The main symptoms of arthrosis of the talonavicular joint
Let's name the most striking signs that appear at stage 2 of the disease:
- swelling of the foot and ankle;
- pain when walking, when flexing and straightening the foot;
- the pain intensifies in cold and damp weather, with excessive exertion;
- inflammation of the joints and adjacent muscle tissue;
- stiffness in the movements of the lower extremities;
- in later stages – joint deformation and lameness.
The pain is especially acute when walking on uneven surfaces.
Ankle injuries
The main purpose of the ankle joint, formed by the tibia, fibula and talus bones, is to be a reliable support for the musculoskeletal system. This section of the leg must consistently support almost 90% of the total body weight when a person stands or performs any kind of physical activity in an upright position. In addition to supporting functions, the joint provides shock absorption of the limb, various movements of the foot in a normal amplitude:
- flexion;
- extension;
- abduction;
- casting;
- rotation.
The stable functioning of the bone joint is guaranteed by the healthy condition of the ligaments, bones, cartilage, and muscles that form it. If at least one unit of a joint fails, not only its performance is impaired, but also an imbalance in the functions of the entire musculoskeletal system occurs. Diseases of the ankle joint have a detrimental effect on the ability to move, lead to deterioration of gait, and often lead to disability. Often, serious pathologies that may require arthrodesis begin with trivial injuries localized in this area:
- bruises;
- dislocations and subluxations;
- ankle fractures;
- violation of the integrity of the heel bone;
- ligamentous distortion (sprains, tears of ligaments, etc.).
Lesions of a traumatic nature often occur as a result of direct exposure to mechanical force, which is provoked by local impacts, falls from a height, unsuccessful jumps, and sharp rotational turns. After all, sometimes it is enough for a person to simply slip on a slippery surface or trip for damage to the constituent structures of the ankle.
Any traumatic lesions require timely diagnosis and immediate treatment. After a certain period, the injury, if proper medical care was not provided in due time, makes itself felt with serious consequences. Pathologies resulting from an old injury, against the background of imaginary well-being, are manifested by the sudden onset of pain and increasing limitation of the locomotor and support potential. People don’t understand what happened, where the discomfort came from, and the cause turns out to be a past injury.
Remember! Complex degenerative-dystrophic processes, often irreversible, predominantly do not develop on their own, but are diagnosed as a post-traumatic complication. The most common pathologies of post-traumatic origin with a serious progressive course are arthritis and osteoarthritis.
Arthrosis, in turn, is a consequence of arthritis. This is the chain mechanism for the development of a complex clinical situation. It is not difficult to go from injury to deforming osteoarthritis (DOA) in a couple of years. But if the injury is not difficult to treat conservatively, then with arthrosis of the ankle joint everything is different - it is an incurable disease that critically depresses the quality of life and negatively affects the statics and dynamics of the entire limb.
How is the disease diagnosed?
To make a diagnosis, examining and interviewing the patient is not enough. Special studies are required:
- Radiography. The image shows narrowing of the joint space, subchondral sclerosis and subchondral cysts, osteophytes and late stage foot deformity.
- MRI. Allows you to most accurately diagnose articular cartilage defects, effusion in the joint cavity, synovitis, ligament damage, tenosynovitis and tendon ruptures, as well as reactive changes in the bone marrow and other pathologies.
- CT. Indicated if there is a need for a three-dimensional image of the joint, especially at the stage of preoperative planning. Helps assess the condition of adjacent joints and the nature of bone fusion. More informative than an x-ray.
- Ultrasound. This diagnostic method is recommended for determining inflammatory processes inside the joint and monitoring effusion. It shows pathological changes in the soft tissue around the joint.
- Bone scintigraphy. Prescribed if there are special indications.
Most often, all arthrosis of the talonavicular joint is diagnosed using MRI.
What is included in the treatment plan
If the treatment regimen for osteoarthritis is drawn up correctly, it is possible to completely restore joint mobility. Conservative treatment includes the following methods and measures:
- Adjustment of physical activity. During the therapy period, it is important to limit high-intensity loads, especially twisting and bending.
- Change of shoes. The patient is advised to wear high boots for ankle support or shoes with rounded soles to relieve stress on the midfoot.
- Orthopedic insoles or orthoses. Reduce stress and pain.
- Cane. Unloads the damaged limb segment.
- Weight correction. Extra pounds aggravate the course of the disease.
- Non-steroidal anti-inflammatory drugs. Stop inflammation.
- Analgesics. Relieves pain.
- Muscle relaxants. Relaxes muscles and fights spasms.
- Chondroprotectors. Helps renew cartilage tissues.
- Physiotherapy. Strengthens the muscles around the joint, stretches the lower leg muscles, and reduces the load on the affected joint.
- Physical exercise. Exercise therapy restores range of motion, strengthens the ligamentous apparatus and reduces the load on the sore joint.
If stiffness is severe, physical therapy may be harmful.
Deforming osteoarthritis of the ankle joint: how does it appear?
The ankle joint does not have its own vascular system, therefore, with metabolic disruptions caused by aging, intense training or other factors, the nutrition of the cartilage tissue is also disrupted. Due to the lack of “building materials” and important microelements, intracellular metabolism decreases, cartilage recovers poorly and slowly, and its basic structure gradually changes.
Chondroitin and glucosamine are synthesized less frequently and in small volumes, which are not enough to support and timely restore the joint. Hence the loss of elasticity, shock-absorbing properties and strength, and the formation of bone growths. In the future, if the disease starts and you don’t know how to treat osteochondrosis of the ankle joint, the cartilage will continue to deteriorate.
In the initial stages of the disease, symptoms of osteoarthritis of the ankle joint are rarely bothersome. Sometimes there is pain, but it goes away as quickly as it started.
Factors that can provoke OGS:
- Poor nutrition.
The body lacks protein, fatty acids and other essential substances.
- Uncomfortable shoes.
For example, high heels.
- Heredity.
- Age-related changes.
- Increased sports loads.
For example, boxing or dancing. There is also a high risk of arthrosis if you suddenly stop playing sports.
- Excess weight.
Excess weight significantly increases pressure on the joints.
- Flat feet, high stature, congenital dysplasia.
- Concomitant diseases such as diabetes, hemophilia, osteochondral disorders or vascular atherosclerosis.
It may occur due to problems with hormones or the thyroid gland. Especially at risk for women during menopause.
- Inactivity.
A lack of daily physical activity weakens muscles, which significantly increases the load on joints.
- What else potentially influences the development of ankle osteoarthritis?
- Hypothermia of the legs.
For example, your feet are cold because your shoes are not appropriate for the season.
- Carrying heavy things.
Arthrosis is especially often diagnosed among loaders.
- Injuries in the ankle area.
Any dislocations and fractures can cause cracks in the cartilage tissue. If microtrauma is not noticed and treated in time, serious consequences and diagnoses cannot be avoided.
In addition, the prerequisites include different leg lengths (due to shifting loads), damage to internal organs, and deformation of the toes. Work that requires a person to stand for a long time throughout the working day also often becomes an aggravating factor along with obesity.
Injection therapy
With deformations of cartilage tissue in the joint, there is always a deficiency of synovial fluid. It contains hyaluronic acid, which acts as a lubricant and shock absorption during movements. If there is not enough fluid, the cartilage surfaces wear out with double force and are damaged faster.
Therefore, in case of arthrosis, patients are primarily recommended to inject synovial fluid prosthesis. The drug is administered under anesthesia under ultrasound guidance. It moves the rubbing surfaces apart and restores mobility to the joint.
Injections into the joint for arthrosis relieve pain for several months, after which they need to be repeated. Why does this happen - expert comment:
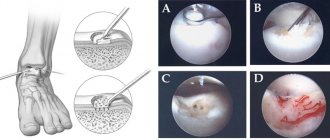
When is surgery needed?
If conservative treatment does not help, the pain intensifies, mobility is limited, and the patient is recommended to undergo surgery. One option is talonavicular arthrodesis. The surgeon removes the damaged parts of the joint and “locks” the joint, after which mobility returns to it. After surgery, a complication is possible - the formation of a false joint, when the bones do not heal (5-10%), and a repeat operation is necessary.
If, in addition to the talonavicular joint, other nearby joints (subtalar and calcaneocuboid) are also damaged, arthrodesis of all of them is performed.
There are no methods for endoprosthetics of the talonavicular joint
Preparing the patient for ankle arthrodesis
When planning this type of surgical treatment, it is extremely important to evaluate all joints adjacent to the problem area. This is necessary to understand how capable neighboring segments are of taking on a larger load complex. Since the movement potential of the ankle joint is blocked after surgery, the adjacent movable joints will naturally be subject to more stress. It is especially important to reliably assess the condition of the talonavicular joint, because it is precisely this central segment of the foot that will bear the maximum share of the load. A positive effect from arthrodesis can be counted on only in the absence of degenerative pathogenesis in it.
The go-ahead to operate on a patient is given only after a comprehensive examination confirming the clear need for this medical care in the absence of contraindications. The patient is prescribed a series of diagnostic measures:
- detailed blood and urine tests, including biochemistry;
- X-ray, MRI or CT scan of the joint in several planes;
- testing for HIV, syphilis, hepatitis;
- fluorography and electrocardiography;
- examination by highly specialized doctors (cardiologist, pulmonologist, etc.);
- consultation with an anesthesiologist.
In addition, the specialist must additionally make sure that the effect of arthrodesis is most likely to “work” and the patient’s well-being will noticeably improve. To do this, a kind of test is first carried out, which consists of applying a plaster cast to the joint. So, a person walks with his ankle fixed in a cast for about 7 days, and after a week, the orthopedic traumatologist finally determines the feasibility of the operation. If the test immobilization helped to create support for the limb and significantly reduce pain, the operation is performed. If discomfort persists, pain appears or pain increases, or gait worsens, arthrodesis is cancelled.
Technique No. 2.
A week before the expected date of the intervention, the use of drugs with anti-inflammatory effects (NSAIDs) and agents that have blood-thinning properties should be stopped. On the eve of surgery, the diet should be light, stop eating 6-8 hours before.
Attention! Make sure your living space is prepared in advance when you arrive home from the hospital. You should remove carpets, runners and cords from floors that could cause your foot to get caught and fall. Place essential items and things in easily accessible places. In the bathroom it is necessary to lay non-slip mats made of rubber or silicone materials with Velcro, etc.
Is it worth treating talonavicular arthrosis?
The disease is quite insidious. It can progress for years and then lead to serious complications. The joint will never be the same as it was before. Pain will significantly affect the quality of life and ability to work, it will intensify first at night and then at rest. Over time, the foot becomes deformed and prevents you from leading your usual lifestyle. Degenerative processes will spread to neighboring joints.
If you notice the slightest signs of pain and discomfort in your foot, do not attribute them to fatigue. Visit an orthopedist and make sure that you are not at risk of arthrosis of the knee or ankle.