to 21.1 ± 1.7 mm. The function of the function of affected shoulder joints from 33.9 ± 4.8 to 17.1 ± 1.2 mm improved. The degree of restriction of active and passive movements of moderate and pronounced degree in the affected joints before the start of treatment took place in more than half of the patients, while after treatment the indicated disorders were registered only in every 6th patient (p <0.01). The effect of therapy, both in the assessment of patients and by the doctor’s assessment, was evaluated as a significant improvement and improvement of 90%, the effect was absent in 10% of cases. Evaluation of the effectiveness of Nurofen Plus was not specially studied in the treatment of PPA, and the combination of ibuprofen and codein was tested for coxarthrosis with moderate and pronounced pain syndrome. Reception with a randomized blind cross method for evaluating the effectiveness of therapy of the combination of 200 mg ibuprofen and 30 mg of codeine (1 group) led to a reliable decrease in pain than only the use of one ibuprofen at a dose of 200 mg. The authors explain a more significant effect by increasing the plasma concentration of the drug, and repeated doses of codein enhance the analgesic effect of ibuprofen [14]. The results of our studies can be conditionally extrapolate to the described above. Thus, the results of an open study using an independent appraiser to assess the effect of therapy allow us to conclude that the advisability of using the Nurofen Plus two -component drug in patients with poorly or moderate pain in the treatment of periarthritis of the shoulder joints.
References 1. Zulkarneev R.A. “Painful shoulder”, glenohumeral periarthritis and “shoulder-hand” syndrome. Kazan: Kazan University Publishing House. 1979: 310. 2. Gulyaeva E.N. Experience in the treatment of glenohumeral periarthritis in outpatient settings. Abstracts of the X Anniversary Conference of the Moscow Professional Association of Chiropractors, October 26–29, 2000. Bulletin. No. 2. M.; 2000: 69. 3. Travell J., Simons DG (Travel J., Simons D.G.) Myofascial pain. Volume 1. M.: Medicine. 1989: 115–127. 4. Nikiforov A.S., Mendel O.I. Shoulder pain syndrome: modern approaches to diagnosis and treatment. RMJ. 2006; 8:621–626. 5. Rheumatic diseases. Ed. V.A. Nasonova, N.V. Bunchuk. – M.: Medicine, 1997: 411–438. 6. Solomin M.Yu., Lomtatidze E.Sh., Potseluiko S.V. Algorithm of treatment and diagnostic measures for glenohumeral pain syndrome. Materials of the III International Conference on Rehabilitation Medicine (Rehabilitation). M: Zlatograph. 2000: 129–130. 7. Talibov F.Yu. Shoulder-scapular periarthritis: etiology, pathogenesis, clinical picture and treatment. Rheumatology. 1983; 4:42–47. 8. Khitrov N.A., Tsurko V.V. Periarthritis of the shoulder joint: clinical and diagnostic features and therapy. Doctor. 2004; 9:39–42. 9. Arthrosonography. H.Sattler, U.Harland. Berlin: Springer–Verlag, 1990.– 164 P. 10. Diagnostic ultrasound. Ed. Zubareva A.V. – 1st edition – M.: Realnoe Vremya. 1999: 176. 11. Agababova E.R., Talybov F.Yu., Mylov N.M., Shprakh M.D. Symptoms of various clinical and anatomical variants of shoulder-scapular periarthritis (periarthrosis). Rheumatology. 1983; 2:48–51. 12. Nasonova V.A. Features of the use of various forms of diclofenac sodium for diseases of the soft tissues of the shoulder girdle and pain in the lower back. Consilium medicum. 2006; 2:46–50. 13. Tsurko V.V., Agapova L.A., O.A. Obukhova, T.B. Ivanova, K.A. Lytkina. Nurofen-plus in the treatment of periarthritis of the shoulder joint. Doctor. 2004; 11:49–51. 14. Quiding H. et al. Ibuprofen plus codeine, ibuprofen and placebo in a single–and multidose cross–over comparison for coxarthrosis pain. Pain. 1992; 50: 303–307.