Deviations from the normal development of joints when they become chronic are almost impossible to treat. As they progress, they leave less and less chance of normal movement. In knee replacement surgery, the damaged part of the joint is replaced with an artificial implant.
This operation is usually performed on people over 50 years of age. Upon reaching this age, many people notice pain and a feeling of stiffness in their knees. If traditional treatments do not work, joint replacement will restore the ability to move and allow you to lead a normal life.
Indications for knee replacement
- Deforming arthrosis. With this disease, the bone constantly grows and becomes denser.
- Rheumatoid arthritis, which affects connective tissue and small joints.
- Metabolic disorders. Often problems with knee joints arise due to gout and diabetes.
- Joint dysfunction after trauma and injury.
- Improper healing after fracture.
- Neoplasms of various types in bone and cartilage tissues that prevent the joint from functioning normally.
Treatment of the knee joint in Germany: autogenous cartilage transplantation
Treatment of the knee joint in Germany using autogenous cartilage transplantation - a new method in orthopedics!
Own (autogenous) cartilage cells, which are then used for “replanting”, are cultivated in the laboratory.
Cartilage (cartilage cell or chondrocyte) transplantation is a surgery that helps repair cartilage damage by replacing dead cells with new ones. Only trained specialists can successfully perform this operation.
The benefits of cartilage cell transplantation include:
-reduction and sometimes complete elimination of pain; — increasing load tolerance; — improvement of joint mobility; — restoration of the cartilage layer; - refusal of an artificial joint. Thanks to the fact that real cartilage tissue can now be built up at the site of the defect, for the first time it is possible to completely eliminate the problem. Previously, the postulate was that cartilage cannot be restored, you can only slow down the process of its destruction.
Cartilage transplantation - the essence of the process
Autogenous cells (i.e., the cells of the person himself) are used for transplantation. Moreover, these cartilage cells are grown directly in our laboratory. To do this, endoscopic imaging is performed to assess the condition of the joint, the extent of damage, and also take a sample of cells from intact cartilage. After that, they are sent to the laboratory and multiplied outside the body, in a test tube.
The transplantation procedure itself is a minimal surgical intervention through arthroscopy. Two small incisions (1-2 cm) are made through which cells are introduced using a special apparatus.
There are many reasons for joint damage: injuries, fractures, inflammation... You can’t list them all. However, the final process is often the same - partial or complete destruction of cartilage tissue, which leads to arthrosis. Cartilage is practically incapable of regeneration, and with age the situation progressively worsens. This leads to pain, difficulty moving, and sometimes complete immobility in the damaged joints.
Only cartilage transplantation can create the effect of regeneration, that is, complete restoration of structurally and functionally identical cartilage tissue.
In certain conditions, further development of a similar method of treating cartilage damage using 3D chondrospheres, along with autogenous cartilage transplantation (also called autogenous chondrocyte transplantation, abbreviated ATC), offers the opportunity to prevent the need for early joint replacement.
Transplantation of one's own cartilage cells involves certain differences between the classic ATC method and the improved version of ATC in 3D.
In the case of classical ATC, the autogenous periosteum is sutured into the area of the treated defect under waterproof conditions, followed by the injection of grown cartilage cells into this cavity.
Three-dimensional cartilage cell transplantation (autogenous matrix-induced chondrocyte transplantation, abbreviated ATC 3D) involves the introduction of three-dimensional balls of cartilage cells (spheroids) into the treated defect area, without the need to remove the coating.
This surgical intervention is performed using the microarthrotomy technique under arthroscopic control. This method provides the most gentle treatment (minimally invasive), which significantly reduces the risks associated with the operation.
The viability of the cartilage tissue surrounding the defect is more significant in comparison with the actual age of the patient.
Operation technique
Stage: collection of a sample of cartilage tissue (biopsy) of the knee joint (collection of a sample of knee cartilage).
During arthroscopic intervention (joint endoscopy), a fragment of your own cartilage tissue is first taken. Cartilage cells are isolated from the collected tissues in a highly specialized laboratory for growing cell cultures, followed by cultivation under sterile conditions.
Cartilaginous tissue is taken from a healthy, minimally exposed area of the joint. The surgery is performed on an outpatient basis and takes approximately 30 minutes. At the same time, about 120–150 ml of blood is taken from the patient. This blood is intended for serum production in the laboratory.
Stage: cell cultivation in the laboratory. Cartilage cells multiply in the patient's own blood serum. This method eliminates contact with foreign proteins and helps maintain cell growth conditions at a stable level. Thus, we eliminate as much as possible the risk of cartilage rejection in the future, because only cells from the person who is preparing for treatment are used.
The collected sample, about the size of a grain of rice, is sent, along with the patient's blood, to co.don® AG.
The process of maturation of new cells lasts approximately 3 to 4 weeks, when small three-dimensional aggregates of cartilage cells are formed.
At the end of the cultivation time, the biological medicinal material is sent to the attending physician. The material is transported over several hours under certain conditions, in special refrigerated vessels, in order to preserve the quality of the cells.
Stage: implantation of cartilage cells of the knee joint with chondrospheres. The treated cartilage defect in the joint is filled with cartilage balls (chondrospheres). The cells are immediately fixed to the bone tissue, filling the defect and eliminating it.
Once the cartilage spheroids contact the defect itself, their “tether molecules,” adhesion proteins, remain relatively mechanically unstable in the vicinity of the bone tissue for approximately 10 minutes. Then cartilage cells grow into the defect until it is completely filled.
This intervention is performed using a minimally invasive method under arthroscopic control and lasts approximately 30–60 minutes. In this case, the damaged cartilage tissue is first removed, and then cultured aggregates of cartilage cells are introduced.
The benefits of cartilage cell transplantation, from a medical point of view, have been confirmed over 25 years of scientific research since the development of the method.
Currently, a minimally invasive arthroscopic technique is available for eliminating cartilage defects of the knee, ankle and hip joints.
The implanted material is not perceived by the body as a foreign body, because it has properties identical to natural cartilage.
Thus, living chondrocytes are capable of building a new functioning cartilage layer. Due to the fact that cartilage cells cultured in spherical form (so-called spheroids) are placed in the second stage directly into the area of the damaged joint where there is a lack of cartilage mass, the cells continue to multiply in the body in the place where cartilage is needed.
This leads to the development of healthy autogenous cartilage tissue, which has all the protective properties that the damaged joint lacked.
What happens after surgery?
After just 6 weeks, complete coverage of the defect with living cartilage cells is observed, which do not yet have the density and resistance to stress characteristic of the surrounding cartilage tissue. Therefore, for some time it is necessary to use a cane to unload the joint. At the same time, you should pay attention to sufficient joint mobility, which will help improve blood circulation.
Cartilage nutrition is realized by diffusion. When tissues are compressed, toxins are released, and when unloaded, on the contrary, nutrients are supplied. Healing is facilitated by special motor splints and physical therapy.
When is it possible to return to previous loads?
After approximately 6 weeks, partial weight bearing should be started, with the cane being discontinued after a maximum of three months.
When are sports allowed?
Cycling, swimming and other joint-friendly sports are allowed after approximately three months. After complete regeneration of the cartilage defect, approximately one year after the operation, when the new cartilage has completely healed, the joint can be loaded by doing any kind of sport.
Who can this method help?
Cartilage transplantation is not always a treatment option. If the joint is too large or the joint surface is very damaged, it is too late to carry out this procedure.
The main prerequisites for successful cartilage transplantation are a stable joint, a normal articular axis and the absence of fragments in the joint cavity that could damage the graft.
The main indications for transplantation of cartilage cells (chondrocytes) are local defects of articular cartilage, especially the knee or ankle joint. Ideal conditions for transplantation in patients aged 15–55 years are a defect size of up to 10 cm2, in the presence of healthy residual cartilage tissue.
The knee joint must be stable, that is, the ligaments must be intact. Unusual loads on the joint, such as excess body weight, should be avoided whenever possible.
Thus, despite the fact that this method is recommended for patients under the age of 55 years, the decisive factor is the biological, and not the calendar age of the patient.
Cost for 2 operations - 18,000 Euro (including operation to remove cells 7900 Euro)*
Stay in the clinic - 3 days
Rehabilitation period - 8 weeks (including outpatient 2 weeks)
- Prices may vary depending on the patient's condition.
Treatment of the knee joint in Germany using autogenous cartilage transplantation in more than 90% of cases increases the likelihood of successful treatment and gives positive postoperative results.
arthrosis of the joints, modern treatment in Germany, how arthrosis is treated in Germany, knee joint in Germany, treatment of arthritis and arthrosis in Germany, treatment of arthrosis in Germany, knee joint surgery in Germany
How is knee replacement surgery performed?
Endoprosthetics is performed according to a specific algorithm:
- Introduction of anesthetics. Typically, a local anesthetic is used when the substance enters the spinal canal.
- The operating surgeon makes an incision on the front of the knee to gain access to the diseased joint.
- After the joint is opened, the damaged areas are removed to be replaced with artificial ones.
- Artificial pads that make up the endoprosthesis are installed in the kneecap and fixed with bone cement. Other fixation options are also possible.
- The wound is sutured in layers, securing the incision with special staples.
- A silicone drainage tube is installed to drain the blood into a special container.
- Apply a postoperative wound dressing and wrap the leg with an elastic bandage.
Treatment methods and repair of cartilage tears
There are 2 types of treatment for cartilage tears: conservative and surgical.
Conservative treatment
If you go to the clinic in a timely manner and the disease is at an early stage, the specialist will prescribe conservative treatment.
First of all, it is necessary to stop putting stress on the knee joint. The doctor may also prescribe vitamins for joints, anti-inflammatory and painkillers, and pinpoint injections with hyaluronic acid. The treatment package may include a course of physical exercise and wearing orthopedic devices.
Another method is plasma lifting. This method is based on the use of platelets taken from the patient's blood. The specialist takes blood, uses centrifugation to isolate platelets, and injects the resulting material into the joint.
Plasmolifting is based on the principle of self-healing of the body.
Operation:
Minimally invasive: 2 incisions are made, each a few cm. A mini-camera (arthroscope) is inserted through the first incision, which transmits the image to the monitor. Instruments are inserted into the joint through another hole. Depending on the condition of the joint, the cartilage is restored, microfracturing (formation of microfractures of the subchondral bone) or bone treatment using an arthroscopic drill (abrasive arthroplasty) is performed. Thanks to local hemorrhage, bone marrow stem cells penetrate into the damaged areas, which leads to the formation of new cartilage.
Duration of the operation and recovery period:
Cell extraction is performed under short-term general anesthesia or neuraxial anesthesia. The intervention is performed arthroscopically (minimally invasive). Two small pieces of cartilage are taken from the intact part of the joint to further culture autogenous chondrocytes in the laboratory. After 3-8 weeks, the grown cartilage tissue is transplanted to the damaged area of the joint. This is done through a 2-3 cm long incision, sometimes even arthroscopically. 2-3 days of stay in the clinic. Postoperative treatment is also important. For about 6 weeks you will need to rely on crutches, but even then you should return to normal work and sports life slowly and carefully.
The purpose of arthroscopic chondroplasty
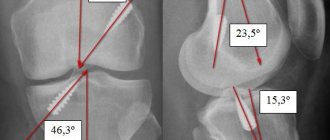
Making an accurate diagnosis for cartilage pathologies is quite difficult. X-ray examination and MRI in this case can give an inaccurate and erroneous result. Such examination methods are informative only in cases of extensive damage. That is why arthroscopic examination of cartilage tissue is the most effective way to diagnose joint diseases. Often during operations on menisci or ligaments, the surgeon discovers pathology and decides to eliminate it.
Chondroplasty involves achieving the following goals:
- restoration of damaged cartilage;
- as a result - a decrease in pain.
Knee cartilage damage symptoms
Symptoms of a cartilage injury may not appear immediately like they do with an ACL tear or meniscus tear. Similar to the initial stages of arthrosis, the first symptoms are weak and unnoticeable, progressing over time and developing into much more serious and noticeable ones for the patient.
Symptoms of knee cartilage damage—if they have begun to appear—include:
• periodic swelling of the joint (sometimes this is just a symptom without a disease)
• pain after prolonged walking or climbing stairs
• when the body is fully loaded on the knee, its deformation, the patient may also fall due to the fact that the knee could not bear the weight
• clicks or blockages
• the knee may creak when moving
Diagnosing knee cartilage damage can be quite challenging. Knee swelling does not always indicate cartilage damage. Using X-rays, MRI or arthroscopy, you can more accurately determine whether the cartilage is fine or whether it has already worn out (as abrasion reduces the space between the surfaces of the bones).
Damage to the knee cartilage occurs in several stages and can reach complete abrasion and exposure of the end of the bone
Cartilage grown from nasal septum cells helped Swiss patients with knee osteoarthritis
Berkshire Community College Bioscience Image Library
Surgeons from Italy, the USA and Switzerland have developed a new method for treating osteoarthritis and tested it on the first patients. They grew cartilage from nasal septum cells and then implanted it into the inflamed knee joint of two patients. 14 months after surgery, the index scores of the patients, which assess the course of osteoarthritis, increased, which indicates an improvement in their condition. The study was published in Science Translational Medicine.
Osteoarthritis develops when the cartilage tissue of a joint is damaged due to injury, malformation, or infection. Chronic inflammation deforms the joint and over time makes it difficult for the patient to move. The final stage of osteoarthritis is joint ankylosis (fusion of the articular ends of bones) with complete loss of mobility. Anti-inflammatory drugs are used to treat osteoarthritis, and in case of severe lesions, joint replacement is performed, that is, parts of it are replaced with implants.
There is another method for treating articular cartilage injuries, but it is usually not possible to use in cases of osteoarthritis. For local minor injuries to the joint, surgeons transplant cartilage cells from a healthy area of the joint, but if this method is used in a patient with osteoarthritis, the transplanted cells will develop poorly due to chronic inflammation in the joint. Researchers from Italy, the USA and Switzerland, led by Karolina Pelttari from the University of Basel, noticed that nasal septum cartilage cells proliferate better than joint cartilage, so they decided to try transplanting them into patients with osteoarthritis. After successful experiments on mice, doctors tested the method on two patients with osteoarthritis: a 36-year-old woman and a 34-year-old man. Both patients were diagnosed with severe osteoarthritis of the knee joint and were referred for prosthetic replacement, but they chose experimental treatment.
First, a small amount of cartilage was taken from the patients' nasal septum, and then plates of cartilage tissue were grown from these cells in the laboratory. Doctors implanted the resulting cartilage onto patients' defective articular surfaces of the knee joint. Magnetic resonance imaging showed that the cartilage had taken root. After 14 months, the patients' condition was assessed using the Osteoarthritis Course Index (KOOS). All indicators of this index (pain, symptoms, quality of life) among the participants increased by 20-30 units. These results indicate an improvement in the course of osteoarthritis.
Addition from the editor
KOOS index scores of 0 indicate extreme severity of symptoms, and scores of 100 indicate absence of symptoms.
That is, if the pain index is 100, this means that the patient does not feel pain. Share
MRI of the knee joint: e – before surgery, f – after surgery
Acevedo Rua et al / Science Translational Medicine, 2021
Share
To fully evaluate the effectiveness of this treatment, studies will need to be conducted on a larger number of patients. Pelttari's team recently received ethics committee approval to conduct a clinical trial of their method on 15 patients with osteoarthritis, and if all goes well, they will enroll a further 64 patients in the study.
Recently, American doctors suggested treating osteoarthritis with an antidepressant. They found that the antidepressant paroxetine could stop and even partially reverse the destruction of cartilage.
Anastasia Kuznetsova-Fantoni
What processes lead to the need for cartilage transplantation?
Healthy cartilage is essential for the normal functioning of our joints. It acts as an elastic spacer between the bones, reducing friction and stress. Normal cartilage contains intra-articular fluid
, which acts as a lubricant. If the cartilage is worn out or injured, the heads of the bones begin to rub against each other, causing pain and making movement difficult. Cartilage degeneration can also be caused by genetic defects.
The main problem in the treatment of cartilage damage is the lack of a mechanism for restoring cartilage tissue cells - cartilage cannot return to normal on its own. Atrophy processes develop in damaged cartilage tissue
. The problem of damaged cartilage was previously solved either by transplanting a fragment of healthy cartilage tissue (this technique has disadvantages - for example, the transplanted cartilage can be rejected) or by installing an endoprosthesis.