Why does the disease occur?
Tendonitis of the knee joint is a problem for physically active people, most often teenagers and professional athletes. Numerous jumps on hard surfaces during volleyball, basketball, tennis, football and athletics provoke the disease.
Contribute to the development of pathology:
- incorrect training regimen;
- uncomfortable shoes;
- knee injuries;
- long-term therapy with antibacterial drugs;
- foot deformities (flat feet, hallux valgus, etc.);
- posture disorders and spinal diseases;
- overweight;
- lack of muscle elasticity;
- wide hips in women.
Secondary tendonitis is a complication of rheumatic, infectious, parasitic diseases and metabolic pathologies.
Pathogenesis
As a rule, inflammation occurs at the site of attachment of the patellar ligament to the bone. With excessive loads, microdamages with local hemorrhages occur in the tendon tissue, which cause aseptic inflammation. The outcome of the inflammatory process is necrosis of collagen fibers and replacement with scar tissue.
A tendon with many scars is fragile, inelastic, and therefore vulnerable and easily injured again. New microbruises, aseptic inflammatory process and scar, long-term sluggish course, leads to degeneration and thinning of the tendon-ligamentous structures of the joint.
Forecasts, prevention
With timely treatment and strict adherence to the doctor’s recommendations, the prognosis for the patient is favorable - the inflammatory process is stopped, and relapses, as a rule, occur extremely rarely.
Preventive actions:
- wear comfortable shoes;
- Do some physical exercise throughout the day;
- avoid putting excessive pressure on the knee joints;
- Carry out intensive training under the supervision of a trainer;
- Strengthen your immune system and treat infectious diseases in a timely manner.
You can find out which doctor specializes in hip tendinitis on our website Dobrobut.com.
Related services: Orthopedics and traumatology Arthroscopy
Clinic
Clinical manifestations increase gradually and progress slowly. First, pain on the front surface of the knee occurs at peak loads. Further, dull, periodically paroxysmal pain bothers you during normal exercise, and quickly disappears after stopping training. Gradually, pain and discomfort progress, not disappearing after 4-8 hours of rest. As a result, a tear or rupture occurs in the pathologically altered tendon.
A characteristic clinical symptom of tendinitis is pain when palpating the tendon, when pressing on the tibial tuberosity, or patella. Sometimes local swelling and hyperemia of the adjacent skin, limited range of motion, and creaking and crunching when flexing and extending are characteristic.
Important! Untreated tendonitis reduces resistance to physical activity, interferes with training, and can put an end to a sports career.
Diagnostics
The doctor makes a diagnosis based on a history of sports or other injuries and a characteristic clinical picture. Additional examination methods (ultrasound, CT and MRI of the knee joint) are usually not required.
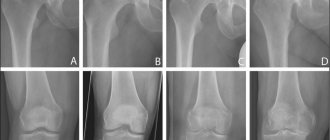
An x-ray of the knee sometimes shows slight thickening of the soft tissue. With ossifying tendonitis, there are foci of calcification.
Reference! CT, MRI and ultrasound are indicative of advanced stages of the disease. Ultrasound of the knee joint reveals a violation of the tendon structure. MRI and CT scans reveal ligament damage.
Laboratory tests are relevant for secondary symptomatic tendonitis. Rheumatoid diseases are indicated by anticiruline antibodies and rheumatoid factor, accelerated ESR, and metabolic pathologies are indicated by increased levels of creatinine and uric acid.
Most often, tendinitis is differentiated from injuries to the bone structures of the knee joint and rheumatoid diseases. The decisive method in this situation is the x-ray diagnostic method.
Treatment
Treatment of knee tendonitis is usually conservative outpatient. Surgical interventions are indicated for ineffective conservative therapy and tendon ruptures.
Treatment methods include:
- Protective mode. Stop training, recommend rest, and in some situations immobilize with plaster or plastic splints.
- Drug therapy with NSAIDs. Nonsteroidal anti-inflammatory drugs (naproxen, ibuprofen) are prescribed to relieve swelling, inflammation and relieve pain. The duration of administration is limited due to side effects from the gastrointestinal tract.
- In case of severe swelling, intense pain, widespread fibrosis, radiotherapy, blockade with glucocorticosteroids and shock wave therapy are prescribed. Hormonal drugs are administered in short courses with an interval of at least 6 months. Such regimens are recommended to avoid serious side effects (including progression of tendon degeneration).
- Physiotherapy. After acute manifestations subside, therapeutic exercises, massage, electrophoresis with novocaine, iontophoresis, UHF and magnetic therapy are prescribed.
- "GIAL-IN" and "GIAL-IN PROLONG" are medical biological products for periarticular or subcutaneous administration. A metabolite of the drug, hyaluronic acid, is part of the connective tissue of all living organisms. Penetrating into the intercellular spaces, the biological product stimulates metabolic and regenerative processes in ligaments, cartilage, joint capsules and synovial membranes of muscles.
Reference! "GIAL-IN" has no side effects and no restrictions on the duration of use. Indicated for tendonitis, degenerative-dystrophic changes in tendons, ligaments, cartilage and soft tissues.
During rehabilitation, the joint is loaded gradually. When the disease is in remission, it is recommended to regularly unload the damaged ligament using special tapes (stape) or fix the joint with an orthosis.
Good results are ensured by targeted improvement of the technique and height of jumps, since tendinitis occurs more often in athletes who practice hard landings, high jumps or landings with a deep squat.
Stages of development of knee tendinitis
The lack of ability of the tendon to absorb increased loads provokes its damage. The disease is characterized by 4 stages, depending on the severity:
- Reactive tendonitis. Tissues have a normal ability to adapt to injury. Pain syndrome occurs exclusively after exercise, while the functions of the knee joint are not impaired.
- Tendon dysfunction. In this case, degenerative processes prevail over restorative ones. Discomfort is present both during the period of exercise and after it. The patient is able to lead an active lifestyle. If further damage to the ligament is prevented, experts give good prognoses.
- Degenerative tendinitis. It is characterized by the presence of pain during and after exercise, and the death of damaged cells. The amount of movement in the joint decreases. Without treatment, it becomes impossible to restore the function of the affected knee and return to sports activities.
- Tendon rupture. Acute pain appears in the area of the joint. It is characterized by complete loss of function of the knee joint and loss of its motor activity. If acute knee tendinitis occurs, treatment can bring the desired result only after surgery.
Surgery
Surgical interventions are indicated for tendon tears, ruptures, or ineffective conservative treatment for 1.5-3 months. The operation is performed as planned in an orthopedic or trauma hospital. The skin over the pathological area is dissected, the ligamentous canal is opened, and necrotic tissue is removed.
In some situations, to stimulate reparative processes, the lower part of the patella is scraped out or multiple incisions are applied through traditional or minimally invasive endoscopic access.
For significant tears and ruptures, surgical reconstruction of the patellar ligament is indicated.
After the operation, antibacterial drugs, painkillers, physiotherapy and massage are prescribed. They are allowed to train after rehabilitation, recovery is possible within 2-3 months.
Complex exercise therapy for tendonitis III-IV degrees
The lesson is carried out after a 5-8 minute joint warm-up. The complex mainly consists of the following exercises:
- to strengthen the abductor muscle groups of the affected leg;
- to stretch and maintain tone of the Achilles tendon, calf muscles and vast oblique muscle of the thigh;
- to strengthen the quadriceps.
Here is an example of alternating these exercises. For some exercises, the dosage - the number of repetitions of the movement in a cycle - is not given. It is selected individually, taking into account individual preparedness. The presented exercise cycle is repeated 2-3 times during the lesson.
For the second and third repetition, so as not to get bored, you can choose exercises that are similar in their effects to those presented, but always in the order indicated in the table.
| Photo and title | Explanation |
|
Repeat the cycle 3-4 times. |
| To perform this exercise you need a small diameter rubber loop.
Repeat the cycle 4-5 times. |
| This exercise should be done 5-6 times, no more. To facilitate movement, when lying down, place your palm as close to the hip joints as possible. In a bent position, fully straighten your knees and place your heels on the floor. |
| Take position 1. Do not bend your knees too much. Let it sit for 2-2.5 minutes. After this, take position 2, but unlike the photo, also do not bend your knees too much and try to spread your feet as wide as possible. In this position, alternately lift your heels off the floor, but do not lift them too high. |
| Repeat the stretch on both legs 6 times (alternating leg positions). You can watch the video below this table to see how to do it correctly. |
| Between a group exercise cycle, lie with your legs elevated for 3-5 minutes, and at the end of the session for 10-20. Legs should be straight, the back of the thighs and calves touching the wall. While lying down, you can do light shaking and slight vibrations. |
In the future, when the restoration of the ligament is successful, the group of exercises presented below is included in the rehabilitation complex.