Frozen shoulder is a condition characterized by inflammation, scarring, and tightening of the connective tissues surrounding the shoulder joint, resulting in shoulder pain and severely decreased range of motion.
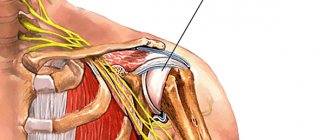
The shoulder joint is a ball joint. There is a notch in the shoulder blade (rosette), and the head of the humerus is spherical. The dense connective tissue surrounding this hinge holds the joint in place and is called the joint capsule. And when inflammation of the joint capsule occurs, then after the inflammatory process resolves, scarring of the capsule tissue occurs and its elastic properties are impaired. This process results in a condition called glenohumeral periarthritis, which typically results in severe loss of range of motion.
Periarthritis of the humeroscapula is most common in people over 40 years of age and tends to occur more often in women than men.
Causes of periarthritis
Although the exact causes are not known, the disease is believed to result from injuries to the shoulder joint or the tissues surrounding it. In these cases, the disease most likely develops due to lack of proper treatment. Quite often, this condition occurs due to insufficient rest during excessive loads or adherence to the principle “pain must be overcome.” The likelihood of this disease is also increased with prolonged immobilization (after injury or surgery). The main factors predisposing to the development of periarthritis are the following:
- history of recent trauma
- history of shoulder surgery
- inadequate treatment after shoulder injury or surgery (especially immobilization for too long)
- diabetes
- autoimmune diseases
- age over 40 years
- bad posture
Useful video
Experts from Channel One in the program “About the Most Important Thing” talk about exercises for the shoulder:
Frozen shoulder syndrome is a fairly common and unpleasant condition. With capsulitis, there is limited mobility of the shoulder joint and constant pain, which negatively affects the quality of life. If you notice the first symptoms of the disease, you should immediately contact a specialist. Timely treatment will help avoid a number of complications.
If you find an error or traces of code (for example, individual characters >, ],=...), please select a piece of text and press Ctrl+Enter.
Symptoms
Symptoms associated with the disease glenohumeral periarthritis tend to develop gradually over a period of time (often after recent injury, surgery and/or immobilization). Patients typically experience a dull ache that may intensify and become sharp with certain movements and activities. The pain is usually located deep in the shoulder, but can sometimes be felt in the shoulder, upper back and neck. Patients may also experience stiffness in the shoulder, neck, and back.
The pain associated with this condition can worsen with any movement of the shoulder and with activities that place pressure on the shoulder. These are activities such as: raising your arms up, lifting weights, pulling or pushing movements, being in a position lying on the affected side, placing your hand behind your back. Patients with glenohumeral periarthritis often experience pain at night or after waking up in the morning. As the disease progresses and moves from the painful stage to the frozen shoulder phase, the pain may decrease significantly.
In addition to pain, patients typically experience noticeable stiffness and a significant reduction in the shoulder's range of motion. As a rule, with periarthritis, all movements in the shoulder are limited, but the most reduction in volume is noticeable during rotation and elevation of the arm. This may manifest as difficulty raising your arm or placing your arm behind your back. As this condition progresses from the "frozen" phase to the "unfreeze" phase, the range of motion gradually increases, with a subsequent decrease in joint stiffness. Patients may also develop muscle atrophy in the affected arm, as a decrease in range of motion causes some of the muscles to not work at full strength and this leads to their atrophy. Although glenohumeral periarthritis usually affects only one side, some patients may have bilateral involvement.
The development of glenohumeral periarthritis can be divided into three phases, each of which can last several months:
- Pain - In this first phase of glenohumeral periarthritis, the shoulder becomes painful and most movements are painful. There may also be stiffness in the shoulder.
- “Freezing” is the second stage of this disease and is characterized by severe loss of movement in the shoulder, coinciding with scarring of the shoulder capsule. Patients usually have difficulty raising their arms or placing their arms behind their back. Pain may noticeably decrease during this phase.
- "Unfreezing" - In this final phase, the shoulder spontaneously begins to "loosen" and movement in the shoulder is gradually restored.
Symptoms of inflammation of the shoulder joint capsule
There are two main manifestations characterizing the frozen state of the joint capsule:
- reduction in range of motion, progressing to complete inability to move the affected arm;
- pain in the joint when raising and turning the arm, which over time complements pain in the neck and spine, numbness of the hand and clumsiness in the fingers, which intensifies as the pathology develops.
Depending on the causes and stage of the disease, symptoms may differ slightly. If the disease is not associated with previous injuries, the less active arm is usually affected. Discomfort and pain at night are more intense than during the day. Without timely assistance from a doctor, the patient experiences an increase in the symptoms of frozen shoulder, which will be more difficult to get rid of than at the initial stage of the inflammatory process. To determine the degree of development of the pathology, a thorough medical examination is necessary.
Diagnostics
As a rule, to make a diagnosis of glenohumeral periarthritis, an examination by a doctor and the patient performing certain functional tests are sometimes sufficient. Additional research methods such as ultrasound or MRI make it possible to visualize the altered connective tissue of the joint capsule and confirm the doctor’s preliminary diagnosis. In addition, laboratory tests are advisable to exclude possible other diseases. The most informative diagnostic method is MRI, which allows you to clearly visualize not only the joint capsule, but also morphological changes in all tissues of the joint.
First aid
Proper implementation of first aid measures for a dislocated shoulder includes immobilization (immobilization) of the joint using available means (scarf, bandage, scarf, clothing), as well as ensuring its functional rest. If there is severe swelling of the soft tissues, cold is applied to the shoulder area (a napkin moistened with cold water, an ice pack), which will reduce the inflammatory reaction, after which the shoulder will hurt less.
The next step of assistance is to transport the injured person to a trauma center or call an ambulance. If habitual shoulder popping develops, a person can straighten it himself or with the help of people around him. In the case of a primary dislocation, it is not recommended to perform a reduction on your own, as this can cause various serious complications, including damage to large vessels with severe bleeding, rupture of the capsule, and large nerve trunks.
Treatment
The goal of treating glenohumeral periarthritis is to reduce pain and maintain mobility in the shoulder. However, recovery of full shoulder function may take a long time, and symptoms may persist for several years.
Conservative treatment
Drug treatment. The most widely used drugs are NSAIDs, such as ibuprofen, voltaren, movalis, etc. For severe pain, prescription analgesics (for example, containing codeine) can also be used. Intra-articular injections of steroids can quickly relieve the inflammatory process and reduce pain during periarthritis. But frequent steroid injections are not recommended as they may cause damage to the shoulder tissue.
Transcutaneous electrical neurostimulation can significantly reduce pain.
Physiotherapy. There are many physiotherapeutic procedures that can improve blood circulation in a damaged joint capsule, reduce inflammation and reduce pain.
Exercise therapy. A carefully chosen exercise program can prevent and even relieve shoulder stiffness.
Shoulder manipulation under anesthesia allows you to increase range of motion.
Surgical treatment and periarthritis
Indicated in cases where conservative treatment is not effective. The operations are performed using arthroscopic techniques, during which excision (removal) of scar tissue and adhesions or osteophytes is performed. Given the minimally invasive nature of such surgical techniques, the patient after arthroscopic surgery is discharged on the same day.
Frozen shoulder syndrome
Shoulder pain is observed in the clinical picture of a number of not only neurological, but also somatic diseases; its prevalence reaches 26% of the general population [1]. The main causes of shoulder pain are listed in Table 1 [2]. For ease of diagnosis, they are divided into two groups: pain with acute and gradual onset. It must be emphasized that pain in the shoulder area can be a manifestation of a severe somatic disease, in particular oncological pathology (Pancoast tumor, extra- and intramedullary tumors), and in this case, early diagnosis can save the patient’s life. Therefore, shoulder pain deserves the most thorough and comprehensive study. However, most often shoulder pain occurs due to damage to the joints (shoulder, acromioclavicular and sternoclavicular) and surrounding soft tissues. It has been shown that in elderly patients, about 65% of cases of shoulder pain are caused by pathology of the rotator cuff, 11% by soreness of the pericapsular muscles, 10% by pathology of the acromioclavicular joint, and 3% by arthritis of the shoulder joint. In 5% of cases, the pain is radiating from the cervical spine [3]. In women, shoulder pain is 1.5 times more common than in men [4].
Frozen shoulder syndrome (FS) is a clinical phenomenon characterized by pain and limited mobility in the shoulder joint. Its cause can be any of the pathologies listed in Table 2 (secondary syndrome).
There is also a primary PV syndrome, the etiology of which is not fully understood [5]. It is more common at the age of 40–70 years, and the prevalence of this pathology is about 2–5% [6]. It is believed that it is based on inflammatory mechanisms in the shoulder joint, accompanied by inflation of the synovial membrane, which causes pain, limitation of movement and a feeling of muscle weakness in the absence of significant structural defects in the anatomy of the joint (Fig. 1).
Risk factors for the occurrence of PP include [1]: – old age; – injuries or surgical interventions in the shoulder joint; - diabetes; – cardiovascular diseases; – cerebrovascular diseases; – endocrine pathology. Most often, PP syndrome is caused by the development of degenerative-inflammatory changes in the joint-ligamentous apparatus of the shoulder. ZP usually occurs in the late stages of glenohumeral periarthropathy. On an x-ray, this looks like arthrosis and calcium deposits in the lateral parts of the joint capsule. Despite the fact that periarthropathy is a chronic, long-term developing process, PV can develop suddenly, acutely and without visible provoking factors. Clinically, PP manifests itself as shoulder pain radiating to the arm and limited range of motion in the shoulder joint. The limitation of movements is more pronounced during flexion, extension and external rotation, less so during adduction and internal rotation. Movements in the neck are completely preserved, but may slightly increase the pain. When the arm is abducted, the pain increases sharply, the muscles of the shoulder girdle tense. In this state, it is very difficult to examine the motor capabilities of the joint. Due to contracture, shoulder abduction is limited: the shoulder is “chained” to the scapula, and only slight abduction is possible. Movement in the sagittal plane (back and forth) is relatively free. No reflex or sensory disturbances were detected in the shoulder girdle area. Pain in glenohumeral periarthropathy is mainly caused by rotator cuff pathology, adhesive capsulitis and myofascial pain syndrome [7]. Rotator cuff pathology
is the most common cause of shoulder pain.
Men over 40 years of age are most often affected, and the dominant hand is usually affected. There are 3 forms of rotator cuff lesions: – degenerative and compressive tendinitis of the supraspinatus tendon; – calcific subacromial tendinitis/bursitis; – complete or partial rupture of the supraspinatus tendon. Rotator cuff lesions are characterized by local pain in the deltoid muscle, under the acromion and near the greater tubercle of the humerus. There may be a slight irradiation of pain, intensification with movement, limitation of active shoulder abduction and external rotation while maintaining passive movements. Palpation of the greater tubercle is painful, crepitus and swelling are detected. For diagnosis, a Nier test is performed: injection of a local anesthetic solution into the subacromial space relieves pain and restores range of motion [6]. Adhesive capsulitis
is a chronic fibrous inflammation of the shoulder joint capsule.
It is this variant of ZP that is considered idiopathic, since the reasons for the occurrence of this process are unclear. It occurs in women over 45 years of age and does not depend on the intensity of physical activity. The lesion is usually unilateral. The pain is constant, aching, localized in the shoulder joint and does not radiate. Characterized by increased pain at rest and at night and a slight weakening with movement. In the morning there is stiffness in the shoulder joint. There is swelling around the joint. The affected shoulder is raised, the muscles of the shoulder girdle are shortened, slightly atrophic, and increased fatigue is characteristic. The range of active and passive movements in the joint is uniformly limited in all directions and does not increase when bending forward. Rotation of the scapula is characteristic when the shoulder is abducted more than 60°. When performing the Nier test, pain decreases, but limited mobility in the joint remains [6]. Myofascial syndrome
is another common cause of PV. The main symptom of myofascial pain syndrome is the presence of acute intense pain that occurs when pressing on the trigger point (TP). Myofascial TP can be located in muscles, fascia or tendons, and they are the cause of this type of pain. In ZP, TTs are most often detected in the subscapularis muscle, then in the pectoralis major and minor muscles, and less often in other areas. On palpation, the TT is felt as a compaction or cord, pressure on which provokes sharp local pain (sometimes with the so-called “jumping symptom,” i.e., shuddering) and radiating (referred) pain of various localizations. Each TT has its own zones of referred pain, which is usually dull, aching, deep and may be accompanied by numbness (paresthesia). Thus, when pressing on the TT, the pain syndrome characteristic of a given patient is reproduced [8].
Treatment of PV syndrome
Treatment is complex and necessarily includes both medicinal and non-medicinal methods of influence [9]. The main therapies are listed in Table 3.
Non-drug methods of influence
are extremely diverse, but their effectiveness from the point of view of evidence-based medicine is quite difficult to assess.
A number of studies have reliably shown the effectiveness of external shock wave effects, laser treatment and physiotherapy. Chiropractic techniques using stretching, post-isometric relaxation, and acupuncture are widely used [10–12]. Arthroscopic subacromial decompression has proven effectiveness among surgical techniques; there are also newer techniques, the experience of which is not yet sufficient to make a confident conclusion about their effectiveness (Table 3). Drug treatment
during an exacerbation is primarily aimed at relieving pain, muscle spasm and swelling; for this purpose, combination therapy is prescribed with the use of analgesics, glucocorticoids, and muscle relaxants [11, 12].
Often, PV syndrome becomes chronic and lasts for years; in this case, external agents, drugs containing biologically active (chondromodulatory, chondroprotective) components of cartilage tissue (chondroitin, glucosamine) and antihomotoxic drugs play a significant role in therapy. To eliminate pain and inflammation, non-steroidal anti-inflammatory drugs (NSAIDs) are widely used, which act quickly and quite effectively. Oral NSAIDs have proven effectiveness in cases of acute tendinitis and subacromial bursitis. However, in some cases, even short-term use of NSAIDs in small doses can cause serious adverse reactions, especially from the gastrointestinal tract (dyspeptic disorders, erosions and ulcers of the stomach and duodenum, bleeding and perforation). Therefore, it is recommended to use NSAIDs in short courses, giving preference to drugs with selective action. It is often advisable to begin therapy with intramuscular injections, switching to tablet forms of NSAIDs. Muscle relaxants
are used to relax spasmodic, painful muscles.
The use of muscle relaxants in complex therapy of PV syndrome can reduce pain and reduce the dosage of NSAIDs. The traditional drug for these purposes is Tolperisone. Hot compresses also have a muscle relaxant effect. To relieve muscle tension, a combined antihomotoxic drug, Spascuprel, containing 11 natural ingredients, is also used. Local injections
are widely used, and nerve blocks (nervus supraskapularis) are considered the most effective in terms of pain management.
A meta-analysis of studies of ZP therapy did not show clear preferences for any surgical method or local anesthesia [13]. Intra-articular injections of corticosteroids in patients with PV may reduce pain in the short term, but their long-term effectiveness compared with local anesthetics remains unclear. New techniques are being tested, such as injections of autologous blood and platelet-rich plasma, the effectiveness of which has not yet been sufficiently confirmed [1]. External agents
(ointments, gels, creams, compresses and patches) are one of the most common methods of treating chronic pain syndromes of the musculoskeletal system. The undoubted advantage of local exposure is the absence of systemic side effects, which allows you to use this or that ointment or gel for an unlimited time. The most commonly used drugs for external use are presented in Table 4.
Slow-acting drugs, or SYSADOA
(Symptomatic Slow Acting Drugs for Osteoarthritis) consist of biologically active (chondromodulating, chondroprotective) components of cartilage tissue necessary for the construction and renewal of articular cartilage.
These include: – cartilage matrix precursors (glucosamine, chondroitin and hyaluronic acid); – cytokine modulators (diacerein and metalloprotease inhibitors). The most studied chondroprotective substances to date are chondroitin and glucosamine. Chondroitin
is produced by the cartilage tissue of the joints and is part of the joint fluid.
It promotes the deposition of calcium in bones, strengthens connective tissue structures: cartilage, tendons, ligaments, skin, and promotes cartilage regeneration. By retaining water in the thickness of the cartilage, it increases the strength of the connective tissue. It is chondroitin that inhibits specific enzymes that destroy connective tissue. Glucosamine is an essential component of glycosaminoglycans and joint fluid, stimulates synthesis in chondrocytes and reduces catabolism; its deficiency impairs the quality of synovial fluid and can cause crunching in the joints [14]. With age, as a result of neurodegenerative processes, the natural synthesis of these substances decreases, and with the help of SYSADOA it is possible to replenish them. A sufficient evidence base has been accumulated indicating the effectiveness and safety of SYSADOA, the need for their use in terms of long-term treatment and prevention of the development of osteoarthritis and other diseases of the musculoskeletal system [15, 16]. They are able to influence the metabolism of bone and cartilage tissue and stimulate its regeneration, have a moderate analgesic and anti-inflammatory effect and are free of the side effects characteristic of NSAIDs. Outside of exacerbation, monotherapy with SYSADOA is recommended. In case of exacerbation of the process and severe pain, it is recommended to combine SYSADOA with NSAIDs, since the analgesic effect of the latter develops much faster. Combined use allows you to reduce the dose of NSAIDs and thereby prevent a number of unwanted side effects [17]. Antihomotoxic drugs
are becoming increasingly popular for the treatment of musculoskeletal diseases.
This group of drugs includes such widely used drugs as Traumeel S, Tsel T, Spascuprel, Lymphomyosot, Discus compositum, etc. Antihomotoxic therapy is aimed at strengthening and supporting the patient’s internal sanogenetic mechanisms by restoring the body’s autoregulatory systems. The effectiveness of this group of drugs is based on their effect on various parts of chronic inflammatory processes and the body as a whole. Unlike analgesics, NSAIDs, and intra-articular corticosteroids, antihomotoxic therapy is safe and does not have significant side effects. Permanent suppression of the inflammatory response when using NSAIDs disrupts the mechanisms of autoregulation (endogenous resolution of inflammation) and is a short-term and symptomatic remedy. In turn, dysregulation of the inflammatory response and microenvironment is considered the main mechanism maintaining chronic maladaptive inflammation [18, 19]. One of the most famous representatives of antihomotoxic drugs is Traumeel S. The drug includes a fairly large list of components (12 plant and 2 mineral), which provides a wide spectrum of action: anti-inflammatory, analgesic, anti-exudative, hemostatic, regenerating and immunomodulatory) [20–24 ]. It is important to note that Traumeel S, unlike NSAIDs, has a promoting effect on recovery processes, maintaining a certain level of inflammation and leaving the body the opportunity for autoregulation. Indications for the use of the drug Traumeel S are degenerative and inflammatory processes in the musculoskeletal system (in particular, glenohumeral periarthritis) and post-traumatic conditions. The advantages of Traumeel S over NSAIDs are its good tolerability and safety of long-term use [21], which is especially important for patients with chronic diseases of the musculoskeletal system. The use of Traumeel S with NSAIDs or glucocorticosteroid drugs makes it possible to reduce their dosage while increasing the effectiveness of complex treatment. If necessary, the drug can provide a safe replacement for NSAIDs. Traumeel S has a variety of release forms (tablets, drops, gel, injection solution) for both local, oral and parenteral administration. The injection solution can be administered intramuscularly, subcutaneously, intra-articularly, periarticularly, intradermally, segmentally (using the biopuncture method) and in places for acupuncture treatment. When using the biopuncture method, a good effect is achieved with a combination of the drugs Traumeel S and Lymphomyosot. Lymphomyosot is used for lymphatic drainage and matrix detoxification, and Traumeel S is used to regulate the inflammatory response [22]. To relieve pain and muscle spasms, a combination of the drugs Lymphomyosot and Spascuprel is used. Spascuprel is an antihomotoxic drug containing 11 natural ingredients. Indications for its use are spasms of smooth and striated muscles. Goal T
is another antihomotoxic drug (contains 14 natural components), which has been used for many years to treat chronic diseases of the musculoskeletal system, such as glenohumeral periarthritis, arthrosis, and spondyloarthrosis. The drug provides a comprehensive anti-inflammatory effect, nourishes, remodels and regenerates articular cartilage, preventing its vascularization. In the treatment of chronic inflammation, this drug plays a special role: many of its components, such as Rhus tox, contain flavonoids known for their antioxidant properties [23]. Rhus tox and Arnica influence the release of IL-6 (regulator of chronic inflammation and angiogenesis) by macrophages; The alkaloid sanguinarine, which is part of the drug in the form of an extract of Sanguinaria canadensis, has the ability to inhibit vascular endothelial growth factor [24]. A number of studies have shown that the drug Cel T is not inferior in effectiveness to COX-1 and COX-2 inhibitors in the treatment of mild and moderate osteoarthritis and arthrosis, while having a much better safety profile and tolerability [25]. The variety of drug release forms (tablets, ointments, ampoules) ensures ease of use. Due to the different types of effects on the mechanisms of acute and chronic inflammation, it is possible to recommend the combined use of the drugs Traumeel S and Target T: Traumeel S - at the onset of the disease and during its exacerbations, Target T - for long-term treatment. Both drugs have a good tolerability profile.
Prognosis and prevention
In most cases, glenohumeral periarthritis heals within a few months. In severe cases, symptoms may last for 18 months or longer. Typically, the painful stage of glenohumeral periarthritis lasts 2 to 6 months. The frozen phase is approximately 4 -12 months, while the defrosting phase can last another 4 - 18 months. In some cases, patients may experience some restrictions in movement after completing all three stages. However, in most cases the prognosis for glenohumeral periarthritis is good. Prevention of this disease is timely consultation with a doctor if shoulder pain occurs (especially after an injury) and systematic physical activity, which minimizes the risk of such conditions and helps maintain mobility and flexibility in the shoulder joint.