Bone marrow is an organ located inside the bones and performs the function of hematopoiesis, which is why it is also called red or hematopoietic marrow. Bone marrow edema is a fairly common pathology, in most cases it occurs without pronounced symptoms (or with blurred clinical manifestations) and is detected accidentally during a magnetic resonance scan in connection with other diseases, for example, intervertebral hernia. Most cases of accumulation of inflammatory exudate in the tissues of the bone marrow and cancellous bone occur as a result of various injuries and infectious processes leading to inflammation of the synovial membrane of the spinal joints. Traditional therapy using methods of forced diuresis for such disorders is ineffective, therefore self-medication after confirmed swelling of the hematopoietic brain of the spine is prohibited due to the high risk of complications.
Spinal bone marrow edema: what is it?
What it is?
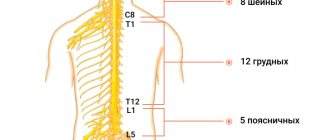
The hematopoietic (bone) marrow is contained in a spongy substance, which is also called trabecular tissue, as it consists of trabeculae (loose bone plates and septa). The largest mass of human bone marrow is located in the bones of the large and small pelvis, skull, and sternum. In the vertebral bodies that make up the human spine, the volume of red medulla is much smaller compared to tubular bones, but despite this, trabecular edema of the spine can cause serious complications, the main of which is the suppression of immune function and the rapid progression of autoimmune diseases (for example , rheumatoid arthritis).
The structure of the bone marrow is determined by its functions, including not only participation in the formation of red blood cells, but also the formation of immune chains when interacting with the lymphoid organs of the peripheral system. The bulk of the mass is fibrous stroma (skeleton). Hematopoietic tissue is represented by five mature sprouts that produce the formed components of blood: erythrocytes, granulocytes (granular leukocytes), lymphocytes, monocytes and megakaryocytes (giant red brain cells).
What cells does bone marrow consist of?
Edema of the hematopoietic brain occurs as a result of excessive accumulation of fluid or inflammatory exudate in the spongy substance of the vertebrae and epiphyses of the pelvic bones and sternum, so the pathology is often referred to as trabecular edema. It manifests itself in the following changes in the osteochondral structure of the vertebra:
- Increased fluid volume in trabecular plates. The normal water content in the bones of the spine is about 10% (the remaining 90% is made up of extracellular matrix and inorganic substances). With swelling, the fluid level can reach 20% (or more).
- Swelling of the vertebral body (caused by an increase in the volume of spongy substance).
- Spread of edema to adjacent tissues (including the subarachnoid space and nervous tissue).
Note! Some traumatologists call bone marrow edema a bone hematoma, but this is not entirely the correct term. A hematoma is an accumulation of blood as a result of damage to small blood vessels and capillaries supplying blood to the vertebrae, and edema is an excessive accumulation of fluid (mainly inflammatory exudate). Despite the fact that the hematoma itself almost always causes swelling of the trabecular substance and bone marrow, pathogenetically these are different pathologies.
Bone structure
Features of the disease in pregnant women and the elderly
Bone marrow cancer is more unfavorable in older people. This is due to the presence of concomitant pathology and the presence of limitations in the use of high-dose chemotherapy, which could potentially lead to stable remission. For example, for myeloma patients over 65 years of age, double stem cell transplantation is not performed due to the high risk of mortality.
As for pregnancy, it is recommended to use reliable contraception for at least 2 years after achieving remission. If the disease was first diagnosed during pregnancy, then the tactics are chosen individually, taking into account the gestational age and type of tumor. For patients in the first trimester of pregnancy, interruption and immediate initiation of chemotherapy are recommended. For indolent forms of leukemia, a wait-and-see approach is possible. Starting from the second trimester of pregnancy, it is possible to carry out chemotherapy treatment with drugs that do not have a negative effect on the fetus. A few weeks before birth, therapy is suspended to allow the bone marrow to recover. The method of delivery is selected based on the obstetric situation.
If bone marrow cancer is diagnosed at the end of the third trimester, early delivery followed by a full course of chemotherapy is possible.
Causes of swelling
The main cause of bone marrow edema (or trabecular edema) is various injuries and injuries to the spine. Such swelling is called primary and occurs as a result of bruises, falls, blows and various injuries to the spine. Hematomas form in the bones of the vertebrae, and blood and lymph leak from damaged vessels, which also put pressure on the trabecular substance. Swelling resulting from injuries is usually localized only in bone tissue, but in some cases it can spread to paravertebral tissues of the spine (musculo-ligamentous apparatus, tendons, synovial membranes of joints).
Secondary edema is not an independent pathology and develops against the background of infectious, inflammatory and degenerative processes in the vertebral bodies and intervertebral discs. To prescribe adequate treatment, correct and extensive diagnosis is of great importance, since therapy for trabecular edema is always selected taking into account the cause of its occurrence. Among them may be:
- Spinal infections (osteomyelitis, spinal tuberculosis, spondylodiscitis, spondylitis). In response to tissue infection, an active release of inflammatory fluid (exudate) occurs, which causes swelling of the vertebrae and their deformation. Particularly dangerous in this regard is hematogenous acute osteomyelitis, in which multiple purulent foci form around the bone marrow and accumulation of purulent exudate occurs.
- Inflammatory processes in the joints of the spine (osteoarthritis). Inflammation of the joints of the spine and their membranes is also accompanied by swelling of the bones and surrounding tissues and can manifest as pain and limited mobility.
- Degenerative-dystrophic diseases. Such pathologies include osteochondrosis, spondylolisthesis, intervertebral hernia, deforming arthrosis, etc.
Damaged and compressed spinal cord from the inside
Note! The likelihood of swelling of the hematopoietic brain increases if a person suffers from diseases of the endocrine system or metabolic disorders, since one of the factors of excess fluid accumulation and accumulation of proteins in the intercellular space is the slow removal of sodium ions from the body.
Causes of spinal cord tumors
The appearance of neoplasms of this type may be preceded by the following risk factors:
- the effects of radiation on the body;
- ultraviolet irradiation;
- poor environmental situation;
- frequent use of a mobile phone;
- being near high-voltage lines;
- exposure to microwave and electromagnetic radiation from household appliances;
- exposure to chemicals or nuclear waste;
- smoking;
- genetic abnormalities;
- consumption of products with nitrates and carcinogens;
- family history of skin, bladder, breast and pancreatic cancer.
The likelihood of developing the disease also increases with age. In addition, doctors identify specific causes of ACM:
- hereditary neurofibromatosis;
- Hippel-Lindau disease.
The appearance of spinal cord tumors, like other types of cancer, is also due to constant stress and lack of emotional balance.
Types of edema and their classification
The classification of bone marrow edema is based on the pathogenetic and etiological mechanism of its occurrence.
Types of red bone marrow edema
| Variety | Cause of occurrence |
| Aseptic | Develops against the background of chronic or pronounced degenerative and dystrophic changes in the vertebrae and intervertebral discs connecting them |
| Traumatic | Occurs as a result of various injuries and damage, as well as exposure to chemical and mechanical factors |
| Reactive | Reactive edema forms for no apparent reason as a result of latent or sluggish inflammatory processes (allergic edema is included in this group) |
| Perifocal | Destruction of bone plates and the formation of edema occurs against the background of a tumor process (including benign formations) |
| Infectious | The cause of infectious edema is bacterial, fungal and viral lesions of the bones of the spine (including damage by Mycobacterium tuberculosis). It is extremely rare that the cause of pathology can be chronic helminthiases and protozoan infestations |
Depending on the location of the inflammatory process, edema can be subchondral (subchondral bone plates are affected) and trabecular (fluid accumulates in the cancellous bone). Trabecular edema is the most common type of hematopoietic bone marrow edema.
Video - Bone marrow and stem cells
Varieties
Swelling of the spinal cord has its own classification, which simplifies the process of choosing treatment tactics when determining the type at the diagnostic stage. Each type has its own characteristics and features.
- Trabecular. Occurs when the spine is injured and vertebrae are destroyed. Against the background of deformed cartilage, an accumulation of fluid appears, which causes severe pain to the person, nausea, dizziness and other characteristic symptoms are observed.
- Subchondral. A process occurs as a result of the destruction of cartilage in the vertebrae. The degree of danger depends on the size of the edema.
- Aseptic. Swelling affects the neck and head of the femoral bone. Against the background of the report, a high body temperature, swelling at the site of localization, and acute pain when pressed appear. Inflammation gradually develops, and functional damage to the area occurs.
- Reactive. Usually occurs after surgery, as it is characterized by the ingestion of pathogenic microflora. Swelling is accompanied by acute pain.
- Perifocal. It is formed when the white matter of the brain enters the plasma proteins. Swelling can be small or extensive and usually does not require surgery.
- Infectious. The cause of the damage is the entry of dangerous pathogens into the body. In rare cases, swelling is caused by helminths or infestations.
Treatment at home after confirmation of the diagnosis is unacceptable, as the risk of complications is high. Therefore, a patient with any form of the disease must be hospitalized in the inpatient department of the hospital.
Spinal cord swelling most often occurs as a result of tissue damage
No ads 1
Signs and symptoms
The clinical picture of bone marrow edema is almost always blurred, which makes it difficult to make a correct diagnosis in a timely manner and often leads to the development of complications. The first (and often the only) symptom of such disorders is pain. A distinctive feature of the pain syndrome in such patients is its localization: painful sensations do not appear at the site of the pathological process, but several centimeters above. This is due to the fact that the vertebral body, which swells with excess fluid, compresses the nerve endings of the spinal nerves located above, as well as the muscles and ligaments located nearby.
In the absence of necessary treatment for a long time, the spinal cord is often involved in the process, so the clinical picture of primary disorders often overlaps with neurological symptoms.
In general, the symptoms of bone marrow edema include the following:
- aching, constant pain predominantly above the affected vertebra (can intensify both at rest and with various types of stress);
- disruption of the functioning of the pelvic organs (difficulty urinating, constipation with painful tenesmus, pain during bowel movements or bladder);
- neurological disorders (impaired sensitivity of the limbs).
Constantly aching pain, mainly above the affected vertebra, is the main sign of bone marrow edema
If the cervical spine is damaged, hydrocephalus may develop (excessive accumulation of cerebrospinal fluid in the ventricles of the brain), increased intracranial pressure, and damage to the nerves responsible for the innervation of the eye muscles.
Since the bone marrow is also involved in the formation of immunity, pathologies of this organ are almost always manifested by a decrease in the body’s resistance to the effects of allergens and pathogens. The patient may experience various allergic reactions, colds and intestinal infections, and possible exacerbation of radiculitis due to hypothermia.
Hemorrhagic syndrome with bone marrow lesions is strongly expressed, and its localization is not always determined at the site of the pathological process. The patient experiences increased bleeding of the gums, frequent nosebleeds, and bruises and hematomas on the body.
Important! The most important symptom of bone marrow pathologies is anemia, which is detected during a clinical blood test and is characterized by a decrease in hemoglobin levels (normal range is from 120 to 150 g/l). If the results of blood tests reveal anemia in a patient, which is combined with back pain, the doctor may suspect trabecular or subchondral edema of the bone marrow of the spine.
Main symptoms of anemia
Musculoskeletal disorders in internist practice - diagnosis, treatment approaches
Musculoskeletal disorders are widespread and occur in all age groups of the population. The vast majority of patients are middle-aged and elderly. The leading complaint is pain in the joints and back associated with physical activity, appearing and/or intensifying in the second half of the day/first half of the night, decreasing with rest, while local and systemic signs of inflammation are slightly expressed.
Typical representatives of the group of musculoskeletal diseases are osteoarthritis (OA), periarticular pathology (enthesitis, bursitis, tendonitis, etc.), and nonspecific low back pain (LBP).
OA is a multifactorial disease, the development of which is facilitated by genetic factors, obesity, physical inactivity, microtrauma of the joints, excessive physical effort, as well as “major” joint injuries [1]. As defined by The Osteoarthritis Research Society International (OARSI) 2005, OA is a disorder involving mobile joints characterized by cellular stress and extracellular matrix degradation initiated by micro- and macro-injury that activate inappropriate repair responses, including pro-inflammatory pathways of the immune system [2].
Currently, several OA phenotypes have been described [3].
OA phenotypes:
- obesity-induced phenotype (oxidative stress, leptin dysregulation, endothelial dysfunction) - OA of the spine and supporting joints;
- phenotype associated with sports loads - microtraumatization of supporting joints (shoulder, elbow, hip, knee), including against the background of torsional loads;
- hypodynamic phenotype - OA of the spine (spondyloarthrosis), shoulder, wrist and hand joints (due to the use of smartphones and a computer mouse);
- a phenotype associated with nutritional deficiency (including hypovitaminosis D, C) - characterized by damage to more than three groups of joints (generalized OA).
OA represents a heterogeneous group of diseases of various etiologies, in which the process involves not only articular cartilage, but also subchondral bone, ligaments, joint capsule, synovium and periarticular muscles.
The progression of OA is a consequence of the interaction of mechanical, biological, biochemical and molecular factors that disrupt the normal cycle of synthesis and degradation of articular cartilage chondrocytes, extracellular matrix (ECM) components and subchondral bone. In normal cartilage, there is a balance between the synthesis and degradation of CM constituents, whereas in OA, the dynamic balance is disrupted as a result of loss of type II collagen. In addition to disorders of cartilage metabolism and changes in subchondral bone, inflammation plays a large role in the pathogenesis of OA. The inflammatory process affects almost all structures of the joint with the formation of chondritis, synovitis and osteitis [4].
The interactions of cytokines, enzymes, and matrix breakdown products lead to a decrease in the content of proteoglycans in cartilage, disruption of the architectonics of the matrix, and the appearance of microcracks and tears in the cartilage. These processes can intensify when microvasculature vessels grow into the cartilage. The inflammatory process involves the synovial membrane and subchondral bone. At this stage, pain may occur. Since cartilage is not innervated, pain is a sign of involvement of periarticular tissues in the pathological process. In addition, sources of pain in OA can also be synovitis, trabecular microfractures, pressure on the exposed subchondral bone, formation of osteophytes, increased intraosseous pressure due to venous stagnation, spasm of nearby muscles, and degenerative changes in ligaments [4].
One of the most significant and disabling forms of OA is gonarthrosis. Its main symptom is mechanical pain that occurs when walking and especially when going up or down stairs. The pain is localized in the front or inner parts of the joint and can radiate to the lower leg. The main place is given to the assessment of pain syndrome in OA, the clinical palette of which is determined by its various pathogenetic variants:
- mechanical type of pain - associated with physical activity, relief at rest;
- continuous night pain (first half of the night) - caused by venous stasis in the subchondral bone, increased intraosseous pressure;
- “starting” pain for 15–20 minutes after periods of rest is a consequence of friction of articular surfaces, cartilage fragments in the joint cavity;
- constant pain due to reactive synovitis, combined with morning stiffness and swelling of the joint area.
M. Lequene’s criteria are used as diagnostic criteria for knee OA, which best reflect the clinical understanding of this disease:
- limitation and/or pain during passive flexion of the knee joint (normal flexion is at least 135°, extension is 0°);
- narrowing of the gap of the femorotibial or femoral-patellar joints;
- osteophytes and/or subchondral sclerosis, subchondral cysts.
The diagnosis is established in the presence of all three signs and the exclusion of diseases such as ischemic bone necrosis, Paget's bone disease, chondrocalcinosis (pyrophosphate arthropathy), hemochromatosis, ochronosis, hemophilia, arthritis, joint infections (including tuberculosis), Charcot's joint (neuroarthropathy) ), pigmented villonodular synovitis, chondromatosis [4].
At the present stage, factors for the progression of OA have been described:
- age;
- pain intensity > 60 mm on visual analogue scale (VAS);
- reactive synovitis;
- bone marrow edema according to magnetic resonance imaging (MRI);
- local and systemic osteoporosis;
- low vitamin D levels;
- metabolic syndrome;
- Muscle weakness/sarcopenia is an important risk factor for the development and progression of knee OA, as well as poor outcome and functional impairment.
In 85% of patients with OA, according to morphological data, inflammatory changes are detected in the area of the “synovioenthesial complex,” which indicates a close connection between the synovium and periarticular structures [5]. When describing periarticular pathology, the following terms are usually used:
Bursitis is an inflammation of the synovial bursae, mainly in the joint area (subacromial, olecranon, trochanteric, prepatellar, bursa anserine).
Tendonitis is inflammation of the tendon (tendinitis) and its sheath (tenosynovitis) (biceps, supraspinatus, calcaneal (Achilles) tendon, infrapatellar).
Enthesopathy/enthesitis - inflammation in the places of attachment of tendons, fascia, ligaments to bones, most often in places of apophyses, tuberosities, condyles, processes (lateral and medial epicondylitis).
The main causes of periarticular pathology (tendonitis and enthesitis):
- overload (change in physical activity stereotype);
- trauma (single or repeated microtrauma);
- local injection of glucocorticosteroids into the thickness of the tendon;
- congenital anomalies of joint structures leading to disruption of biomechanics;
- imbalance of the muscles surrounding the joint;
- physical inactivity (immobilization);
- disruption of the blood supply to certain areas of the tendons;
- age-related involution of the musculoskeletal system.
Characteristic clinical features of periarticular lesions are pain during certain movements and its local nature (the patient indicates the point of maximum pain), a decrease in the volume of active while maintaining the range of passive movements, asymmetry of the joint, the connection of swelling with a specific bursa, tendon sheath.
Anserine tendinitis/bursitis (pes anserinus - the place of attachment to the tibia of the sartorius (m. sartorius), thin (m. gracilis) and semitendinosus (m. semitendinosus) tendons. Anatomically located 3-4 cm below the projection of the knee joint gap along the medial its surface). Risk factors for the development of tendinitis are sports activities (running), osteoarthritis, meniscal tears, obesity, long walking, sudden increase in loads on the legs, flat feet, diabetes.
Anserine tendonitis is characterized by pain when climbing stairs (with gonarthrosis - increased pain when descending), lying on your side, when placing one knee on the other. The patient points to a painful point corresponding to the location of the anserine bursa; upon palpation, severe pain and swelling (less often) is noted in the “interested” area.
Tendinitis/bursitis of the greater trochanter (trochanteritis) - develops more often in women aged 40–60 years suffering from OA of the hip joint. Trochanteritis is characterized by deep, burning pain along the lateral surface of the joint and thigh, which increases when walking on a level surface and climbing stairs, squatting, which is combined with lameness in some patients. The constant nature of the pain indicates trochanteric bursitis. A decrease in pain intensity is noted at rest, intensifying at night, lying on the painful side. Upon examination, there are no restrictions on passive and active movements in the hip joint, local pain is noted in the area of the greater trochanter upon palpation, and pain occurs with resistance to active abduction of the hip.
Nonspecific LBP is a universal model of musculoskeletal disorders in patients of all age groups, including damage to the muscles, ligaments, and articular apparatus of the spine. In the occurrence of acute BS, an important role is played by local damage to the ligamentous apparatus of the spinal column, primarily the short ligaments (yellow, intertransverse and interspinous), which stabilize the spine at the segmental level against the background of non-physiological movements and excessive load. The development of muscle dysfunction, enthesopathies, tendinopathy of the involved muscles, combined with OA of the facet joints, spondylosis, underlies the development of chronic PS, while the maintenance of pain in some patients is due to the development of phenomena of peripheral and central sensitization (Fig.) [5].
Myofascial dysfunction (myofascial syndrome, MFS), associated with physical or postural stress, is characterized by the formation of dense painful bands and areas of increased sensitivity (trigger points, TT) within the affected muscle with a pattern of referred pain or sensory disturbances (paresthesias) upon palpation, and also limiting range of motion.
MFS of the quadratus lumborum muscle is accompanied by pain in the lumbar region of a deep nature with irradiation to the sacroiliac joint and gluteal region, with a deep location of the TT - to the thigh, the region of the iliac crest and the groin region. The formation of TT in the quadratus lumborum muscle occurs during forced movements, accompanied by bending and turning the torso, lifting a load, as well as during postural tension associated with gardening work. Pain in the lumbar region occurs and intensifies when walking, bending the body, turning in bed, getting up from a chair, coughing, sneezing. The pain is most intense in a horizontal position. To identify TT, deep palpation is necessary with the patient lying on the healthy side. When bending the torso in the direction opposite to the localization of the spasmed muscle, the pain syndrome intensifies [6].
MFS of the piriformis muscle is characterized by aching, pulling, cerebral pain in the gluteal region, in the sacroiliac joint, hip joint and along the back surface of the sore leg. Painful phenomena intensify after prolonged sitting, at the beginning of walking, in a standing position, half-squatting, or when trying to adduct the hip. Pain relief occurs in a lying position, sitting with legs apart, and during a short walk. The range of motion in the lumbar spine is not changed, straight leg raising is often limited. TPs in the piriformis muscle are most often activated during movements associated with forced rotation on one leg, falls, and prolonged abduction of the legs at the hip and flexion at the knee joints during obstetric and urological manipulations.
Pain with spondyloarthrosis is localized in the paravertebral region, is unilateral or bilateral, and can radiate down the leg to the level of the knee. Pain syndrome occurs after episodes of prolonged immobility, increases with extension, decreases with flexion and movement, neurological disorders are not typical. Overextension of the spine or a combination of extension and rotation provokes pain (positive Kemp test) [7].
A screening assessment of the condition of the musculoskeletal system (GALS - Gait - gait, Arm - arm, Leg - leg, Spine - spine) is recommended to be carried out, taking into account the following anamnestic information [8]:
- Do you have pain and stiffness in your muscles, joints, and spine?
- Can you fully dress yourself?
- Are you able to go up and down stairs without difficulty?
In the diagnosis of diseases of the articular apparatus, it is important to assess the signs of direct damage to the joint and periarticular pathology. In the first case, the pain is constant, present at rest, intensifies with movement, is accompanied by a decrease in the volume of both active and passive movements; an objective examination reveals effusion in the joint (reactive synovitis in OA), thickening of the synovial membrane, and intra-articular crunch.
Therapeutic tactics for OA, periarticular pathology, and nonspecific LBP are reduced to relieving pain as quickly as possible using nonsteroidal anti-inflammatory drugs (NSAIDs), the effectiveness of which is assessed 7–14 days from the start of taking the full therapeutic dose; oral administration is preferable. For short-term treatment of very intense acute pain and/or when oral administration is not possible, the use of injectable NSAIDs for a duration of no more than three days is recommended. For mild or moderate pain and a high risk of complications when taking NSAIDs systemically, local forms of NSAIDs (ointments, gels, sprays) are used [5].
The algorithm for managing patients with OA includes following recommendations for weight loss, a balanced diet, and physical therapy. In the presence of reactive synovitis, a protective regimen is indicated until the inflammation is relieved. To curb the progression of OA, a course of basic therapy (symptom-modifying drugs with delayed action) is indicated. Balneotherapy, ultrasound therapy, magnetic therapy, and electrophoresis with glucocorticosteroids (GCS) are used as physiotherapeutic treatment.
In the presence of periarticular lesions, it is recommended to limit active movements involving the involved structures for 2–3 weeks. Periarticular administration of corticosteroids is carried out if NSAIDs are ineffective, physiotherapeutic procedures (phonophoresis, electrophoresis, cryotherapy, magnetic currents, balneotherapy), and physical therapy. Local injections of GCS are carried out in the presence of local inflammation in the area of a clearly defined anatomical structure and the absence of effect when using NSAIDs for at least 7-14 days. The interval between injections of GCS should be 2–3 weeks; no more than three injections in one area within 12 months are recommended [5].
For nonspecific LBP, bed rest should be limited to 72 hours. Drug therapy in the acute period can be multicomponent (NSAIDs, muscle relaxants for a short course of up to 10 days, analgesics). In the presence of MFS, preference is given to the prescription of muscle relaxants and the use of manual muscle relaxant techniques. Weekly assessment is recommended for acute LBP or exacerbation of chronic LBP. Correction of management tactics (including consultation with a neurologist) if it is ineffective is carried out after 4–6 weeks (for a chronic course - monthly examination) [9].
Priority in the treatment of OA is given to drugs with delayed symptomatic action (SYSADOA - Symptomatic Slow-Acting Drugs for Osteoarthritis). The latter are characterized by their natural origin, the presence of reliable data on clinical effectiveness and a low frequency of undesirable effects. In the treatment of OA, chondroitin sulfate, glucosamine, unsaponifiable compounds of soy and avocado, diacerein, and hyaluronic acid are used.
In clinical practice, for several decades, a multicomponent drug of delayed symptomatic action has been widely used, demonstrating high clinical efficacy and safety - Alflutop - a standardized injection solution based on a bioactive concentrate from small marine fish. The drug contains sulfated glycosaminoglycans, similar to the matrix of hyaline cartilage: chondroitin-4-sulfate, chondroitin-6-sulfate, dermatan sulfate, keratan sulfate, glucuronic acid, free amino acids, macro- and microelements (sodium, potassium, calcium, magnesium, iron, copper , zinc) (table).
According to new experimental data obtained in vitro, Alflutop demonstrates a pathogenetic mechanism of action in OA.
The mechanism of action of the drug Alflutop:
- Inhibition of cartilage degradation - inhibition of the expression of proteases, hyaluronidase.
- Strengthening catabolic processes - increasing the synthesis of aggrecan and hyaluronic acid.
- Anti-inflammatory effect - inhibition of extracellular release of interleukins (IL-1β, IL-6, IL-8), vascular endothelial growth factor (VEGF), expression of cyclooxygenase-2, regulation of the expression of pro-inflammatory cytokine genes.
- Antioxidant effect - inhibition of the production of superoxide radicals, activation of enzymes involved in oxidative reactions.
- Effect on phosphorus-calcium metabolism - slows down bone resorption and reduces the loss of calcium ions.
In addition, experimental studies on a standardized cell line of normal human bone chondrocytes (CHON-001) have proven the chondroreparative effect of Alflutop. Proliferative status (indicative of dynamic cellular regeneration) and extracellular release of transforming growth factor beta (TGF-β), a key protein in extracellular matrix homeostasis, were studied. In the study, Alflutop demonstrated TGF-β activation and an improvement in cell proliferative index by more than 50% compared to control cells; the drug stimulates the synthesis of deoxyribonucleic acid and mitosis of chondrocytes, this effect is dose-dependent [10].
The drug Alflutop has a wide range of clinical evidence base. With the participation of employees of the Department of Faculty Therapy named after. acad. A. I. Nesterov Russian National Research Medical University named after. N.I. Pirogov conducted a two-year, multicenter, blind, randomized, placebo-controlled clinical trial to study the symptom- and structure-modifying effects of the drug Alflutop in gonarthrosis [11]. The study included 90 patients with knee OA of stages 2 and 3 according to the Kellgren–Lawrence classification. Patients were randomized into two groups of 45 people each: the first received intramuscular injections of Alflutop 1 ml in courses of 20 days at intervals of six months for two years (four courses in total), the second received injections of placebo (isotonic sodium chloride solution) according to a similar scheme . Ibuprofen was prescribed as concomitant therapy at a dose of 600–1200 mg/day. The differences in the absolute value of the reduction in pain intensity according to the Western Ontario and McMaster Universities Osteoarthritis Severity Index (Western Ontario McMaster Universities OA Index - WOMAC) between the groups were significant. A significant decrease in stiffness in the Alflutop group was observed by the third visit (p < 0.001). A statistically significant improvement in quality of life was noted by the sixth visit only in the Alflutop group (p = 0.0045). Patients in the main group reduced their intake of NSAIDs in 79% of cases and discontinued them in 21% of cases. A significant slowdown in joint space narrowing was observed in patients receiving Alflutop, in contrast to patients receiving placebo (p = 0.0003). After three months of treatment with Alflutop, there was a trend toward a decrease in the level of the cartilage degradation marker C-terminal cross telopeptides of type II collagen (CTX-II). In the placebo group, CTX-II levels did not change. Based on the results obtained, the authors of the study concluded that Alflutop has a structure-modifying effect in OA of the knee joints.
The effectiveness of periarticular administration of Alflutop in patients with gonarthrosis with signs of damage to the tendon-ligamentous apparatus, as well as enthesopathies of the supraspinatus and/or subscapularis muscles has been demonstrated in several studies [12, 13]. A course of administration of the drug to pain points corresponding to the entheses of the affected muscles led to a decrease in pain in the shoulder joint, an increase in range of motion, and a decrease in the dose of NSAIDs taken. In a double-blind, placebo-controlled study by O. S. Levin et al. the drug was prescribed for chronic vertebrogenic lumboischialgia associated with spondyloarthrosis. The study compared the effectiveness of intramuscular and paravertebral routes of administration of Alflutop. The authors conclude that there is a statistically significant decrease in the intensity of pain with paravertebral administration compared to placebo [14].
The drug is prescribed according to the following regimens:
- For OA of large joints - 2 ml intra-articularly once every three days (six injections), followed by intramuscular injection of 1 ml daily for 20 days.
- For spondyloarthrosis - paravertebral 0.25 ml at four points (1 ml in total) at the level of two adjacent vertebral segments twice a week (five injections), followed by intramuscular injection of 1 ml daily for 20 days.
- For generalized osteoarthritis - deep intramuscular injection, 1 ml per day (20 injections in total).
Thus, the available data on the high clinical efficacy and safety of the drug Alflutop, which has a clear symptom- and structural-modifying effect, allows us to recommend its use as basic therapy in patients with musculoskeletal disorders such as gonarthrosis, spondyloarthrosis, tendonitis, enthesitis, including in patients with comorbidity, if long-term therapy for OA is necessary and limiting the intake of NSAIDs.
Literature
- Kristjansson B., Honsawek S. Current perspectives in mesenchymal stem cell therapies for osteoarthritis // Stem Cells Int. 2014: 194318. DOI: 10.1155/2014/194318.
- Kraus VB, Blanco FJ, Englund M. et al. // Osteoarthritis Cartilage. 2015; 23(8):1233–1241.
- Van der Esch M., Knoop J., van der Leeden M. et al. // Osteoarthritis Cartilage. 2015; 23(4):544–549.
- Shostak N. A., Pravdyuk N. G. Osteoarthrosis: determinants of pain, approaches to treatment // Breast Cancer. 2021. No. 22. pp. 1476–1480.
- Nasonov E. L., Yakhno N. N., Karateev A. E. et al. General principles of treatment of musculoskeletal pain: interdisciplinary consensus // Scientific and practical rheumatology. 2016; 54(3):247–265. DOI: 10.14412/1995–4484–2016–247–265.
- Shostak N. A., Pravdyuk N. G., Timofeev V. T., Abeldyaev D. V. Regional pain syndromes of soft tissues in the practice of a therapist // RMZh. 2021. No. 9. pp. 648–652.
- Deconstructing Chronic Low Back Pain in Older Adults: Summary Recommendations // Pain Med. 2016; 17(12):2238–2246. DOI: 10.1093/pm/pnw267.
- https://en.wikipedia.org/wiki/GALS_screen.
- Clinical guidelines “Diagnostics and treatment of chronic back pain in general medical practice.” Association of General Practitioners. M., 2013.
- Olariu L., Brindusa D., Buse E., Pyatigorskaya NV, Pavlov A. “In vitro” chondro-restitutive capacity of Alflutop® proved on chondrocyte cultures // Romania Biotechnological Letters. 2021, vol. 22, no. 6.
- Alekseeva L. I., Sharapova E. P., Taskina E. A. et al. A multicenter, blind, randomized, placebo-controlled study of the symptom- and structure-modifying effects of the drug Alflutop in patients with osteoarthritis of the knee joints. Message 2 - assessment of the structure-modifying effect of the drug // Scientific and practical rheumatology. 2014. T. 52. No. 2. pp. 174–177.
- Salikhov I.G., Volkova E.R., Yakupova S.P. Periarticular use of chondroprotectors in patients with gonarthrosis with signs of damage to the tendon-ligamentous apparatus // Consilium Medicum. 2006. T. 8. No. 2. P. 59–61.
- Khitrov N. A. Periarthritis of the shoulder joint - modern ways of treatment // Consilium Medicum. 2010. No. 1. P. 65–70.
- Levin O. S., Olyunin D. Yu., Golubeva L. V. The effectiveness of Alflutop in chronic vertebrogenic lumbar sciatica according to a double-blind, placebo-controlled study // Scientific and Practical Rheumatology. 2004. No. 4. pp. 80–84.
N. A. Shostak, Doctor of Medical Sciences, Professor N. G. Pravdyuk1, Candidate of Medical Sciences
Federal State Budgetary Educational Institution of Russian National Research University named after. N. I. Pirogova Ministry of Health of the Russian Federation, Moscow
1 Contact information
* It is advisable to repeat the course of treatment after six months.
Musculoskeletal disorders in internist practice - diagnosis, approaches to treatment / N. A. Shostak, N. G. Pravdyuk
For citation: Attending physician No. 12/2017; Issue page numbers: 68-73
Tags: pain syndrome, joints, spine, myofascial syndrome
Diagnostics
When choosing a diagnostic method in patients with complaints typical of bone marrow edema, it is important to consider that in most cases, radiography does not detect signs of fluid accumulation or exudate. It is more advisable for such patients to be prescribed a magnetic resonance scan (magnetic resonance imaging), which not only identifies foci with the presence of exudate, but also allows one to measure its amount.
The main task of MRI is to identify possible edema and its location. Ancillary diagnostic methods are aimed at establishing the cause of edema and associated disorders. Depending on the symptoms present, these may be the following methods:
- computed multislice tomography;
- blood tests for tumor markers and rheumatoid factors;
- radiography of the spine;
- examination of the cerebrospinal fluid tract (if complications are suspected in the functioning of the spinal cord located in the central spinal canal).
Diagnosis of bone marrow edema
If you want to find out in more detail the indications and procedure for MRI of the cervical spine, as well as familiarize yourself with the contraindications, you can read an article about this on our portal.
To exclude malignant processes, a biopsy of biological materials may be prescribed, followed by histological examination.
Characteristics of the disease
Spinal cord edema occurs due to excess fluid accumulation in the spinal cavity. This happens due to damage to the ridge, blood vessels, or a failure in the natural process of removing cerebrospinal fluid. Usually this is the body’s reaction to negative external influences, but the process can begin due to the entry of dangerous bacteria and pathogenic microorganisms into the circulatory system. In this case, it is they who increase the volume of tissue due to the onset of local inflammation.
This condition is dangerous for humans, and without medical help a variety of complications develop. If swelling is suspected, the doctor will prescribe tests and an MRI. They allow you to make an accurate diagnosis and take the necessary measures.
Can bone marrow edema be treated with leeches?
Hirudotherapy, which is often recommended as a safe and effective method of treating spinal pathologies, cannot be used for various bone marrow edema. Hirudotherapy is based on the method of bloodletting, so any conditions accompanied by heavy or regular blood loss are a contraindication for treatment with leeches. In addition, in patients with signs of anemia, hirudotherapy can lead to an even greater drop in hemoglobin and associated consequences, including:
- organic lesions of the nervous system;
- impaired absorption of certain vitamins, macro- and microelements;
- cardiomyopathy;
- thinning of epithelial tissue and mucous membranes;
- chronic stomatitis;
- hematological diseases, etc.
What is hirudotherapy
In rare cases, hirudotherapy can be used to treat fresh injuries, but only if the patient does not have symptoms of anemia (including those confirmed by a clinical blood test) and hemorrhagic syndrome.
Who is at risk
- Persons whose immediate blood relatives have suffered from myeloma, leukemia or lymphoma.
- Patients with primary and secondary immunodeficiencies.
- Persons exposed to ionizing radiation (those undergoing radiation therapy, liquidators of the Chernobyl disaster) or chemical carcinogens.
- Persons who have taken or are taking antitumor drug therapy.
- The presence of predisposing diseases - mononucleosis, monoclonal gammopathy.
Prevention
Prevention of bone marrow edema involves timely treatment of spinal diseases, infectious pathologies, maintaining sufficient physical activity and preventing injuries (move carefully on slippery surfaces, fasten seat belts in a car, etc.).
Specific prevention of bone marrow pathologies consists of following recommendations for maintaining normal hematopoietic function.
- The daily diet should contain a sufficient amount of foods that have a positive effect on the function of hematopoiesis (veal, cod liver, beef liver, eggs, pomegranates, apples).
- Maintaining an optimal balance of minerals and nutrients is of great importance for the prevention of any edema. Nutrition should be varied and balanced in the content of nutrients and nutrients.
- To prevent sodium retention in the body, salt intake should be limited to 1 teaspoon per day.
- Back massage improves blood circulation and normalizes lymph flow. It is recommended to do it for the purpose of prevention 2-3 times a year for 5-10 sessions (outside of exacerbations of any pathologies of the spine).
Surgical treatment and complications of bone marrow edema
Bone marrow edema is a serious disease that can cause serious neurological disorders and even disability. When the first symptoms of pathology appear, you should immediately seek medical help. A favorable prognosis for patients with this diagnosis is possible only with early initiation of therapy, so you should not delay visiting a medical facility if at least one of the possible signs is present.
Possible complications
Swelling of the spinal cord is quite favorable if you consult a specialist in a timely manner. With complex treatment, the patient completely restores all impaired functions and mobility of the spine; any physical activity is allowed after rehabilitation. If treatment is started late, there is a risk of paralysis, partial or complete, or death.
The most common consequence of the pathology is loss of limb mobility and dysfunction of the pelvic organs. The prognosis largely depends on the location of the lesion, the degree of progression of the disease before seeking medical help, and the age of the patient. The higher the swelling is located, the higher the likelihood of complete paralysis.
The patient's legs should be higher than the level of the head, to reduce swelling, bed rest is strictly observed
Other diseases - clinics in
Choose among the best clinics based on reviews and the best price and make an appointment
Family
Scoliosis Treatment Center named after K. Schroth
Moscow, st.
Azovskaya, 24, building 2 POM VI/KOM 5,6,7/ET 1 Sevastopolskaya
+7
- Consultation from 1500
- Exercise therapy from 2700
0 Write your review
Family
Oriental Medicine Clinic "Sagan Dali"
Moscow, prosp.
Mira, 79, building 1 Rizhskaya
+7
- Consultation from 1500
- Diagnostics from 0
- Reflexology from 1000
0 Write your review
Family
Center for Chinese Medicine "TAO"
Moscow, st.
Ostozhenka, 8 building 3, 1st floor Kropotkinskaya
+7
- Consultation from 1000
- Massage from 1500
- Reflexology from 1000
0 Write your review
Show all Moscow clinics
Methods of treating the disease
The main treatment for a spinal cord tumor is surgical removal. Operations are prescribed after a complete examination of the patient and an accurate diagnosis. Today, the capabilities of neurosurgeons are significantly increased by the latest medical equipment:
— endoscopy technology provides the opportunity to gain access to tumors in hard-to-reach places;
— thanks to microsurgical instruments, the risk of complications during and after the procedure is reduced.
Our neurosurgery department has modern operating microscopes made in Germany with the highest degree of resolution. Their use allows surgeons to avoid damaging healthy areas.
The recovery period after removal of benign tumors ranges from several months to two years. In 70% of cases, complete recovery is achieved. In the case of intramedullary and low-quality formations, the prospect is not so comforting. Metastatic tumors are usually inoperable.
Further treatment for a spinal cord tumor after surgery includes:
- chemotherapy;
- radiation therapy.
To rehabilitate the patient, physiotherapeutic methods, fixation of the spine from the outside, and learning to walk again are prescribed. It is advisable to carry out social and psychological rehabilitation.
You can make an appointment using the contact number. We will provide a free consultation about the treatment of a spinal cord tumor, approximate prices and answer other questions.
The cost of surgical removal depends on the type of tumor and the nature of the surgical procedure. We guarantee operations at the highest level and at reasonable prices.
Other diseases - specialists in Moscow
Choose among the best specialists based on reviews and the best price and make an appointment
VertebrologistOrthopedist
Gromov Ilya Sergeevich
Moscow, st.
Azovskaya, 24, building 2 POM VI/KOM 5,6,7/ET 1 (Scoliosis Treatment Center named after K. Schroth) +7 Registration
0 Write your review
VertebrologistOrthopedist
Kudryakov Stepan Anatolievich
Moscow, st. Azovskaya, 24, building 2 POM VI/KOM 5,6,7/ET 1 (Scoliosis Treatment Center named after K. Schroth)
+7
Registry
0 Write your review
Orthopedist