Osteoarthritis is a chronic, non-inflammatory disease of the joints or articular cartilage and the tissues that surround them. Osteoarthritis is one of the most common diseases, affecting 10-14% of the world's population. This disease mainly affects women aged 45 to 55 years. Osteoarthritis is the most common joint disease and accounts for almost 80% of all joint etiologies. The etiology of this disease is currently unknown . All factors that cause tissue degeneration and aging of the body can lead to the occurrence of this disease, therefore, with age, the appearance of osteoarthritis is almost inevitable.
There are external and internal factors for the occurrence of this disease. The main external factors of osteoarthritis include dampness, hypothermia, unfavorable working conditions, functional overload of joints with frequent microtraumas, as well as exposure to radiation energy and vibration. The main and fairly common cause of osteoarthritis is the inability of cartilage to resist increased stress on the joints. The reasons for this manifestation may be poor posture, prolonged work while standing, and even certain sports: weight lifting, running or jumping.
The internal factors that cause this disease include the following: hereditary predisposition to the occurrence of diseases of cartilage tissue, impaired blood supply to the joint, hormonal imbalance and metabolic disorders. The cause of osteoarthritis in women may be ovarian dysfunction during menopause. In addition, vascular processes with the early development of atherosclerosis may also be the cause of this disease. Osteoarthritis also develops secondary to diseases such as congenital dislocation, rheumatoid arthritis, intra-articular fractures, and even alcoholism.
general information
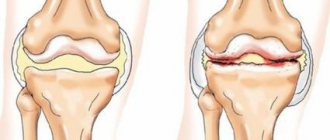
Osteoarthritis begins with microdamage to cartilage against a background of increased load or reduced ability to regenerate. As a result, the tissue becomes thinner and becomes denser and less smooth. The movement of bones relative to each other becomes difficult, and certain areas of the articular surfaces begin to experience constant overload.
The process is accompanied by a change in the properties of the synovial fluid, which becomes thicker. Bone growths – osteophytes – appear inside the joint cavity. As the disease progresses, their number increases and the distance between the bones decreases. The pathological process spreads to surrounding tissues: ligaments, muscles. Ultimately, all elements of the joint grow together, and movement is completely blocked.
Make an appointment
Pathophysiology of OA
Vascularization of cartilage is a feature of the development of osteoarthritis. Blood vessels grow into the cartilaginous continuation of the articular surface, and ossification of the articular capsule begins from the subchondral zone
Primary and secondary OA have a common pathological basis. OA was previously thought to be a degenerative disorder resulting from the biochemical breakdown of hyaline cartilage in synovial joints. However, today a slightly different point of view is accepted, which suggests that not only the articular cartilage suffers, but also the entire joint, including the subchondral bone, synovial membrane and nearby tissues.
Despite the degenerative nature of OA, there is increasing evidence that after the synthesis of cytokines by chondrocytes and the release of cytokines into the joint cavity, an inflammatory process develops. Proinflammatory mediators (cytokines interleukin-1 and tumor necrosis factor) are not involved in matrix degradation [2], but activate chondrocytes in the superficial layer of cartilage, which increases the synthesis of matrix metalloproteinases and, consequently, degeneration of articular cartilage.
In the initial stage of OA, due to increased synthesis of proteoglycans, the main component of the matrix, swelling of the cartilage occurs. This stage can last several years or even decades, and its main manifestation is hypertrophy of the articular cartilage.
Further, as OA progresses, the level of proteoglycans decreases to extremely low values, and their qualitative composition changes. Damaged cartilage is subject to overload, as a result of which the synthesis of metalloproteinases (collagenase, stromelysin and others) increases. They contribute to the further destruction of proteoglycans and the entire collagen network, which determines the progressive degeneration of cartilage. As a result, the cartilage softens and loses its elasticity and becomes increasingly damaged. Microscopically, peeling and vertical clefts are noticeable on the smooth surface of the articular cartilage at this stage of the disease.
OA is characterized by vascularization of cartilage and changes in the subchondral bone. An actively mineralizing osteoid is formed in it, and then subchondral cysts and microfractures form. This leads to the development of subchondral sclerosis.
Kinds
Most often, the disease is classified depending on the location of the pathological process. Osteoarthritis can be unilateral or bilateral and deform almost any joint:
- knee;
- hip;
- ankle;
- brachial;
- temporomandibular;
- elbow;
- small joints of the foot and hand;
- intervertebral joints.
Depending on the cause, osteoarthritis can be primary (occurs on its own) or secondary (develops against the background of another pathology or injury).
Concept and classification of osteoarthritis
Osteoarthritis predominantly affects weight-bearing joints: knees, hips, shoulders and lumbosacral joints.
A 2011 comparative study found that the topical analgesic capsaicin was 50% more effective as a pain reliever for OA than placebo. An inhibitor of neuronal reuptake of serotonin and norepinephrine, a third-generation antidepressant, duloxetine is more effective than placebo in relieving pain in OA. OA is a heterogeneous group of conditions with different etiologies and similar biological, morphological and clinical manifestations. OA primarily affects weight-bearing joints: knees, hips, shoulders, and lumbosacral joints. The distal and proximal interphalangeal joints and metacarpal joints may be affected, but such localization is much less common. Daily loads, which are mostly placed on weight-bearing joints, play an important role in the development of the disease.
Primary, or idiopathic, is osteoarthritis, the cause of which remains unknown. It can be local (one or two joints are affected) or generalized (three or more joints are affected). Local OA is most often associated with damage to the knee joints (gonarthrosis) and hip joints (coxarthrosis). In secondary OA, there is an obvious cause of the disease: trauma, metabolic disorders, a history of other rheumatological diseases, and so on.
Causes
The development of osteoarthritis can be triggered by any disease or condition that increases the load on the joint or worsens its regeneration processes. Most often, pathology occurs against the background of:
- joint injury or surgery;
- past inflammatory process;
- excess body weight;
- regular excessive physical activity (standing work, professional sports, heavy lifting);
- hormonal shocks (pregnancy, menopause);
- congenital pathologies of the musculoskeletal system (flat feet, congenital hip dislocation, etc.);
- autoimmune diseases (systemic lupus erythematosus, rheumatoid arthritis);
- connective tissue dysplasia (a condition in which its structure changes);
- endocrine diseases and metabolic disorders (diabetes mellitus, gout);
- vascular diseases (atherosclerosis, thrombophlebitis, etc.).
Heredity, as well as age over 45 years, significantly increases the risk of developing osteoarthritis.
Degrees
Orthopedists distinguish 4 degrees of the disease:
- Grade 1: there are no symptoms, but with exertion a person may notice slight pain or discomfort; all cartilage damage occurs at the microscopic level;
- 2nd degree: pain occurs not only during exercise, but also at rest; x-rays reveal a narrowing of the joint space and isolated bone growths;
- 3rd degree: destruction reaches its peak, surrounding tissues are involved in the pathological process; the pain becomes constant, and the pictures clearly show deformation, narrowing of the joint space and numerous osteophytes; Often at this stage, dislocations and subluxations of the joint occur due to weakening of the ligaments;
- 4th degree: bone growths completely block the joint, movement is impossible.
Symptoms
The main signs of osteoarthritis develop gradually, intensifying as the disease progresses. Most patients note:
- pain: associated with friction of the articular surfaces of bones from each other, intensity and duration depend on the stage;
- crunching when moving: is one of the first signs of the disease, as it progresses it is accompanied by pain;
- stiffness: as the cartilage is destroyed and osteophytes appear, the range of motion of the joint is reduced until complete blocking (ankylosis);
- joint deformation due to bone growths;
- changes in surrounding tissues: especially noticeable when affecting the limbs and fingers, which appear noticeably curved.
Damage to large joints significantly changes a person’s lifestyle, as he loses the ability to move independently and take care of himself.
Osteoarthritis - modern approaches to diagnosis and treatment
ABOUT
Steoarthrosis (OA) is a chronic progressive joint disease characterized by primary degeneration of articular cartilage followed by changes in subchondral bone and the development of marginal osteophytes and accompanied by reactive synovitis. Another name for the disease, “osteoarthritis,” is also widely used due to the frequent identification of accompanying signs of inflammation. Osteoarthritis is the most common joint disease, affecting both men and women; most often develops in men under the age of 45 and in women over the age of 55. The prevalence of osteoarthritis is the same in people of both sexes over 70 years of age and occurs in almost everyone.
Factors contributing to the development of OA
1. Chronic microtraumatization of cartilage.
2. Age of patients.
3. Obesity.
4. Load on joints.
5. Congenital or acquired defects of the musculoskeletal system.
6. Hereditary predisposition (Heberden's nodes occur 2 times more often in mothers and 3 times more often in sisters of a patient with OA).
There are primary and secondary OA. Primary (idiopathic) OA
develops in peripheral joints, most often in the distal and proximal interphalangeal joints of the hands (with the formation of Heberden's and Bouchard's nodes), 1st carpometacarpal, 1st metatarsophalangeal, hip and knee joints, intervertebral discs and joints of the spine, especially the cervical and lumbar regions.
Depending on the prevalence of the process, there are 2 forms of primary OA:
— local
the form is characterized by damage to one or two joints (OA of the joints of the hands, feet, knee, hip joints, OA of the spine);
- for generalized
forms are characterized by damage to 3 or more joints or a group of joints (proximal interphalangeal joints are assessed as one group, and distal interphalangeal joints as another).
Secondary OA
develops as a result of trauma, congenital dysplasia of the musculoskeletal system, endocrine diseases (acromegaly, hyperparathyroidism), metabolic disorders (ochronosis, hemochromatosis, gout) and other diseases of bones and joints (rheumatoid arthritis, infectious arthritis, aseptic bone necrosis).
Leading pathogenetic factors
with OA are
degeneration and destruction of articular cartilage
, developing as a result of a discrepancy between the mechanical load on the articular surface of the cartilage and its ability to resist this load. Changes in articular cartilage can be caused by both congenital and acquired internal factors, and external environmental influences. The most pronounced pathomorphological changes in arthrosis occur in the cartilage matrix. They lead to the development of progressive erosion of cartilage and destruction of type II collagen fibers, as well as degradation of proteoglycan macromolecules. Disorders of cartilage metabolism are based on quantitative and qualitative changes in proteoglycans—protein-polysaccharide complexes that ensure the stability of the structure of the collagen network, which is the basis of the cartilage matrix. Cartilage damage during arthrosis is the result of increased synthesis and release of collagenase and stromelysin (metalloproteases) from chondrocytes, which destroy proteoglycans and the collagen network. An increase in the synthesis of collagenase and stromelysin in the affected cartilage, which can be genetically determined and is under the control of cytokines released from the synovial membrane, leads to further degradation of the cartilage matrix.
Inflammation in the joint is also associated with the level of cytokines, which are often found in the synovial fluid of patients with arthrosis. Cytokines, in particular interleukin-I, stimulate chondrocytes and lead to an increase in the synthesis of metallo- and serine proteases. In addition, cytokines can inhibit the synthesis of the most physiological enzyme inhibitors and block the synthesis of the main matrix elements - collagen and proteoglycans. A decrease in the level of inhibitors and an increase in enzymes leads to an increase in the activity of the amount of proteases, which, in combination with inhibition of matrix synthesis, leads to cartilage degeneration and the development of arthrosis.
Pathological anatomy
. Cartilage changes from strong, elastic and blue to dry, yellow, dull with a rough surface. At the early stage of OA, as a rule, local zones of softening of the cartilage form in places of maximum load; at later stages, fragmentation occurs and vertical cracks form in it. In places the cartilage becomes calcified. Cracking of the cartilage leads to ulceration, exposing the underlying bone and releasing fragments that enter the joint cavity as detritus. When the cartilage cover is thinned, the pressure distribution between the articular surfaces becomes uneven. This leads to local overloads and increased friction between the articular surfaces.
In recent years, the concept of viscoelastic joint protection
: the elastic-viscous properties of synovial fluid depend on the content of hyaluronan in it. The ability to absorb water and retain it is determined by the main property of the hyaluronic molecule. The physiological role of hyaluronan is to provide protection, lubrication and mechanical stabilization of the collagen network and cells in and on the joint tissues. With arthrosis in the joint, rheological homeostasis is disrupted, which is associated with the viscoelastic properties of the joint environment and provides the conditions for its normal functioning.
Clinic and diagnosis of osteoarthritis
The main clinical manifestations of OA are pain, deformity and joint stiffness. The cardinal clinical symptom of OA is pain in the affected joints. The pain is heterogeneous and has a variety of mechanisms of occurrence.
Types of pain in osteoarthritis
1. "Mechanical" type
characterized by the onset of pain under the influence of daytime physical activity and subsidence during the period of night rest, which is associated with a decrease in the shock-absorbing abilities of the cartilage and bone subchondral structures. This is the most common type of pain in OA.
2. Continuous dull pain at night
more often in the first half of the night they are associated with venous stasis in the subchondral spongy part of the bone and an increase in intraosseous pressure.
3. "Starting pains"
short-term (15-20 minutes), occur after periods of rest and disappear against the background of physical activity. “Starting pains” are caused by friction of the articular surfaces on which detritus settles - fragments of cartilaginous and bone destruction. During the first movements in the joint, detritus is pushed into the inversions of the joint capsule (“articular mouse”).
4. Constant pain
are caused by a reflex spasm of nearby muscles, as well as the development of reactive synovitis.
In the presence of synovitis, in addition to pain in the joint both during movement and at rest, morning stiffness, swelling of the joint, and a local increase in skin temperature are characteristic. As the disease progresses, relapses of synovitis become more frequent. Deformation and stiffness of the joints gradually develop due to the development of fibrosclerotic and hypotrophic changes in the periarticular tissues. At the early stage of OA, joint dysfunction is caused by pain and reflex muscle spasm. As the disease progresses, a decrease in range of motion is affected by tendon-muscular contractures, osteophytes, and disruption of the congruence of articular surfaces.
The clinical picture of OA is determined by the specific joint involved in the pathological process. The most significant and disabling forms of OA are gonarthrosis and coxarthrosis.
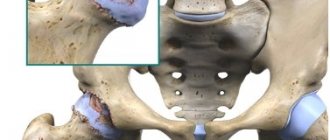
Coxarthrosis
- the most common and severe form of OA, which usually ends in progressive impairment of joint function up to its complete loss. The main symptoms of coxarthrosis are mechanical pain in the hip joint, often accompanied by limping.
To make a diagnosis of hip OA, according to the American College of Rheumatology (ACR) criteria, the presence of pain in the hip joint and two of the following three signs is necessary:
— ESR<20 mm/h;
— X-ray detected osteophytes of the femoral head or acetabulum;
— X-ray detected narrowing of the joint space (in the upper, axial and/or medial part).
Gonarthrosis
- the second most common localization of deforming OA. The main symptom is mechanical pain that occurs when walking and especially when going up or down stairs. The pain is localized in the front or inner parts of the joint and can radiate to the lower leg.
The M. Lequene criteria are used as diagnostic criteria for osteoarthritis of the knee joint, which best reflect the clinical understanding of this disease (Table 1).
The diagnosis is established in the presence of all three signs and the exclusion of the following diseases: ischemic bone necrosis, Paget's disease of bone, chondrocalcinosis (pyrophosphate arthropathy), hemochromatosis, ochronosis, hemophilia, arthritis, joint infections (including tuberculosis), Charcot's joint (neuroarthropathy), pigmentary villonodular synovitis, chondromatosis.
Damage to the distal interphalangeal joints of the hand ( Heberden's nodes
) is the third characteristic localization of osteoarthritis.
Dense, pea-sized, sometimes painful on palpation, usually multiple nodules are more common in menopausal women on the fingers. They are caused by bone marginal osteophytes. In 50% of patients with Heberden's nodes, a similar lesion of the proximal interphalangeal joints is observed - Bouchard's nodes
. They are located on the lateral surface of the joint, causing the finger to acquire a spindle-shaped shape.
For the diagnosis of OA of the hand joints, the AKR criteria are also widely used (Table 2).
The second and third distal interphalangeal joints, the second and third proximal interphalangeal joints and the first metacarpophalangeal joints of both hands are taken into account.
Polyosteoarthrosis
- a common variant of OA with multiple lesions of peripheral and intervertebral joints. Polyosteoarthrosis can be primary or secondary. Secondary polyosteoarthrosis occurs in patients with metabolic polyarthritis - gout, pyrophosphate arthropathy, ochronosis.
Primary polyosteoarthrosis was described in 1952 by English scientists J. Kellgren and R. Moore under the name “generalized osteoarthritis.” This disease is often referred to as Kellgren's disease - multiple lesions of the peripheral and intervertebral joints, that is, a systemic degenerative lesion of the musculoskeletal system.
The most significant in diagnosing OA is x-ray examination.
musculoskeletal system. Currently allocated
- mandatory radiological symptoms:
1) narrowing of the R-articular space;2) osteophytes;
3) subchondral osteosclerosis
- optional radiological symptoms:
1) periarticular marginal bone defect;2) subchondral cysts;
3) intra-articular calcified chondromas.
arthroscopy
has become increasingly important in recent years , which allows a detailed study of the surface morphology of cartilage and clarify the diagnosis using targeted biopsy.
Magnetic resonance imaging (MRI)
is one of the most modern research methods. This technique has a whole range of advantages: good contrast of soft tissues, free choice of image plane, three-dimensional nature of the information obtained, absence of radiation exposure and artifacts from bone structures and air. MRI provides contrast in the image of the cartilage layer, allows you to identify surface changes of various sizes and abnormalities in metabolism.
Treatment of osteoarthritis
Therapeutic tactics for OA consists of three components:
1. Mechanical unloading of affected joints
2. Relief of synovitis
3. Prevention of disease progression.
Drug treatment
is aimed at relieving synovitis and pain, improving intraosseous and regional blood flow, stimulating metabolic processes in the body.
Currently, in the treatment of OA, two classes of drugs are distinguished according to their pharmacological action.
Class I includes immediate-acting symptomatic drugs, that is, analgesics and nonsteroidal anti-inflammatory drugs (NSAIDs), which can reduce pain, swelling, stiffness and improve joint function. Class II is a group of drugs that modify the structure of the joint and can prevent the progression of the disease.
NSAIDs are the most commonly used drugs for OA.
. They have anti-inflammatory, analgesic and antipyretic effects, which help reduce pain and improve joint function.
The anti-inflammatory and analgesic activity of NSAIDs is associated with a decrease in the production of prostaglandins. NSAIDs have also been shown to inhibit the formation of prostacyclin and thromboxane, exerting a complex effect on vascular permeability and platelet aggregation. The anti-inflammatory effect of NSAIDs is due to inhibition of cyclooxygenase activity
(COX) is the main enzyme in the metabolism of arachidonic acid on the path of its conversion into prostaglandins.
There are at least two isoforms of COX. And although their amino acid sequence is 60% identical, they are the product of two different genes. COX-1
regulates normal cellular processes and is stimulated by hormones or growth factors.
COX-1 is expressed on most tissues of the body and is inhibited to varying degrees by all NSAIDs, so many adverse reactions from the gastrointestinal tract are explained by this inhibition. Another isoform, COX-2
, which is usually not detected in tissues, is expressed during inflammation and is also inhibited by all existing NSAIDs to a greater or lesser extent, as well as by glucocorticosteroids, which distinguishes it from COX-1.
At the same time, evidence is accumulating that the anti-inflammatory and analgesic effects of NSAIDs are explained not only by the suppression of COX. It is assumed that NSAIDs inhibit the activation and chemotaxis of neutrophils and reduce the production of toxic oxygen radicals in stimulated neutrophils, inhibit the activity of the transcription factor NF-kB, inhibiting the stimulation of nitric oxide synthetase.
The study of the mechanisms of action led to the creation of a new classification of NSAIDs (Table 3), based on the selectivity of action against COX, allowing the doctor to individually select the most effective and safe drug.
The “gold standard” among NSAIDs when assessing the analgesic and anti-inflammatory effect is diclofenac sodium.
Diclofenac ( Voltaren
) differs favorably from other NSAIDs in that it is available in various dosage forms: tablets, injections, suppositories, and also for local therapy - in the form of a gel.
For oral administration, diclofenac is available in the form of tablets 25-100 mg, incl. coated (film, enteric), regular and delayed (retarded) release, the latter provides a longer effect of the drug. For parenteral administration, use a 2.5% solution in a 3 ml ampoule (75 mg of active substance). The doctor has diclofenac at his disposal ( Voltaren
) for rectal administration - suppositories of 50 and 100 mg, and for children - 25 mg.
Systemic administration of diclofenac can be limited using forms for local use: 1.5% gel, 1.2% ointment, 1% emulgel. This method of treatment is also successfully used to relieve joint pain due to osteoarthritis.
Recommended daily doses are 75-150 mg in 2-3 doses. Treatment should begin with the minimum effective dose. Daily fluctuations in the symptoms of the disease require clarification of the timing of admission. Synchronization of prescription of diclofenac ( Voltaren
) allows you to increase efficiency and reduce the number of side effects, especially when taking short-lived NSAIDs, such as diclofenac. It should be remembered that the analgesic and anti-inflammatory activity of the drug does not always correspond to the same dose. As a rule, the analgesic effect is achieved with a lower concentration of the drug.
For long-term therapy, it is usually sufficient to prescribe 1 tablet of Voltaren retard, 100 mg per day. In cases where the pain is most pronounced at night or in the morning, it is recommended to give preference to taking Voltaren retard 100 mg in the evening.
Along with the widespread use of group I drugs, agents are currently being created that can slow down the progression of OA. These drugs are called structure-modifying drugs, their role is to prevent, slow down, stabilize or reverse the osteoarthritic process not only in the cartilage, but throughout the entire joint. Evidence has been obtained that these drugs stimulate the synthesis of hyaluronic acid and proteoglycans and inhibit the action of proteolytic enzymes, thereby enhancing anabolic processes in cartilage and suppressing catabolic ones, which underlies their structure-modifying effect. There is evidence of their ability to suppress the formation of superoxide radicals and the synthesis of nitric oxide, which apparently determines their analgesic effect.
Table 4 presents the main directions of complex therapy for OA.
For painful muscle spasms, including after surgery for osteoarthritis of the hip joint,
Sirdalud
(tizanidine) is used. The drug is effective for moderate to severe pain, especially when the pain intensifies during the night.
Sirdalud has a dual mechanism of action - muscle relaxant and analgesic [3]: the analgesic effect of the drug is associated not only with its muscle relaxant properties, but also with a direct effect on the pain-transmitting structures of the central nervous system. Thus, Sirdalud is able to effectively break the vicious circle of “pain-muscle spasm-pain”.
Sirdalud is characterized by a rapid onset of a positive therapeutic effect and good tolerability. Selection of an individually effective dose (from 2 to 6 mg/day) is usually carried out within 2-4 weeks. Clinically significant improvement is usually observed within the first 2-3 weeks from the start of therapy. Sirdalud is usually prescribed in combination with non-steroidal anti-inflammatory drugs, since their effect is synergistic. It is believed that Sirdalud, acting through central α-adrenergic pathways, inhibits the production of gastric secretions and prevents aspirin-induced changes in glycoproteins and damage to the gastric mucosa, while reducing the risk of ulcer formation [9,10]. Thus, Sirdalud is able to prevent damage to the gastric mucosa caused by non-steroidal anti-inflammatory drugs [4, 9-12].
The mechanism of action of Sirdalud is significantly different from the mechanisms of action of other drugs used to reduce increased muscle tone [1, 2]. Therefore, Sirdalud is used in situations where there is no antispastic effect of other antispastic drugs (in so-called cases that do not respond to treatment). The advantage of Sirdalud compared to other muscle relaxant drugs that are used for the same indications is that when muscle tone decreases when Sirdalud is prescribed, there is no decrease in muscle strength [1,2].
The duration of therapy with Sirdalud is determined only by the clinical situation.
Important role in prevention
OA plays a role in the identification and timely orthopedic correction of congenital anomalies of the musculoskeletal system. It is necessary to exclude long-term static and mechanical overloads of the joints. An essential condition for the prevention of knee OA is the normalization of excess body weight.
Due to the possibility of disability due to OA, patients with OA with damage to large joints, mainly knees and hips, are subject to dynamic observation, starting from the early stages of the disease.
In case of severe joint deformities, the issue of arthroplasty or endoprosthetics is decided. Literature:
1. Coward DM Pharmacology and mechanisms of action of tizanidine (Sirdalud). /In: Spasticity: The current status of research and treatment. Ed. by M. Emre, R. Benecke. -Carnforth etc.: The Parthenon Publishing Group, 1989. -P.131-140
2. Coward DM Tizanidine: Neuropharmacology and mechanism of action. //Neurology. -1994. -Vol.44., N.11 (Suppl.9). -P.S6-S11
3. Davies J., Quinlan JE Selective inhibition of responses of feline dorsal horn neurons to noxious cutaneous stimuli by tizanidine (DS103-282) and noradrenaline: Involvement of alpha2-adrenoceptors. //Neurosci. -1985. -Vol.16. -P.673-676
4. Berry H., Hutchinson DR A multicentral placebo-controlled study in general practice to evaluate the efficacy and safety of tizanidine in acute low-back pain. //J. Intern. Med. Res. -1988. -Vol.16. -P.75-82
5. Lepisto P. A comparative trial of tizanidine and placebo in patients with skeletal-muscle spasms after surgery for herniated disk. //Curr. Therap. Res. -1981. -Vol.30. -P.141-146
6. Abud MC, Fernandez GJA, Ochoa CH et al. Evaluacion de la eficacia y tolerancia de tizanidina en lumbalgia aguda. //Investig. Med. Internac. -1992. -Vol.19. -P.110-114
7. Benecke R. Clinical experience with antispastic drugs. /In: The origin and treatment of spasticity. Ed. by R. Benecke et al. -Carnforth etc.: The Parthenon Publishing Group, 1990. -P.103-112
8. Roberts RC, Part NJ, Pokorny R. et al. Pharmacokinetics and pharmacodynamics of tizanidine. //Neurology. -1994. -Vol.44., N.11 (Suppl.9). -P.S29-S31
9. Maeda-Hagiwara M., Watanabe H., Kanaoka R., Watanabe K. Reduction of centrally-stimulated gastric acid secretion by tizanidine, a new imidazoline derivative, in anesthetized rats. //Arch. Int. Pharmacodyn. -1985. -Vol.277. -P.321-327
10. Maeda-Hagiwara M., Watanabe H., Kanaoka R., Watanabe K. Influence of clonidine and a new related imidazoline derivative (tizanidine) on rat gastric mucosa. //Pharmacology. -1986. -Vol.32. -P.109-113
11. Berry H., Hutchinson DR Tizanidine and ibuprofen in acute low-back pain: Results of a double-blind multicentre study in general practice. //J. Intern. Med. Res. -1988. -Vol.16. -P.83-91
12. Hutchinson DR Muscle relaxants: a role of in the treatment of acute low back pain. //In: Back pain, painful syndromes and muscle spasms (Current concepts and recent advances). Ed. by MI Jayson et al. -Carnforth etc.: The Parthenon Publishing Group, 1990. -P.117-128
13. Fogelholm R., Murros K. Tizanidine in chronic tension-type headache: a placebo controlled double-blind cross-over study. //Headache. -1992. -Vol.32. -P.509-513
14. Shimomura T., Awaki E., Kowa H., Takahashi K. Treatment of tension-type headache with tizanidine hydrochloride: Its efficacy and relationship to the plasma MHPG concentration. //Headache. -1991. -Vol.31. -P.601-604
15. Chantraine A. Management of spasticity in hemiplegia. //In: Motor disturbances I. Ed. by R. Benecke et al. -London etc.: Academic Press, 1987. -P.187-195
16. Lee HK, Jahng JS, Kang ES et al. A multicentre study to evaluate the efficacy and tolerability of tizanidine in the treatment of acute painful muscle spasms in Korea. //Brit. J. Clin. Res. -1990. -Vol.1. -P.23-32
Diagnostics
If you have problems with your joints, you should seek help from an orthopedist-traumatologist. Its tasks include identifying the symptoms of osteoarthritis, determining the extent of the disease and selecting treatment.
Radiography remains the main way to visualize changes occurring inside the joint. The image allows you to see the size of the joint space, the number and size of osteophytes, and bone deformation. If it is necessary to visualize soft tissues, ultrasound or MRI is performed. According to indications, arthroscopy is performed: a puncture of the joint capsule, followed by the introduction of a miniature camera into the cavity, allowing one to see the joint from the inside. This technique can be supplemented by the administration of drugs.
Laboratory diagnostics are of an auxiliary nature. A general blood test can show an active inflammatory process if arthritis has joined osteoarthritis. If the disease is secondary in nature, tests, examinations and consultations with specialists are prescribed to diagnose the original pathology.
Treatment of osteoarthritis
Treating osteoarthritis of the joints takes time and patience. At an early stage, doctors successfully stop the pathological process with the help of medications and physiotherapy, but in advanced cases the disease can only be dealt with surgically. All treatment methods are divided into:
- medicinal;
- non-medicinal;
- surgical.
Drug treatment is aimed at reducing pain and restoring cartilage tissue. Pain due to osteoarthritis significantly reduces the patient’s quality of life, making it difficult to move freely, which is why analgesics and anti-inflammatory drugs are at the top of the list of prescriptions. Depending on the clinical situation, drugs from the following groups are prescribed:
- NSAIDs (non-steroidal anti-inflammatory drugs): stop inflammation and reduce pain;
- corticosteroids: hormonal drugs that block inflammation;
- antispasmodics: relieve reflex muscle spasms.
Preparations of these groups are available in the form of ointments for topical use, tablets and capsules, suppositories or solutions for injections. Some are injected directly into the joint cavity, acting as efficiently as possible. The dose, duration and frequency of administration are selected only by a doctor, since long-term use can accelerate the destruction of joints.
The second group of drugs is aimed at restoring or slowing down the destruction of cartilage. The debate about the effectiveness of chondroprotectors is still not over, but at the moment their use is mandatory. Preparations based on chondroitin, glucosamine or their combination are used in long courses of 3-6 months.
In addition to basic therapy, the doctor may prescribe drugs to improve blood circulation and anti-enzyme drugs. Warming ointments have a good effect.
Non-drug treatment methods help enhance the effect of drugs. They are aimed at improving microcirculation in the affected area, stimulating muscles and reducing stress on the joint. For this purpose the following are used:
- massage;
- physical therapy and mechanotherapy;
- joint traction;
- physiotherapy: shock wave therapy, electrophoresis, ultraphonophoresis, ozone therapy, various applications, etc.
The help of surgeons is necessary in the final stages of the disease, when drugs can no longer stop or slow down the pathological process. The most effective method at the moment is endoprosthetics. The affected joint is removed and replaced with a modern prosthesis that can function for decades. This technique is especially often used to restore knee and hip joints.
In some cases, operations are performed to alleviate the patient's condition:
- corrective osteotomy: excision of part of the bone tissue followed by fixation of the remains at a different angle; allows you to reduce the load on the sore joint;
- arthrodesis: fastening bones together; this completely blocks movement in the joint, but the patient is able to lean on the leg without pain.
Make an appointment
What are the symptoms and clinical signs of this disease?
The manifestation of osteoarthritis is expressed by severe pain and deformation of the joints, which leads to disruption of their functions. This disease most often affects weight-bearing joints (hip and knee joints) and small joints of the hand. The spine is also involved in the process. But most often the knee and hip joints are affected. The most basic symptom of osteoarthritis is severe pain in the affected joints. These pains cause damage to bones, joints or periarticular tissues. Typically, such pain increases with physical activity and decreases with rest. Night pain, swelling of the joint, as well as the appearance of a feeling of “gel viscosity” in the affected joint in the morning - all this indicates the occurrence of osteoarthritis. The intensity of such pain depends on many reasons (atmospheric pressure, air humidity and temperature changes). All these factors begin to influence the pressure in the joint cavity, which causes these pains. The next main symptom of osteoarthritis is the appearance of crunching or creaking in the joints, not only when walking, but even with any movement. The appearance of such a crunch or squeak is associated with a violation of the articular surfaces, which causes a limitation of mobility in this joint. With osteoarthritis, there is an increase in the volume of the joints, which is a consequence of the appearance of swelling of the periarticular tissues. Swelling or fever in the area of the affected joint is extremely rare. Clinical forms of osteoarthritis:
- Gonarthrosis.
- Coxarthrosis.
- Osteoarthritis of the distal interphalangeal joints of the hand.
- Osteoarthrosis of the proximal interphalangeal joints of the hands.
- Spondylosis deformans.
- Intervertebral osteochondrosis.
1. Gonarthrosis is a lesion of the knee joint due to osteoarthritis. In this case, pain in the knee joints is pronounced when walking, and they are especially intense if you go down the stairs. The location of these pains is in the inner and anterior parts of the affected knee joint. Increased discomfort occurs when the knee is bent. In addition, in many cases with gonarthrosis, deviation of the knee joint occurs. The disease begins gradually, and the pain is increasing. A crunching sound may be heard during active and passive movements. The pain begins to intensify, and in many cases synovitis develops - inflammation of the lining of the joint capsule or tendon. 2. Coxarthrosis is a lesion of the hip joint. Initial pain when the hip joint is affected does not appear in the hip area, but in the knee, groin or buttock. They intensify when walking, and subside at rest. These pains, which occur even with minor changes on the x-ray, are associated with muscle spasm. When the hip joint is damaged, there is a gradual increase in limited mobility in the joint. This disease is a consequence of injury or arthritis. With coxarthrosis, there is a gait, developing lameness, wasting of the muscles of the buttock and thigh. There is also pain on palpation in the area of the femoral head. 3. Osteoarthritis of the distal interphalangeal joints of the hand or Heberden's nodes . The appearance of such nodules is most often observed in women during menopause. Initially they appear on the 1st and 3rd fingers of the hand. Over time, namely after several months or even years, symmetrical damage is observed in other distal interphalangeal joints. Such nodules are located on the dorsolateral surface of the joints. 4. Osteoarthritis of the proximal interphalangeal joints of the hands or Bouchard's nodes. Unlike Heberden's nodes, these nodes appear on the lateral surface of the joint, resulting in lateral enlargement of the joint. As a result of this enlargement, the finger acquires a spindle-shaped shape. 5. Spondylosis deformans - as a result of this disease, marginal bone growths appear in the vertebral area. This disease appears at the age of 20. Osteophytes (bone growths) look like swellings - due to compression of blood vessels, swelling appears. As a result, spinal stiffness occurs, and in some cases, neurological disorders occur. 6. Intervertebral osteochondrosis occurs in combination with spinal curvature or spondylosis deformans. With this disease, disc degeneration occurs and the nucleus protrudes in different directions, and this leads to spinal trauma. Osteophytes also grow and the joint surface increases. In this case, the choroid of the joint suffers, resulting in vasculitis - inflammation of the walls of small blood vessels. The pain syndrome is very pronounced and intensifies with physical activity or hypothermia.
There are two main forms of osteoarthritis - primary or idiopathic (the causes of the disease are not clear) and secondary (the disease occurs against the background of other diseases).
Primary osteoarthritis is localized when less than 3 joints are affected. With localized osteoarthritis, the spine, joints of the hands and feet, knee joints, hip joints and other joints are affected. There is also generalized osteoarthritis, when 3 or more joints are affected. In this case, large joints and distal interphalangeal joints are affected. In addition, erosive osteoarthritis also occurs in the generalized form. Secondary osteoarthritis can be post-traumatic. Also, the causes of secondary osteoarthritis can be metabolic diseases such as Gaucher disease, which is a genetic disease; Wilson's disease is a rare form of liver damage in which copper metabolism is impaired; Hemochromatosis or, as this disease is also called, bronze diabetes, or pigmentary cirrhosis, is a hereditary disease in which iron metabolism is disrupted and it accumulates in organs and tissues. Diseases such as diabetes mellitus, hypothyroidism - decreased thyroid function, acromegaly - hyperfunction of growth hormone, can also be causes of osteoarthritis. In addition to the diseases listed above, osteoarthritis can also be caused by calcium deposition disease, neuropathy and many other diseases.
Prevention
Like most diseases, osteoarthritis is much easier to prevent than to cure. Simple rules will help maintain healthy joints and stop the process at an early stage if it has already occurred:
- sufficient physical activity: amateur sports are a good prevention of physical inactivity, help improve microcirculation and form a good muscle frame;
- normalization of body weight: excess weight creates increased stress on the joints, especially the knee, hip and ankle;
- minimizing traumatic factors: vibration, standing work, heavy lifting contribute to the development of joint diseases;
- correct posture and shoes to distribute the load on the joints;
- timely treatment of diseases that can cause secondary osteoarthritis.
Diet
Proper nutrition is not the main factor in the prevention of osteoarthritis, but it will also make its contribution to maintaining healthy joints. Recommended:
- a diet balanced in calories, macro- and micronutrients;
- sufficient amounts of vitamins and minerals;
- exclusion of spicy, canned, excessively fatty foods, alcohol, as well as products with artificial flavors and dyes;
- minimizing fast carbohydrates.
Collagen and omega-3 acids have a good effect on the condition of cartilage, which is why aspic and sea fish and olive oil should always be present in the diet.
Consequences and complications
Without timely treatment, osteoarthritis can cause disability, especially with bilateral damage.
It causes:
- severe joint deformation;
- bone curvature;
- loss of mobility;
- shortening of the limb (with coxarthrosis and gonarthrosis).
When the large joints of the legs are affected, a person’s gait and posture change so much that this inevitably leads to problems with the spine, pain in the neck and lower back.
Generalized osteoarthritis and disability
When deciding on disability, those whose osteoarthritis is rapidly progressing, as confirmed by x-ray, are referred to MSEC for at least 3 years. Moreover, exacerbations occur at least three times a year.
Patients after surgical treatment with disorders that limit their life activities are also referred. As well as those patients who have severe impairments in standing and walking.
Definition of disability groups
- The first disability group is characterized by a complete loss of the ability to move without outside support, the ability to self-care, work, and study.
- The second group of disabilities is characterized by a significant limitation in the ability to move and care for oneself without outside support or auxiliary devices.
- The third disability group is assigned to moderately severe limitations in the ability to move. In order to overcome short distances, considerable effort and long stops are required. As a rule, these are patients with coxarthrosis and gonarthrosis of the 2nd degree.
Unfortunately, this type of arthrosis cannot be cured. However, with competent and timely treatment, good results can be achieved: pain relief, slowing down the progression of pathology, and improving the functionality of diseased joints.
You might be interested in
- Arthrosis of the lower extremities: treatment and exercises
Treatment at the Energy of Health clinic
If you begin to notice a suspicious crunch in your joints, you should not quickly search the Internet for how to treat osteoarthritis with folk remedies. It is better to seek help from professionals from the Energy of Health clinic. We use modern means of cartilage tissue restoration and offer each patient:
- individual selection of a drug regimen;
- constant monitoring and control of treatment effectiveness;
- various physiotherapeutic procedures;
- massage and physical therapy;
- puncture of the joints followed by the administration of painkillers or artificial synovial fluid;
- drug blockades for quick and effective pain relief.
Physiotherapy
This non-drug method is very effective in combating pain and impaired joint mobility.
Properly selected exercises and a responsible attitude towards their regular implementation have a significant therapeutic effect.
The purpose of exercise therapy is:
- strengthening the muscle corset around the affected joint;
- optimization of blood circulation in cartilage and articular surfaces of cartilage;
- development of movements in the affected joint, which reduces the onset of the feeling of “stiffness” in the joint.
Advantages of the clinic
“Health Energy” is a multidisciplinary clinic with modern equipment and experienced staff. We are always aware of new developments in the field of treatment and prevention of diseases and offer our patients not only time-tested methods, but also modern, advanced methods.
Come to us if you need:
- fast and effective diagnostics;
- assistance from experienced doctors;
- an integrated approach to the treatment of diseases;
- comfortable conditions in the clinic;
- affordable prices for all medical services.
Osteoarthritis is a disease that begins gradually, develops slowly, but ultimately often leads to disability. Don’t let it change your life, sign up for a consultation with the orthopedists at Energy of Health.