Supraspinatus tendinitis - treatment
The term tendonitis defines the inflammatory process that develops in the ligaments and tendons of various structures of the human musculoskeletal system.
Inflammation of the supraspinatus tendon, which is part of the shoulder cuff, is a fairly common phenomenon that develops under the influence of various provoking factors. If a medical specialist has diagnosed tendinitis of the supraspinatus muscle of the shoulder joint, treatment is selected individually, depending on the etiology (origin) and severity of the disease.
Possibilities of ultrasound in monitoring conservative treatment of shoulder tendinitis
Ultrasound machine HM70A
Expert class at an affordable price.
Monocrystal sensors, full-screen display mode, elastography, 3D/4D in a laptop case. Flexible transformation into a stationary scanner with a cart.
Introduction
Ultrasound diagnosis of pathology of soft tissues and the musculoskeletal system is gradually becoming a routine examination in clinical practice. Ultrasound is a reliable, non-invasive and inexpensive method of examination compared to arthroscopy, magnetic resonance and computed tomography. This method allows you to examine the tendons of muscles, nerves and joints in several projections during clinical motor tests [2, 3, 6, 8].
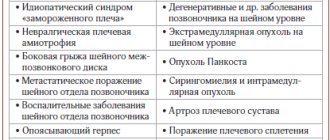
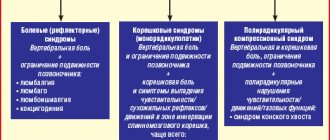
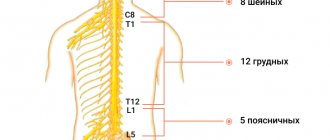
In clinical practice, quite often there are patients with pain syndrome and complaints of limitation and/or impossibility of movements in the shoulder joint. This can be caused by: pathology of the shoulder joint itself, damage to the tendons of the muscles surrounding the joint; pathology in the acromioclavicular joint; diffuse damage to the joint capsule; damage to peripheral nerves; complex involvement of structures located under the acromion; changes in the cervical and thoracic spine.
Tendon pathology is one of the most common indications for ultrasound of the musculoskeletal system [4, 7]. In this case, it is possible to diagnose inflammatory changes in the tendons (acute tendonitis or tenosynovitis and chronic tendinitis), tendinopathies (degenerative changes, calcific tendonitis), damage (partial and complete ruptures) of the tendons. Tendon changes are associated with an increase in the glycoprotein matrix, with the proliferation of tenocytes and fibroblasts with the formation of disorganized collagen fibers. These processes lead to changes in the characteristics described by ultrasound - thickness, structure, echogenicity and vascularization of the tendons.
In our work, we tried to monitor the treatment of shoulder tendinitis using ultrasound.
Materials and methods
We examined 65 patients (age from 31 to 55 years, average age - 42.5±6.2 years) with complaints of pain in one shoulder joint and restrictions of movement. The average duration of pain and limitation of movement was 3.2±1.8 months (from 1.5 to 9.2 months).
According to the anamnesis, clinical examination, and functional movement tests, the possibility of traumatic injury was excluded. All patients underwent ultrasound using devices equipped with color and power Doppler mapping modes, three-dimensional angiography before, after 2 and 4 months of treatment. The tendons (thickness, structure and echogenicity) of the rotator cuff of the affected shoulder joint were assessed in gray scale mode and these characteristics were compared with the contralateral asymptomatic shoulder joint. The tendons assessed included: the supraspinatus tendon, the long head of the biceps, the infraspinatus tendon, and the subscapularis tendon (Fig. 1). In B-mode, tendon thickness was measured (shown by an arrow) in the longitudinal projection (Long Axis), structure and echogenicity were assessed in two projections: longitudinal and transverse (Short Axis). The presence of fluid in the bursa of the shoulder joint was determined: the approximate volume in the bursa of the long head of the biceps - using 2 projections - Long Axis and Short Axis, the thickness of the fluid - in the subacromio-subdeltoid and in the subscapular bursa - in the Long Axis projection. Ultrasound angiography in the mode of energy mapping and three-dimensional reconstruction assessed the degree of vascularization along the tendons. Ultrasound data were compared with data from clinical examination of patients.
Rice. 1.
Assessment of tendons of various muscles in B-mode, Long Axis.
A)
Supraspinatus muscle. The structure is heterogeneous, the echogenicity of the tendon is normal. The subaromyo-subdeltoid bursa is not increased in size (asterisk).
b)
Long head of biceps. The structure is homogeneous, the echogenicity of the tendon is normal. Fluid along the tendon is not detected.
V)
Infraspinatus muscle. The structure is homogeneous, the echogenicity of the tendon is normal.
G)
Subscapularis muscle. The structure is homogeneous, the echogenicity of the tendon is normal. The bag has not been increased in size (asterisk).
d)
Measuring the liquid in the bag.
A set of techniques was used to treat patients: laser therapy, hirudotherapy, manual therapy using acupuncture and massage, automobilization and individual therapeutic exercises. In case of severe pain symptoms, treatment began with the introduction of non-steroidal anti-inflammatory drugs into the joint cavity. The basic method of treatment for bursitis was laser therapy, and for tendonitis - hirudotherapy. Subsequently, treatment was supplemented with another method of conservative treatment, the choice of which depended on clinical symptoms.
results
According to ultrasound, tendonitis of the supraspinatus muscle was detected in 52 (80%) patients, in 74% of cases - a combination of tendonitis of the supraspinatus muscle and tendinitis of the long head of the biceps. In gray scale mode, the supraspinatus tendon was thickened in all patients. The echogenicity of the tendon was reduced in all patients (Fig. 2). The tendon structure was inhomogeneous in all cases, without clear signs of damage (Table 1). When using ultrasound angiography, hypervascularization along the supraspinatus tendon was detected in only 15 (28.9%) patients (Fig. 3); in most patients the tendon remained hypovascular.
Rice. 2.
Supraspinatus tendon in B-mode, Long Axis.
A)
Before treatment. The tendon is thickened (up to 0.8 cm), has a moderately heterogeneous structure, and reduced echogenicity.
b)
After 2 months of treatment. There is a decrease in the thickness of the tendon (up to 0.6 cm), the structure is the same, the echogenicity is moderately increased.
V)
After 4 months of treatment. The tendon is not thickened (up to 0.47 cm), its structure is somewhat heterogeneous, and its echogenicity is normal.
Table 1
. Characteristics of the supraspinatus tendon, quantity (%).
| Characteristic | Average tendon thickness (range), cm | ||
| before treatment | after treatment | ||
| 2 months | 4 months | ||
| 0,75 (0,57-0,82) | 0,67 (0,55-0,78) | 0,58 (0,44-0,64) | |
| B-mode | |||
| Structure: | |||
| homogeneous | 0 (0) | 35 (67,3) | 45 (86,5) |
| inhomogeneous | 52 (100) | 17 (32,7) | 7 (13,5) |
| Echogenicity: | |||
| regular | 3 (5,8) | 39 (75) | 46 (88,5) |
| reduced | 49 (94,2) | 13 (25) | 6 (11,5) |
| Ultrasound angiography | |||
| Degree of vascularization: | |||
| regular | 37 (71,1) | 45 (86,5) | 49 (94,2) |
| increased | 15 (28,9) | 7 (13,5) | 3 (5,8) |
Rice. 3.
The supraspinatus tendon in various modes and projections.
A)
B-mode, before treatment, Short Axis. The tendon is thickened, has a moderately heterogeneous structure, and reduced echogenicity.
b)
Energy mapping and 3D reconstruction respectively, before treatment, Short Axis. Along the course of the tendon, closer to the place of attachment to the greater tubercle, hypervascularization is determined.
V)
Energy mapping and 3D reconstruction respectively, before treatment, Short Axis. Along the course of the tendon, closer to the place of attachment to the greater tubercle, hypervascularization is determined.
G)
B-mode, after 4 months of treatment, Short Axis. Reduced tendon thickness, increased echogenicity. The tendon structure is more homogeneous.
After 2 months of treatment, positive dynamics were noted: a decrease in tendon thickness, an increase in echogenicity in 75% of cases and a change in the structure of the tendon in 67% of cases, a decrease in the degree of vascularization.
Positive dynamics after 4 months of treatment were observed in 46 patients. At the same time, the average thickness of the tendon decreased, and the echogenicity of the tendon increased. The tendon structure remained heterogeneous in 13.5% of cases. The absence of positive dynamics was noted in 6 patients: according to the gray scale, in all patients the decrease in tendon echogenicity remained; Ultrasound angiography showed moderate enrichment of the vascular pattern in 3 patients.
When assessing the long head of biceps tendon, tendinitis was identified in all 65 patients (Fig. 4). Before treatment, the average thickness of the tendon was 0.38 cm, the echogenicity of the tendons was reduced in most cases, and the structure was heterogeneous (Table 2). According to ultrasound angiography, hypervascularization was detected in 15 (31.9%) patients. During treatment, positive dynamics were observed in the form of a decrease in tendon thickness, normalization of the tendon structure (in 35.4% of cases - after 2 months and in 83.1% - after 4 months) and an increase in the echogenicity of the tendon (in 56.9% - after 2 months and in 91% - after 4 months).
Rice. 4.
The tendon of the long head of the biceps in various modes and projections.
A)
B-mode, before treatment, Long Axis. The tendon is moderately thickened, has a somewhat heterogeneous structure, and reduced echogenicity. Along the tendon there is a small amount of fluid.
b)
B-mode, after treatment for 2 and 4 months, respectively. There is a decrease in tendon thickness and increased echogenicity. The structure of the tendon after 4 months of treatment is homogeneous. Fluid along the tendon is not visualized.
V)
B-mode, after treatment for 2 and 4 months, respectively. There is a decrease in tendon thickness and increased echogenicity. The structure of the tendon after 4 months of treatment is homogeneous. Fluid along the tendon is not visualized.
G)
Energy mapping and 3D reconstruction respectively, lo treatment, Long Axis. Along the course of the tendon, pronounced hypervascularization is determined.
d)
Energy mapping and 3D reconstruction respectively, lo treatment, Long Axis. Along the course of the tendon, pronounced hypervascularization is determined.
table 2
. Characteristics of the tendon of the long head of the biceps, quantity (%).
| Characteristic | Average tendon thickness (range), cm | ||
| before treatment | after treatment | ||
| 2 months | 4 months | ||
| 0,38 (0,43-0,51) | 0,33 (0,30-0,45) | 0,28 (0,22-0,36) | |
| B-mode | |||
| Structure: | |||
| homogeneous | 5 (7,7) | 23 (35,4) | 54 (83,1) |
| inhomogeneous | 60 (92,3) | 42 (64,6) | 11 (16,9) |
| Echogenicity: | |||
| regular | 8 (12,3) | 37 (56,9) | 59 (91) |
| reduced | 57 (87,7) | 28 (43,1) | 6 (9) |
| Ultrasound angiography | |||
| Degree of vascularization: | |||
| regular | 27 (41,5) | 37 (56,9) | 59 (91) |
| increased | 38 (58,5) | 28 (43,1) | 6 (9) |
During treatment, the degree of vascularization in patients decreased. In cases where there was no positive effect, in 9% of cases the tendon of the long head of the biceps remained hypoechoic and hypervascular (see Table 2).
Ultrasound of the infraspinatus tendon revealed tendonitis in only 16 (24%) patients. The average tendon thickness before treatment was 0.61 cm (range 0.52-0.75); during treatment after 2 and 4 months, it was 0.54 and 0.48 cm, respectively (Fig. 5). Just as with tendinitis of the supraspinatus muscle, the echogenicity of the tendon of the infraspinatus muscle with tendinitis was reduced in most cases, the structure was heterogeneous. During treatment, there was an increase in echogenicity and a change in the structure of the infraspinatus tendon (Table 3).
Rice. 5.
Infraspinatus tendon in B-mode, Long Axis.
A)
Before treatment. The tendon is thickened, has a moderately heterogeneous structure, and reduced echogenicity.
b)
After 4 months of treatment. Decreased tendon thickness, moderate increase in echogenicity. The structure of the tendon is the same.
Table 3
. Characteristics of the infraspinatus tendon, quantity (%).
| Characteristic | Average tendon thickness (range), cm | ||
| before treatment | after treatment | ||
| 2 months | 4 months | ||
| 0,61 (0,52-0,75) | 0,54 (0,45-0,60) | 0,48 (0,40-0,52) | |
| B-mode | |||
| Structure: | |||
| homogeneous | 0 (0) | 9 (56,2) | 13 (81,3) |
| inhomogeneous | 16 (100) | 7 (43,8) | 3 (18,7) |
| Echogenicity: | |||
| regular | 1 (6,3) | 8 (50) | 16 (100) |
| reduced | 15 (93,7) | 8 (50) | 0 (0) |
| Ultrasound angiography | |||
| Degree of vascularization: | |||
| regular | 12 (75) | 14 (87,5) | 16 (100) |
| increased | 4 (25) | 2 (12,5) | 0 (0) |
Ultrasound angiography revealed an increase in the degree of vascularization before treatment in only 4 patients; during treatment, the degree of vascularization decreased.
Subscapularis tendinitis (Fig. 6) was detected in 47 (72%) patients. Moreover, before treatment, the tendon was thickened on average to 0.7 cm, in all patients the echogenicity was reduced, the structure was heterogeneous. Hypervascularization before treatment was detected in 10 patients. A decrease in the average thickness to 0.64 cm after 2 months and to 0.52 cm after 4 months, as well as an increase in echogenicity and a change in structure were regarded as positive dynamics during treatment (Table 4).
Rice. 6.
Subscapularis tendon in B-mode, Long Axis.
A)
Before treatment. The tendon is thickened, has a moderately heterogeneous structure, and moderately reduced echogenicity. Fluid in the subscapular bursa is not detected.
b)
After 4 months of treatment. Decreased tendon thickness, moderate increase in echogenicity. The structure of the tendon is the same.
Table 4
. Characteristics of the subscapularis tendon, quantity (%).
| Characteristic | Average tendon thickness (range), cm | ||
| before treatment | after treatment | ||
| 2 months | 4 months | ||
| 0,70 (0,65-0,73) | 0,64 (0,59-0,68) | 0,52 (0,47-0,56) | |
| B-mode | |||
| Structure: | |||
| homogeneous | 0 (0) | 27 (57,4) | 40 (85,1) |
| inhomogeneous | 47 (100) | 20 (42,6) | 7 (14,9) |
| Echogenicity: | |||
| regular | 2 (4,3) | 24 (51,1) | 3 (91,5) |
| reduced | 45 (95,7) | 23 (48,9) | 4 (8,5) |
| Ultrasound angiography | |||
| Degree of vascularization: | |||
| regular | 36 (76,6) | 40 (85,1) | 46 (97,9) |
| increased | 11 (23,3) | 7 (14,9) | 1 (2,1) |
The absence of positive dynamics during treatment was noted in 4 patients, while the echogenicity of the tendon did not change significantly, hypervascularization remained in 1 patient.
Ultrasound revealed fluid in the joint capsules in most cases (Table 5).
Table 5
. Characteristics of shoulder joint bursae during B-mode ultrasound, number (%).
| Characteristic | before treatment | after treatment | |
| 2 months | 4 months | ||
| Bursa of the long head of the biceps, average volume, ml (% of cases) | 0,45 (95,3) | 0,27 (40) | 0,15 (9) |
| Subacromi-subdeltoid bursa, average thickness, mm | 0,32 | 0,25 | 0 |
| Subscapularis bursa, average thickness, mm | 0,20 | 0,09 | 0 |
As can be seen from table. 5, before treatment, in most cases (62 patients), fluid was detected in the bursa of the long head of the biceps (Fig. 7). After 2 months of treatment, with changes in tendon characteristics, the amount of fluid decreased, and tenosynovitis was detected in 40% of cases. The lack of positive dynamics in the treatment of tenosynovitis of the long head of the biceps was accompanied by the persistence of a small amount of fluid in its bursa.
Rice. 7.
Determination of fluid in the bursa of the long head of the biceps in B-mode.
A)
Before treatment. The bag contains about 1.21 ml of liquid.
b)
After 4 months of treatment. Reducing the volume of liquid to 0.01 ml.
The amount of fluid in the subacromio-subdeltoid and subscapularis bursae was measured by the thickness of the corresponding bursae. According to the above data, a decrease in fluid is visible after 2 months of treatment and its absence after 4 months. The results obtained completely coincided with the clinical data.
Discussion
The term "tendinitis" means inflammatory changes in the tendon. In reality, this term is not always used correctly. Taking into account histomorphological data, tendinitis shows signs of degenerative rather than inflammatory changes. In such cases, it is more correct to call this process “tendinosis.” However, these changes in etiology are inflammatory, so distinguishing tendonitis from simple tendinosis is important, since the treatment tactics for these diseases are different [4, 5]. Although both processes can be treated conservatively (rest and anti-inflammatory therapy), inflammatory processes that do not respond to treatment require the use of corticosteroids or surgery.
The range of ultrasound findings depends on the type of tendon affected and changes in the adjacent synovial bursa. The tendon is a dense specialized connective tissue consisting of a matrix (type 1 collagen fibrils, elastin, proteoglycans) and fibrocytes [1]. It is surrounded either by connective tissue (epitenon) or by a tendon sheath - a sheath covered from the inside with synovial tissue [1, 3, 5]. On ultrasound, the epitenon looks like an ultrasound line; in tendons with a synovial membrane, a thin hypoechoic strip of fluid can be detected along the tendon.
In tendons with the presence of peritenon, the inflammatory process leads to the development of peritendinitis - thickening of the paratenon, uneven contour of the tendon, the appearance of fluid in the paratenon and in the peritendinous tissues.
According to the authors [2, 5, 8], in the case of tendinitis of a tendon without a synovium (tendon of the supraspinatus, infraspinatus and subscapularis muscles), ultrasound reveals focal expansion of the tendon, an increase in the distance between longitudinally located fibers (a consequence of microtrauma), and the presence of focal hypoechoic areas ( area of inflammation). In most cases, there is a thickening and change in the structure of the tendon along its entire length, which is clearly visible when comparing the tendon with the contralateral side. The decrease in echogenicity of the tendon is due to edema, myxoid degeneration and the presence of vascular proliferation. With long-standing inflammation of the tendon, unevenness of the cortical layer is noted.
With inflammatory changes in the tendon with the presence of a synovial membrane (the tendon of the long head of the biceps), an increase in the amount of fluid is observed around the tendon - tenosynovitis develops. The thickness of the fluid strip may exceed the thickness of the tendon. Synovial fluid may have a heterogeneous structure due to the presence of fibrin, cholesterol, uric acid crystals, calcium pyrophosphate, etc. [5]. There is an increase in the thickness of the synovial membrane and a decrease in its echogenicity. Vascularization in it is not enriched. Acute serous tenosynovitis is diagnosed based on an increased amount of fluid along the tendon sheath, often combined with hyperemia, regardless of the severity of tenosynovitis [4, 5]. With chronic tendinitis, the amount of synovial fluid may not increase. In this case, thickening of the tendon is most often observed. Differential diagnosis is carried out with rheumatoid diseases, in which there is uneven pronounced thickening of the synovial membrane with signs of hypervascularization [2].
In our study, we performed an ultrasound analysis of the thickness, structure, echogenicity and vascularization of the tendons of the rotator cuff muscles before treatment and after 2 and 4 months of conservative treatment. The ultrasound results showed the possibility of monitoring conservative treatment, as well as positive dynamics during the treatment of shoulder tendinitis.
The use of laser therapy as a basic method in patients with bursitis significantly reduced the volume of effusion along the tendon of the long head of the biceps, in the subacromial-subdeltoid and subscapularis bursae, which was reliably confirmed by ultrasound data. The use of hirudotherapy for tendonitis led to a decrease in the inflammatory vascular reaction along the tendons.
Limitations of the study were the inability to compare ultrasound results with MRI and arthroscopy data, as well as the lack of statistical results.
Conclusion
Ultrasound allows non-invasive assessment of the condition of the tendons of the rotator cuff muscles, the severity of inflammatory changes before and during conservative treatment and can serve as an additional method for diagnosing diseases of the shoulder joint.
Literature
- Belenky A.G. Pathology of the periarticular soft tissues of the shoulder joint. diagnosis and treatment//Uch. village Russian Medical Academy of Postgraduate Education. - M., 2005.- 62 p.
- Bouffard JA, Sung-Moon Lee, Dhanju J. Ultrasonography of the Shoulder // Seminars in Ultrasound, CT and MRI. Musculoskeletal Ultrasound - 2000. - June. -Vol. 21(3).- P.164.91.
- Chhem R., Cardinal E. Guidelines and Gamuts in Musculoskeletal Ultrasound // Wiley.Liss-1999. — P. 39.63.
- O`Connor PJ, Grainger AJ, Morgan SR, Smith KL, Waterton JC, Nash AF Ultrasound assessment of tendons in asymptomatic volunteers: a study of reproducibility// Eur. Radiol. — 2004.- Vol. 14. - P. 1968.73.
- Martinoli C., Bianchi S., Dahmane M`H., Pugliese F., Bianchi?Zamorani MP, Valle M. Ultrasound of tendons and nerves // Syllabus Ultrasound-2002. — Mar. — P. 44.55.
- Teefey SA, Middleton WD, Payne WT, Yamaguchi K. Detection and measurement of rotator cuff tears with sonography: analysis of diagnostic errors // AJR-2005. - Vol. 184.- P. 1768.73.
- Teefey SA, Rubin DA, Middleton WD, Hildebolt CF, Leibold RA, Yamaguchi K. Detection and quantification of rotator cuff tears. Comparison of Ultrasonographic, Magnetic Resonance Imaging and Arthroscopic findings in seventy.one consecutive cases // The Journal of Bone and Joint Surgery (American). — 2004.- Vol. 86. - P.708.716.
- van Holsbeeck MT, Introcaso JH Musculoskeletal Ultrasound // Mosby - 2001.- P. 82.129, 463.477, 492.504.
Ultrasound machine HM70A
Expert class at an affordable price.
Monocrystal sensors, full-screen display mode, elastography, 3D/4D in a laptop case. Flexible transformation into a stationary scanner with a cart.
Tendinitis
Tendinitis The shoulder joint has a round shape, which allows for a high range of motion in 3 different planes.
The structure that increases strength and stabilizes the joint is the cuff. It includes the rotator cuff, supraspinatus, infraspinatus, and subscapularis muscles. The supraspinatus tendon attaches to the lesser tuberosity of the humerus and runs in close proximity to the capsule. Features of the anatomical structure determine the frequent combined inflammation of the supraspinatus tendon and other components of the shoulder, consisting of soft tissues. The pathological process spreads to the biceps tendon (biceps). After determining the prevalence of inflammation that accompanies tendinitis of the supraspinatus tendon of the shoulder joint, treatment and rehabilitation are selected by the doctor in accordance with the results of the study.
Symptoms
When the infraspinatus muscle is damaged, symptoms such as pain, stiffness and weakness in the shoulder, arm and even neck may appear. Movements in the arm, such as moving the shoulder back or to the side, may be difficult or impossible (if the muscle damage is severe). The pain may intensify at night and lead to sleep disturbances, especially if the patient lies on the injured side. The infraspinatus muscle can have several trigger points. Each point can be a source of referred pain to different areas of the body. Therefore, diagnosing all trigger points can then allow you to get rid of all referred pain. Pain referred from trigger points can be observed in the shoulder, biceps, mid-scapular area, and there may also be tingling and numbness in the forearm and hand. The pain can be sharp or dull.
Etiology
Inflammation is a complex pathophysiological reaction that develops as a result of tissue damage. In the area of the pathological process, cells of the immune system accumulate, which produce certain biologically active compounds (prostaglandins) that respond to the characteristic manifestations of the inflammatory reaction (pain, tissue swelling, hyperemia). The main provoking factors leading to inflammation are:
- Intense physical activity on the shoulder.
- Previous injuries that affect the cuff to varying degrees (fall on an outstretched arm, bruise, dislocation, fractures of the upper third of the humerus).
- Infectious inflammation, which is the result of the activity of pathogenic (disease-causing) or opportunistic microorganisms.
- Aseptic inflammation developing against the background of local hypothermia in the shoulder area.
- An autoimmune process is a pathology of the immune system in which antibodies are “erroneously” produced to one’s own tissues, in particular the structures of the musculoskeletal system.
- Degenerative-dystrophic processes in which the nutrition of the tissues of the structures of the musculoskeletal system is disrupted, leading to their destruction with the subsequent development of an inflammatory reaction.
After the doctor has diagnosed tendinitis of the supraspinatus tendon, treatment is prescribed taking into account the causes that led to the inflammation.
diagnostics
Diagnosis
Regardless of origin, most diseases of the shoulder joint components have a similar clinical picture. Reliable determination of the extent of changes is carried out using various modern imaging techniques (X-ray, tomography, arthroscopy, ultrasound). To find out the cause of inflammation, a laboratory test is prescribed.
Based on the results that make it possible to establish a diagnosis of tendinitis of the supraspinatus muscle of the shoulder, treatment is prescribed by an orthopedic doctor. In case of autoimmune pathology, diagnosis and prescription of therapeutic measures is carried out by a rheumatologist.