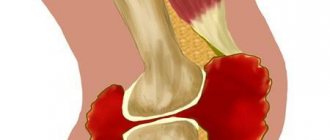
When, 2-3 days after an unsuccessful fall or intense physical activity, pain and a characteristic round swelling in the joint occur, there is reason to suspect bursitis. This condition requires special attention from the patient and the doctor - if not treated correctly, the inflammation can lead to the need to remove the joint capsule or become chronic. Need quick and competent medical care.
Bursitis is treated at the Kuntsevo Treatment and Rehabilitation Center - here there is everything necessary for this - from a high-tech diagnostic base to a modern exercise therapy room and experienced doctors.
What is acute bursitis
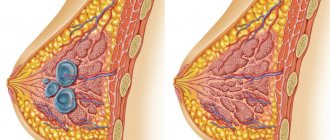
A person has about one hundred and sixty joint capsules (bursae). This is a special formation of strong connective tissue on the outside and a special layer of cells on the inside. Their task is to protect joints from external influences, injuries and friction of articular elements against each other. This is ensured with the help of a special synovial fluid, which is produced in the joint and improves gliding. In addition, it is this liquid that contains components that penetrate the cartilage tissue and provide its nutrition and hydration.
When the bursa becomes inflamed, the amount of fluid in it increases and its composition changes. Protein exudate, inflamed cells appear in the lubricating fluid, swelling of the joint capsule occurs - formation up to 5-10 cm in size. This leads to impaired mobility - any movement causes pain in the affected joint, and sometimes it bothers you even without physical activity.
The initial inflammation that occurs is acute bursitis. Typically, it occurs with severe symptoms that gradually decrease (with the exception of purulent bursitis). Untreated inflammation can lead to complications - the formation of purulent fistulas, phlegmon and tissue sepsis. Protracted acute bursitis becomes a chronic form of the disease. In this case, bursitis can worsen whenever immunity decreases or there are other risk factors for relapse. Chronic bursitis will be more difficult to cure.
How does inflammation of the bursae manifest?
Symptoms of bursitis vary depending on the type of inflammation. But among the general signs the following symptoms can be identified:
- swelling at the site of the elbow lesion - there is no pain;
- difficulty in movement;
- skin color takes on a red tint;
- a tumor forms - after some time, pain appears;
- general body temperature rises, headaches or problems with appetite may occur;
- Difficulty occurs when moving the elbow.
At the first signs of bursitis, it is recommended to seek help from a specialist. Self-diagnosis and self-medication can cause serious consequences and undesirable development of the disease.
Types of acute bursitis
Inflammation of the bursa can occur in any of the joints. Bursitis most often occurs in large joints:
- Elbow.
- Shoulder.
- Hip.
- Knee.
- Radiocarpal.
The name also changes depending on the location of the inflammation: acute bursitis of the elbow joint, acute bursitis of the knee joint, and so on.
Another classification is based on the causes of inflammation:
- Septic bursitis occurs due to bacterial infection. Most often the cause is Staphylococcus aureus (about 80% of cases) and streptococci, but there may be other pathogens.
- Aseptic bursitis develops due to non-infectious causes - injuries, constant pressure or physical activity, existing joint diseases.
To predict the further course of the disease and select a treatment method, it is important to understand how the synovial fluid has changed. Bursitis is classified according to the nature of the exudate:
- Serous - plasma with an admixture of blood elements is formed in the bag.
- Hemorrhagic - a large number of red blood cells in the exudate.
- Purulent - an accumulation of microorganisms and destroyed cells. This is the most dangerous variant of acute bursitis with severe pain, rapid
- development and risk of complications - breakthrough of pus into the periarticular tissues and blood poisoning.
Modern approaches to the treatment of bursitis (recommendations for an outpatient surgeon)
For citation. Akhtyamova N.E. Modern approaches to the treatment of bursitis (recommendations for an outpatient surgeon) // RMZh. 2021. No. 3. pp. 193–196.
Pathological processes in extra-articular soft tissues (skeletal muscles, tendons and their synovial sheaths, fascia, aponeuroses, synovial bursae) constitute a large group of pain syndromes of the musculoskeletal system and are united under the name “diseases of soft periarticular tissues” [1–4].
Diseases of soft periarticular tissues are very common, and currently there is a tendency towards a further increase in the incidence of this nosology. According to literature data, in a survey of 6000 people, lesions of periarticular soft tissues are detected in 8% of individuals. At least 25–30% of patients seeking outpatient medical care from surgeons, traumatologists, neurologists, and rheumatologists are patients with lesions of soft periarticular tissues [3, 4]. Pathological changes in the periarticular soft tissues can be a manifestation of both local and systemic disease. Most often, damage to extra-articular tissues is local in nature in the form of bursitis, tendinitis, tenosynovitis, tendovaginitis, enthesitis, fasciitis - due to local overloads, microtraumas and overstrain, especially against the background of congenital or acquired skeletal anomalies, such as scoliosis and kyphosis of the spine, hypermobility syndrome, axial bone deformations, etc. [3, 4]. On the other hand, extra-articular lesions can be one of the manifestations of systemic diseases, including inflammatory (rheumatoid arthritis, seronegative spondyloarthritis), endocrine (diabetes mellitus, hypothyroidism), metabolic (gout, hyperlipidemia, etc.) [1]. The structure of diseases of extra-articular soft tissues is represented by more than 50 independent nosological forms, among which lesions of the tendon-ligamentous apparatus, called diseases of periarticular soft tissues, prevail: periarthritis, enthesopathies, tendonitis, tendovaginitis, ligamentitis, bursitis, etc. [1]. Despite the high prevalence and variety of forms of damage, there is still no unity in terminology, methods of examining patients and criteria for diagnosing soft tissue diseases. Various options for systematizing lesions of extra-articular soft tissues were proposed: diseases were grouped according to anatomical, etiopathogenetic principles, clinical manifestations, etc. Classification and systematization of nosologies is necessary in order to improve diagnosis. The most reasonable systematization of lesions of periarticular soft tissues according to the anatomical and functional principle seems to be most reasonable. According to this principle, all lesions of periarticular soft tissues can be combined into 4 groups [2]. I. Muscle diseases
1.1.
Inflammatory muscle diseases – myositis 1.2. Non-inflammatory muscle diseases – myopathies 1.2.1. Reactive 1.2.2. Metabolic 1.2.3. Endocrine 1.2.4. Vascular 1.2.5. Toxic II.
Lesions of fibrous and synovial formations 2.1.
Tendinitis 2.2. Tenosynovitis and tenosynovitis 2.3. Bursitis 2.4. Ligamentitis – tunnel syndromes 2.5. Fasciitis and aponeurositis 2.6. Combined forms of damage - periarthritis 2.7. Combined forms of damage III.
Diseases of subcutaneous fat tissue 3.1.
Erythema nodosum 3.2. Painful lipomatosis - Dercum's syndrome 3.3. Panniculitis IV.
Primary fibromyalgia Despite the high prevalence of the disease, the variety of nosological forms and the high level of disability caused by the pathology of extra-articular soft tissues, to date this problem has received undeservedly little attention. One of the most common nosological forms of damage to periarticular soft tissues is bursitis. The proportion of this pathology in the general structure of diseases of the musculoskeletal system is very high, therefore this pathology attracts the close attention of specialists. Ideas about it have changed and been supplemented as a result of recent research. Often, bursitis was rightly considered a typical pathology of representatives of certain professions, which determine the localization of the process: the elbow joints are more often affected by tanners, engravers, polishers, and embossers; knee - for tilers, parquet workers, miners; shoulder - for blacksmiths, loaders; bursitis of the anterior surface of the scapula - in diggers and sawyers; calcaneal bursitis – among sellers and ballerinas [5–7]. However, occupational bursitis is only part of the problem of pathological processes faced by doctors in both outpatient and inpatient practice. According to modern concepts, the key factor in the development of bursitis is mechanical damage to the periarticular bursa, less often - infection, metabolic disorders, intoxication, allergic reactions, autoimmune processes. Mechanical damage may be associated with excessive load or a decrease in tolerance to the previous load with age-related changes [8]. Mechanical load on the synovial bursa leads to an increase in the production of synovial fluid, thereby providing the necessary shock absorption of the structural elements. The structure of the synovial bursa is favorable for the development of inflammation. It is a narrow slit-like cavity lined with synovial membrane, delimited from surrounding tissues by a capsule and filled with synovial fluid. Such features ensure the attachment of an infectious component and the formation of inflammatory infiltrates. Synovial macrophages play a key role in the formation of the immune response and can be activated by a variety of proinflammatory factors, so constant antigenic stimulation of the synovium can contribute to the development of chronic bursitis [5, 8, 9]. In clinical practice, there are classifications of bursitis of different causes [5]: • taking into account the location (elbow, knee, shoulder joint, etc.) and the name of the affected bursa; • depending on the clinical course: acute, subacute, chronic bursitis; • aseptic (non-infected) and infected bursitis; • taking into account the pathogen: specific (for syphilis, tuberculosis, brucellosis, gonorrhea) and nonspecific bursitis; • according to the nature of the exudate: serous (plasma mixed with a small amount of blood cells), purulent (microorganisms, destroyed cells, disintegrated leukocytes), hemorrhagic (liquid with a large number of red blood cells) and fibrinous (high fibrin content) bursitis. The clinical manifestations of bursitis are determined by the peculiarities of the structure and function of the joint around which the synovial bursae are located. The leading symptom of bursitis is a round, fluctuating swelling that appears at the site of the lesion, painful on palpation, with symptoms of local hyperthermia. In addition, clinically, bursitis is characterized by the presence of pain, which significantly reduces the quality of life of patients. In most cases, the duration of the disease is limited to one to two weeks and does not pose a serious danger to human health. However, with the addition of microbial flora and the further development of the inflammatory process, serous inflammation quickly turns into a purulent form. The spread of the purulent process to surrounding tissues can occur as a phlegmonous inflammation with necrosis of the bursa wall and the formation of subcutaneous and intermuscular phlegmon. In advanced cases, long-term non-healing fistulas form. The breakthrough of pus into the joint cavity leads to the development of purulent arthritis. The most common bursitis is the elbow bursae and the bursae of the shoulder, hip and knee joints, as well as the Achilles tendon area. Elbow bursitis in most cases is a consequence of chronic injury during sports or professional activities. In this case, the subcutaneous synovial bursa of the olecranon process is mainly affected, and less commonly, the radiobrachial synovial bursa of the lateral epicondyle [7, 8]. In the area of the shoulder joint, the most commonly affected bursae are those that do not communicate with the joint cavity - the subcutaneous acromial, subdeltoid and subacromial. Complaints boil down to pain during abduction and rotation of the upper limb. Bursitis of the subdeltoid bursa is especially painful [7, 10]. Bursitis in the hip joint is characterized by severity. The deep-lying iliopectineal bursa, located between the muscles and the joint capsule, as well as the superficial or deep synovial bursae in the area of the greater trochanter of the femur are more often affected by inflammation. Bursitis of these localizations is accompanied by pain in the hip joint, aggravated by walking, especially at the beginning of movement, and local pain on palpation in the greater trochanter. Active movements, especially external rotation and abduction, are acutely painful. Iliopsoas bursitis is associated with inflammation of the bursa located between the iliopsoas muscle and the anterior surface of the hip joint. The bursa is large and in some cases communicates with the joint cavity. When a significant amount of exudate accumulates in it, it can be detected in the groin in the form of a tumor-like formation. Bursitis is accompanied by pain in the hip joint. Compression of the femoral nerve by a stretched bursa can lead to pain and paresthesia in the thigh [8, 11]. The appearance of limited swelling in the area of the knee joint is observed when the synovial bursae are affected. Thus, in the popliteal region, a limited elastic formation may be detected, associated with inflammation of the semimembranosocnemius bursa (Baker's cyst). In some patients it reaches a large size and can spread to the lower leg. Limited swelling in the area of the patella is characteristic of prepatellar bursitis. The development of infrapatellar bursitis leads to the formation of a cyst-like formation that protrudes on either side of the patellar tendon. Foot anserine bursitis is an inflammation of the synovial bursae located in the area where the semitendinosus, sartorius, and gracilis tendons attach to the tibia. It is usually not accompanied by significant swelling, but causes pain during exercise and local tenderness upon palpation in the affected area [6, 8, 11, 12]. A consequence of heavy physical activity can be bursitis in the Achilles tendon area. Bursitis of this localization is accompanied by pain near the site of attachment of the Achilles tendon to the heel bone. Objectively, swelling, hyperemia of the skin, and local pain on palpation are determined in this area [11]. Particular attention should be paid to the timely treatment of bursitis, since the lack of effectiveness of treatment measures leads to long periods of disability, and in 35–50% of patients, according to literature data, to the frequent development of recurrent and chronic forms [1, 4, 5, 8, 9] . The consequence of this may be the occurrence of persistent functional disorders, which significantly limit physical activity, including ability to work, and have a negative impact on the quality of life of patients. A prerequisite for effective treatment of bursitis is the elimination of stress on the affected area. The nature of the load limitation depends on the severity of the disease and the location of the affected area. Traditionally, treatment of bursitis begins with the prescription of nonsteroidal anti-inflammatory drugs (NSAIDs) (Fig. 1). NSAIDs are included in the program of pathogenetic therapy of bursitis as one of the main components.
The mechanism of anti-inflammatory action of non-steroidal drugs is the same for all drugs in this group, based on inhibition of the synthesis of inflammatory mediators - prostaglandins due to inhibition of the activity of the enzyme cyclooxygenase (COX) [2, 8, 9]. Given the variety of existing drugs, choosing one of them can be difficult and requires attention to each individual case. The selection of NSAIDs is carried out empirically, taking into account the severity of the analgesic and anti-inflammatory effect, duration of action, and individual tolerance of the drug. If there is no effect within 5–7 days, the drug should be replaced with a non-steroidal agent of another chemical group (Table 1) [2].
Despite the variety of drugs, there is no ideal non-steroidal anti-inflammatory drug. Nevertheless, the results of the studies, as well as an assessment of the dynamics of the use of NSAIDs, make it possible to identify certain leaders. One of these drugs from the NSAID group is nimesulide (Nise®). Unlike most NSAIDs, nimesulide selectively inhibits the proinflammatory isoform of COX-2 and does not affect the physiological COX-1 [13]. It is the first selective COX-2 inhibitor synthesized [14]. Another advantage when prescribing nimesulide is its non-acidic origin (in the nimesulide molecule the carboxyl group is replaced by sulfonanilide), which provides additional protection of the gastrointestinal mucosa [14, 15]. The analgesic activity of nimesulide is close to that of indomethacin, diclofenac, and piroxicam. Nimesulide also has a number of pharmacological effects that are independent of COX-2 blockade. In particular, it suppresses the hyperproduction of the main pro-inflammatory cytokines (interleukin-6, TNF-), the phosphodiesterase-4 enzyme and thereby reduces the activity of macrophages and neutrophils, which play a fundamental role in the pathogenesis of the acute inflammatory reaction [14, 15]. According to the statement of the British professor K. Rainsford, “nimesulide is an NSAID that has analgesic, anti-inflammatory and antipyretic effects due to unique chemical and pharmacokinetic properties and has a multifactorial mechanism of action that goes beyond its selective inhibitory activity against the COX-2 enzyme” [16] . To enhance the therapeutic effect and quickly relieve inflammation and pain, it is important to use an integrated approach to treatment. It has been proven that the combined use of Nise tablets and Nise gel enhances the therapeutic effect and promotes rapid relief of pain and inflammation [17]. The base of the Nise gel is represented by isopropyl alcohol, which allows the active substance to quickly penetrate deep into the tissue, directly to the source of inflammation. And after 15 minutes, the medicine is almost completely absorbed from the surface of the skin and concentrated at the site of inflammation. The drug Nise® (nimesulide) is available in two forms - in the form of 100 mg tablets for oral use and in the form of a 1% gel for external local use [18]. Thus, the variety of forms of damage to extra-articular soft tissues, their high prevalence and social significance determine the relevance of the problem of diagnosis and treatment of bursitis. Timely and complete treatment helps to avoid the development of protracted and recurrent forms of the disease. Among the variety of NSAIDs that are the drugs of choice in the treatment of bursitis, nimesulide claims to be one of the first places in terms of treatment effectiveness. The combined use of oral and local forms of NSAIDs improves treatment results for persistent and severe disease.
Causes
There are factors that increase the risk of inflammation:
- Weakened immunity.
- Chronic infections in the body.
- Long-term treatment with antibiotics, corticosteroids and some other drugs.
- Incorrect shoes and poor posture.
- Excess weight.
- Diseases – diabetes, metabolic disorders and others.
- Professional or other activities that involve repetitive movements, pressure or joint injuries. For example, acute prepatellar bursitis (inflammation of one of the bursae of the knee joint) often occurs in those whose working position involves resting on their knees: gardeners, mechanics, plumbers and representatives of other professions. Elbow bursitis often occurs in those who work at a computer, play sports that place stress on the joint (tennis, baseball, weightlifting), or where the risk of falling on the elbow is high (football, basketball, and other sports).
The main causes of acute bursitis:
- Injuries and microtraumas of the joint area.
- Infectious diseases.
- Allergies or autoimmune diseases.
Causes of the disease
Bursitis is usually infectious in nature. It can be caused by untreated inflammatory pathologies. Viruses and bacteria are often the causative agents, leading to the development of sinusitis, otitis, bronchitis, abscess or the formation of another source of infection.
The cause of the onset of the inflammatory process can also be:
- allergic reaction;
- poor circulation in the joint capsule;
- injuries of the synovial bursa or its vessels.
People at risk include people with low or excessive physical activity. In both cases there is an increased risk of injury. Therefore, inflammation of the joint capsule is more common among housewives, office workers, drivers, miners, and professional athletes.
Diagnostics
Acute bursitis is usually visible to the naked eye due to reddened skin and swelling of the joint. For more accurate diagnosis, use:
- Palpation (feeling) of the joint.
- X-ray - the study will show not only inflammation, but also pathologies of bone and cartilage tissue in the joint, salt deposits, thickening of the synovial bursa.
- Ultrasound or MRI - for diagnosing soft tissues.
- Laboratory tests - blood, PCR diagnostics for the analysis of inflammatory pathogens.
Diagnosis of inflammation
The peculiarity of bursitis is that the doctor will be able to determine its type through palpation and a clarifying questioning of the patient. This form of diagnosis is standard.
For an in-depth diagnosis of inflammation, the patient is prescribed an x-ray. With its help, the doctor will be able to study the formation of osteophytes, the condition of the joint, and prescribe effective treatment.
In rare cases, specialists prescribe puncture of the synovial bursa. The method is necessary to diagnose the cause of the disease if the previous examination did not give accurate results.
Treatment
Treatment is carried out by a traumatologist-orthopedist or surgeon (for acute purulent bursitis). In case of acute inflammatory process it is necessary:
- Rest - reduce or completely eliminate movements in the joint, minimize the load. For this, you can use orthoses, bandages and other fixing devices.
- Cold – Periodic cold compresses reduce inflammation.
- Compression – compressing the joint with elastic bandages or other devices reduces pain.
Conservative treatment is used to treat acute elbow bursitis and others:
- Medicines - the doctor will prescribe painkillers, local anti-inflammatory drugs, hormonal agents with anti-inflammatory effects and intra-articular injections.
- Physiotherapeutic procedures - cryotherapy, procedures using electrical currents with different parameters and other procedures. They improve the penetration of drugs into the affected tissues, reduce swelling, improve blood circulation and reduce pain.
The goals of conservative therapy are to stop inflammation, relieve pain, restore joint mobility and prevent complications.
For the purulent form of acute bursitis, conservative therapy is ineffective; surgical treatment is recommended. An opening is performed and the inflamed bursa is drained, the pus is pumped out and the joint cavity is washed with antibiotics and antiseptics. In severe cases, surgery may be performed to remove the bursa.
Treatment of elbow bursitis
First of all, experts recommend limiting physical activity. The affected joint is fixed with special bandages, and in more severe cases, plaster is used. Rest of the elbow joint has a positive effect on its condition.
Severe pain can be neutralized with painkillers. It is recommended to use only those products prescribed by your doctor.
Removal of accumulated fluid from synovial pockets occurs using joint puncture. After this procedure, the bag is washed with antiseptics and antibacterial drugs, which will increase the rehabilitation time after the disease. To more effectively combat elbow bursitis, doctors prescribe immunostimulants, which include vitamin complexes.
In severe cases of the disease, one of the following operations is performed:
- drainage of the synovial sac to remove mucous fluid through the canal;
- removal of the affected area - during the rehabilitation process, a new synovial sac is formed.
In addition, there are other ways to overcome bursitis, for example, with ointments or injections. Experts do not recommend turning to folk remedies. Self-treatment may be ineffective, and in the worst case, lead to serious consequences.
Treatment methods
How to treat this pathology? For this purpose, an integrated approach is used, which is aimed at the following actions:
- Treatment with medications. To eliminate inflammatory processes and pain, the patient should take non-steroidal anti-inflammatory and painkillers. The most effective remedies are: Ibuprofen, Voltaren, Diclofenac and others.
- Application of ointments. Local treatment helps to act directly on the affected area. Thanks to this, the patient can save himself from possible side effects that occur as a result of taking medications internally. Ointments relieve a person from pain and inflammation. For this purpose, the following medications are used: Diclak Gel, Voltaren Gel, etc.
- Physiotherapeutic procedures. They help strengthen muscle tissue and also help restore mobility to sore joints. For these purposes, the following procedures are used: massage, electrophoresis using Dimexide, cryotherapy, etc.
- Physiotherapy. Specially designed exercises gradually restore the mobility of the affected joints and also help eliminate discomfort.
If the above methods do not bring the expected result, then the patient is recommended to have surgery. The essence of the operation is to excise the damaged parts of the subcutaneous heel bursa. It is prescribed only for advanced forms of the disease and helps to restore motor activity to the patient.
Treatment with folk remedies
Medicines to relieve pain and relieve inflammation can be prepared independently at home. To do this, you should turn to alternative medicine recipes. Let's look at the most effective home remedies.
Linen
To prepare a warming agent you will need 2 tbsp. l. flax seeds, which need to be heated in a frying pan. Place them in a small bag made of natural fabric. Apply to problem areas until cool. The duration of such treatment is usually about 2 weeks.
Apple cider vinegar and honey
You will need apple cider vinegar and honey in equal quantities. The ingredients should be mixed thoroughly. 1 tsp. Dilute the finished medicine in 1 glass of water. Take this medicine 2 times a day. The duration of use of this product should be no more than 1 week.
White cabbage
For an analgesic and anti-inflammatory compress, take a few cabbage leaves and beat them a little until the juice appears. These leaves should be applied to the sore heel, secured with a bandage and wrapped in a warm ball. Keep the compress on all night.
It is also useful to apply cold and heat when subcutaneous heel bursitis appears. Achilles bursitis can be treated with celery infusion and grapefruit juice, which should be taken orally.
The variety of treatment methods allows you to choose the most effective methods, taking into account the individual characteristics of the course of the disease of each patient. If you follow the recommendations of your doctor, you can get rid of bursitis in the heel within 2 weeks.
httpv://www.youtube.com/watch?v=embed/R-FDNQ82GJg
Appendix B: Patient Information
The elbow joint has a complex structure and is classified as a trochlear joint. A common pathology is considered to be bursitis of the elbow joint - inflammation of one of the periarticular bursae - bursa (interosseous ulnar, radiobrachial, subcutaneous ulnar). In a healthy person, the cavities of the bursae contain a small amount of synovial fluid, which is necessary to reduce the friction of the cartilaginous surfaces of the joints of the bones and provide nutrition to the cartilage. With bursitis, the amount of this fluid increases as inflammation and swelling of the inner (synovial) membrane develops, pain and other symptoms occur. Treatment of elbow bursitis in the acute phase is more successful than treatment of the chronic process, so it is not recommended to delay visiting a specialist.
Therapy for the disease must be comprehensive, and it begins with ensuring rest (immobilization) of the upper limb with a scarf or other immobilization. Immobilization helps reduce swelling and pain. Sometimes, to prevent injury to the elbow joint, it may be necessary to immobilize the limb with a splint. If bursitis is traumatic, apply a cold compress before immobilizing the limb.
Modern methods of treating acute bursitis include intra-articular injections with glucocorticosteroids (Betamethasone, Hydrocortisone**). This is done to prevent relapses of the disease and quickly relieve pain, reduce swelling of the synovial membrane of the bursa. The procedure is performed only in a medical institution, since failure to comply with the rules of aseptic and antiseptic treatment can lead to infection and the development of purulent bursitis.
Among the medications for bursitis of the elbow joint are prescribed:
- Non-steroidal anti-inflammatory drugs for rapid relief of inflammation and for analgesic purposes.
- Preparations with chondroprotectors for the restoration of joint tissue.
- Antibiotics for infectious inflammation of the periarticular bursa.
Local therapy
In addition to the injection of drugs into the joint and systemic drugs, the doctor recommends the use of local agents. They will not only relieve pain faster, but also accelerate tissue regeneration and reduce swelling and inflammation. These include:
- Compresses with dimexide, which have a strong absorbable effect.
- Ointments with chondroitin sulfate, glucosamine, and collagen.
- Ointments with non-steroidal anti-inflammatory components.
Physiotherapy and exercise therapy
In the subacute period, during the chronic course of the process, physiotherapy sessions are required, which effectively relieve local symptoms of bursitis. The following physiotechniques are used:
- Ultrasound
- Microcurrents
- Electro-, phonophoresis
- UHF
- Dry heat
- Balneotherapy
- Paraffin therapy
In cases of tissue necrosis or atrophy, which often accompany chronic bursitis, as well as in cases of purulent inflammation of the bursa, surgical intervention is most often required - excision of the bursa. With frequent exacerbations of bursitis, part of the joint capsule or all of its tissue is removed, a splint is applied, and then a set of rehabilitation measures is carried out.
Diagnosis of elbow bursitis
If you have the symptoms described above, you should contact a surgeon, traumatologist or orthopedist.
Diagnosis of inflammation of the subcutaneous ulnar bursa is not difficult. If infected bursitis is suspected, a puncture is performed followed by examination of the material. The sensitivity of detected pathogens to antibiotics is checked.
Due to the special location of the interosseous and radioulnar synovial bursae, they are examined using MRI. If necessary, the patient is referred for consultation to a rheumatologist.