The causes of muscle weakness are many and there is a wide range of conditions that can cause muscle weakness. These can be both well-known diseases and quite rare conditions. Muscle weakness can be reversible and permanent. However, in most cases, muscle weakness can be treated with exercise, physical therapy, and acupuncture.
Muscle weakness is a fairly common complaint, but the word weakness has a wide range of meanings, including fatigue, decreased muscle strength, and the inability of muscles to work at all. There is an even wider range of possible causes.
The term muscle weakness can be used to describe several different conditions.
Primary or true muscle weakness
This muscle weakness manifests itself as an inability to perform a movement that a person wants to perform using the muscles the first time. There is an objective decrease in muscle strength and strength does not increase regardless of effort. That is, the muscle does not work properly - this is abnormal.
When this type of muscle weakness occurs, the muscles appear to have collapsed and become smaller in volume. This can happen, for example, after a stroke. The same visual picture occurs with muscular dystrophy. Both conditions result in weakened muscles that cannot perform normal activities. And this is a real change in muscle strength.
Features of the development of the musculoskeletal system in a child of the first year of life
Among clearly defined diseases and deformations of the musculoskeletal system of infants, in practice there are a large number of unstable, transient disorders that cause concern for parents. This is the calcaneal and calcaneal-valgus position of the feet in a newborn, apparent flat feet, asymmetry of skin folds on the hips and buttocks, varus (O-shaped) curvature of the legs, erratic movement of the arms, limited abduction of the legs bent at the hip and knee joints, etc.
To distinguish a pathological condition from a normal one, it is necessary to know the characteristics of the child’s development and his motor capabilities.
Thus, unfixed calcaneal-valgus position of the feet, as a rule, occurs due to intrauterine compression of the feet, and quickly disappears after birth. Gymnastics and massage, bandaging a soft cotton roll to the back of the foot speeds up the process of restoring normal foot function.
The absence of a longitudinal arch of the plantar surface of the feet, which is typical for adults, during loading in an infant does not yet indicate the presence of flat feet, because The arch is formed during the first years of life, and before that it is poorly expressed due to the thick fatty layer on the plantar surface. In this case, it is necessary to monitor whether there are conditions conducive to the formation of flat feet (obesity, excess weight, weakness of the musculo-ligamentous apparatus, including rachitic origin, deformities of the knee joints and feet). In all these cases, preventive measures will include gymnastics, massage, limiting the load, wearing orthopedic shoes, etc.
As for varus (O-shaped) deformity of the lower extremities, it is typical for newborns and goes away over time, but with the slightest increase in curvature, it is necessary to take preventive measures (reducing the load on the lower extremities, combating the obesity of the child, carrying out antirachitic measures, massage, gymnastics , baths). The child normally moves his arms randomly, but erratic arm movements in a properly developing child should become purposeful by 2-3 months.
Often in newborns and infants, asymmetry of skin folds on the thighs and buttocks is detected. In this case, you should pay attention not to the folds on the hips and their number, but to the gluteal-femoral and popliteal folds, which, during dislocation and subluxation of the hip, are located asymmetrically at different levels. Experience has shown that in almost 80% of children, asymmetry of skin folds on the hips is not accompanied by dysplasia (underdevelopment) of the hip joints, and only 20% is accompanied by dysplasia.
Normally, hip abduction with bent legs in children in the first months of life is achieved up to 80-90`. Limitation of abduction at this age may depend on increased tone of the adductor muscles rather than on anatomical changes in the hip joint. This physiological increase in muscle tone in children in the first months of life creates a picture of limited movement in various joints, including the hip. But if it is limited and impossible beyond the 70-75 position, such a child should be examined and taken for treatment by an orthopedist as suspicious for dysplasia. In this case, it is necessary to check the stability of the hip joints. Crunching and clicking in the hip joint or (both joints) is an indicator of joint instability or slipping of the femoral head from the socket (dislocation or subluxation of the hip). In these cases, treatment is required. It boils down to wide swaddling: two diapers are folded several times and placed between the baby’s legs, bent at the hip and knee joints and abducted 70-80° (such swaddling can be recommended for all children, because in this position the hip joints develop better and it is physiological in the first days of a child’s life).
Delayed development of the statokinetic functions of crawling, sitting, and standing up often frightens parents, but one must keep in mind that the timing of development of these functions is very individual and if a child has not yet begun to walk at one year, this does not mean that he is sick. However, in these cases, in the absence of signs of any disease, as with rickets, general massage, gymnastics, baths should be prescribed, and the child’s nutrition and regimen should be checked. These and many other concerns of parents are best resolved during preventive examinations by an orthopedist and neurologist in the first months of life.
Muscle fatigue
Fatigue is sometimes called asthenia. This is the feeling of tiredness or exhaustion that a person feels when muscles are used. The muscles don't really get weaker, they can still do their job, but doing the muscle work requires more effort. This type of muscle weakness is often seen in people with chronic fatigue syndrome, sleep disorders, depression, and chronic heart, lung, and kidney disease. This may be due to a decrease in the rate at which the muscles can receive the required amount of energy.
Muscle fatigue
In some cases, muscle fatigue is basically increased fatigability - the muscle starts to work, but gets tired quickly and takes longer to restore function. Fatigue is often associated with muscle fatigue, but is most noticeable in rare conditions such as myasthenia gravis and myotonic dystrophy.
The difference between these three types of muscle weakness is often not obvious and a patient may have more than one type of weakness. Also, one type of weakness can alternate with another type of weakness. But with a careful approach to diagnosis, the doctor is able to determine the main type of muscle weakness, since certain diseases are characterized by one or another type of muscle weakness.
Weakness of the ligamentous apparatus in a child. In children
If weakness of the ligamentous system is the cause of problems of the musculoskeletal system in children, then physiotherapy, pain relief, and muscle strengthening are carried out.
For hereditary joint weakness, it is recommended to avoid limb hyperextension, impact and resistance exercises to reduce the risk of subluxation and dislocation.
Children should be prohibited from contact and traumatic sports if they have joint hypermobility. Myofascial release is achieved through massage and gentle osteopathic techniques.
Flat feet due to hypermobility of the ligaments is usually associated with disability and the risk of arthrosis. If the child experiences pain, then surgery is recommended. But surgery is contraindicated for people with Marfan, Down or Ehlers-Danlos syndrome.
Orthopedic therapy helps stabilize the feet and ankle to avoid injury and avoid permanent damage to the joints.
Rolling with a tennis ball or foam roller helps reduce tension in the calf muscles and knee flexors. According to Dr. Komarovsky, it is important for a child to have the right shoes that allow the foot to move, as well as physical activity to strengthen the muscles.
Patients are advised to wear knee pads and elastic bands during any physical activity to protect the joints.
You can’t stretch a child’s weak ligaments any further, so it’s better to postpone gymnastics and yoga until the muscles are strengthened.
Surgical procedures usually help temporarily.
Weak joints in a child are often associated with low muscle tone and a secondary lack of carnitine in the blood. A decrease in the level of the substance is associated with joint pain.
Carnitine, similar to B vitamins, is important for metabolism and energy metabolism. The substance helps fatty acids penetrate cells for oxidation and release of energy. Participates in the removal of oxidative reaction products from tissues and prevents the destruction of cell membranes.
For its synthesis, the amino acids lysine and methionine, vitamins C, B6, niacin, and iron are needed. With a lack of protein in the diet and a poor variety of dishes, carnitine production decreases
Carnitine deficiency occurs due to:
- lack of amino acids and cofactors for its synthesis;
- poor diet;
- decreased absorption in the duodenum;
- renal dysfunction.
With a lack of carnitine, muscle weakness and dysfunction of the cardiovascular system occur. For diagnosis, a blood test is performed, and then a corrective diet is developed.
To produce collagen, vitamin C, magnesium salt, piascledine, chondroprotectors and amino acids (lysine, proline) are used. Compensate for the lack of carnitine with appropriate supplements.
Main causes of muscle weakness
Lack of adequate physical activity - inactive (sedentary) lifestyle.
Lack of muscle exercise is one of the most common causes of muscle weakness. If the muscles are not used, the muscle fibers in the muscles are partially replaced by fat. And over time, the muscles weaken: the muscles become less dense and more flabby. And although the muscle fibers do not lose their strength, their number decreases and they do not contract as efficiently. And the person feels that they have become smaller in volume. When trying to perform certain movements, fatigue sets in faster. The condition is reversible with reasonable, regular exercise. But as we age, this condition becomes more pronounced.
Maximum muscle strength and a short recovery period after exercise are observed at the age of 20-30 years. This is why most great athletes achieve great results at this age. However, strengthening muscles through regular exercise can be done at any age. Many successful long-distance runners were over 40 years of age. Muscle tolerance during a prolonged activity such as a marathon remains high longer than during a powerful, short burst of activity such as a sprint.
It is always good when a person has sufficient physical activity at any age. However, recovery from muscle and tendon injuries occurs more slowly with age. No matter what age a person decides to improve their physical fitness, a reasonable training regimen is important. And it is better to coordinate training with a specialist (instructor or exercise therapy doctor).
Aging
As you age, muscles lose strength and mass and become weaker. While most people accept this as a natural consequence of age - especially if they are older - it is still uncomfortable to not be able to do things that were possible at a younger age. However, exercise is still beneficial in old age, and safe exercise can increase muscle strength. But the recovery time after injury is much longer in old age, as involutional changes in metabolism occur and bone fragility increases.
Infections
Infections and diseases are among the most common causes of temporary muscle fatigue. This occurs due to inflammatory processes in the muscles. And sometimes, even if the infectious disease has regressed, the restoration of muscle strength can take a long period of time. Sometimes this can cause chronic fatigue syndrome. Any illness with fever and muscle inflammation can be a trigger for chronic fatigue syndrome. However, some diseases are more likely to cause this syndrome. These include influenza, Epstein-Barr virus, HIV, Lyme disease and hepatitis C. Other less common causes are tuberculosis, malaria, syphilis, polio and dengue fever.
Pregnancy
During and immediately after pregnancy, high levels of steroids in the blood, combined with iron deficiency, can cause feelings of muscle fatigue. This is a completely normal muscle reaction to pregnancy; however, certain exercises can and should be done, but significant physical activity should be excluded. In addition, pregnant women often experience lower back pain due to impaired biomechanics.
Chronic diseases
Many chronic diseases cause muscle weakness. In some cases, this is due to a reduction in the flow of blood and nutrients to the muscles.
Peripheral vascular disease is caused by narrowing of the arteries, usually due to cholesterol deposits, and is triggered by poor diet and smoking. The blood supply to the muscles decreases, and this becomes especially noticeable during exercise, when the blood flow cannot cope with the needs of the muscles. Pain is often more characteristic of peripheral vascular disease than muscle weakness.
Diabetes is a disease that can lead to muscle weakness and loss of fitness. High blood sugar puts muscles at a disadvantage and their functioning is impaired. In addition, as diabetes progresses, a disorder occurs in the structure of the peripheral nerves (polyneuropathy), which in turn impairs the normal innervation of the muscles and leads to muscle weakness. In addition to nerves, diabetes causes damage to the arteries, which also leads to poor blood supply to the muscles and weakness. Heart disease, especially heart failure, can lead to impaired blood supply to muscles due to a decrease in myocardial contractility and actively working muscles do not receive enough blood (oxygen and nutrients) at the peak of exercise and this can lead to rapid muscle fatigue.
Chronic lung diseases , such as chronic obstructive pulmonary disease (COPD), reduce the body's ability to use oxygen. Muscles require a rapid supply of oxygen from the blood, especially during physical activity. Decreased oxygen consumption leads to muscle fatigue. Over time, chronic lung disease can lead to muscle wasting, although this mostly occurs in advanced cases when oxygen levels in the blood begin to drop.
Chronic kidney disease can lead to an imbalance of minerals and salts in the body, and may also affect the levels of calcium and vitamin D. Kidney disease also causes the accumulation of toxic substances (toxins) in the blood, since impaired excretory function of the kidneys reduces their excretion from the body. These changes can lead to both true muscle weakness and muscle fatigue.
Anemia is a lack of red blood cells. There are many causes of anemia, including poor diet, blood loss, pregnancy, genetic diseases, infections and cancer. This reduces the blood's ability to carry oxygen to the muscles so that the muscles can contract fully. Anemia often develops quite slowly, so that by the time of diagnosis, muscle weakness and shortness of breath are already noted.
Diseases of the central nervous system
Anxiety: General fatigue can be caused by anxiety. This is due to increased activity of the adrenaline system in the body.
Depression: General fatigue can also be caused by depression.
Anxiety and depression are conditions that tend to cause feelings of tiredness and "fatigue" rather than actual weakness.
Chronic pain - the overall effect on energy levels can lead to muscle weakness. Like anxiety, chronic pain stimulates the body to produce chemicals (hormones) that respond to pain and injury. These chemicals cause you to feel tired or tired. With chronic pain, muscle weakness may also occur because the muscles cannot be used due to pain and discomfort.
Muscle damage due to injury
There are many factors that lead to direct muscle damage. The most obvious are wounds or injuries such as sports injuries, sprains and sprains. Doing exercises without warming up and stretching your muscles is a common cause of muscle damage. With any muscle injury, bleeding occurs from the damaged muscle fibers within the muscle, followed by swelling and inflammation. This makes the muscles less strong and also painful when performing movements. The main symptom is local pain, but later weakness may appear.
Medicines
Many medications can cause muscle weakness and muscle damage as a result of a side effect or allergic reaction. It usually starts as fatigue. But the damage can progress if the medications are not stopped. The most common medications that cause these effects are statins, some antibiotics (including ciprofloxacin and penicillin), and anti-inflammatory painkillers (such as naproxen and diclofenac).
Long-term use of oral steroids also causes muscle weakness and wasting. This is an expected side effect of steroids with long-term use and is why doctors try to shorten the duration of steroid use. Less commonly used medications that can cause muscle weakness and muscle damage include:
- Certain heart medications (eg, amiodarone).
- Chemotherapy drugs.
- Anti-HIV drugs.
- Interferons.
- Medicines used to treat an overactive thyroid gland.
Other substances.
Long-term alcohol use can lead to weakness in the shoulder and thigh muscles.
Smoking can indirectly weaken muscles. Smoking causes narrowing of the arteries, which leads to peripheral vascular disease.
Cocaine abuse causes noticeable muscle weakness, just like other drugs.
Sleep disorders
Problems that disrupt or reduce sleep duration lead to muscle fatigue, muscle fatigue. These disorders may include: insomnia, anxiety, depression, chronic pain, restless leg syndrome, shift work, and having young children who do not sleep at night.
Other causes of muscle weakness
Chronic fatigue syndrome
This condition is sometimes associated with certain viral infections, such as Epstein-Barr virus and influenza, but the genesis of this condition is not fully understood. The muscles are not sore, but they get tired very quickly. Patients often feel that greater effort is required to perform muscle activities that they previously performed easily.
In chronic fatigue syndrome, muscles do not collapse and may have normal strength when tested. This is reassuring as it means that the chances of recovery and full restoration of function are very high. CFS also causes psychological fatigue when performing intellectual activities, for example, prolonged reading and communication also become tiring. Patients may often show signs of depression and sleep disturbances.
Fibromyalgia
This disease resembles chronic fatigue syndrome in its symptoms. However, with fibromyalgia, the muscles become painful to palpation and fatigue very quickly. Fibromyalgia muscles do not shrink and remain strong during formal muscle testing. Patients tend to complain more about pain than fatigue or weakness.
Thyroid dysfunction (hypothyroidism)
In this condition, a lack of thyroid hormones leads to general fatigue. And if hypothyroidism is not treated, muscle degeneration and malnutrition may develop over time. Such changes can be serious and in some cases irreversible. Hypothyroidism is a common disease, but, as a rule, with timely treatment, muscle problems can be avoided.
Lack of fluid in the body (dehydration) and electrolyte imbalance.
Problems with the normal balance of salts in the body, including as a result of dehydration, can cause muscle fatigue. Muscle problems can only be very serious in extreme cases, such as dehydration during a marathon. Muscles perform less well when there is an imbalance of electrolytes in the blood.
Diseases accompanied by muscle inflammation
Inflammatory muscle diseases tend to develop in older people and include polymyalgia, polymyositis and dermatomyositis. Some of these conditions are well treated by taking steroids (which must be taken for many months before there is a therapeutic effect). Unfortunately, steroids themselves can cause muscle loss and weakness if taken for a long time.
Systemic inflammatory diseases such as SLE and rheumatoid arthritis are often the cause of muscle weakness. In a small percentage of cases, rheumatoid arthritis, muscle weakness and fatigue may be the only symptoms of the disease for a significant time.
Oncological diseases
Cancer and other cancers can cause direct muscle damage, but having cancer in any part of the body can also cause general muscle fatigue. In advanced stages of cancer, loss of body weight also leads to true muscle weakness. Muscle weakness is usually not the first sign of cancer and occurs more often in the later stages of cancer.
Neurological conditions leading to muscle damage.
Diseases affecting the nerves usually lead to true muscle weakness. This happens because if the nerve of a muscle fiber stops working fully, the muscle fiber cannot contract and, as a result of lack of movement, the muscle atrophies. Neurological diseases: Muscle weakness can be caused by cerebrovascular diseases such as stroke and cerebral hemorrhages or spinal cord injuries. Muscles that become partially or completely paralyzed lose normal strength and eventually atrophy. In some cases, the changes in the muscles are significant and recovery is very slow or function cannot be restored.
Spinal disorders: When nerves are damaged (compressed at the exit of the spine by a herniation, protrusion, or osteophyte), muscle weakness can occur. When a nerve is compressed, conduction and motor disturbances occur in the zone of innervation of the root, and muscle weakness develops only in the muscles innervated by certain nerves that have undergone compression
Other nervous diseases:
Multiple sclerosis is caused by damage to nerves in the brain and spinal cord and can lead to sudden paralysis. In multiple sclerosis, partial restoration of function is possible with adequate treatment.
Guillain-Barré syndrome is an acute autoimmune inflammatory polyradiculoneuropathy, manifested by flaccid paresis, sensory disturbances, autonomic disorders, caused by a viral infection
Parkinson's disease: is a progressive disease of the central nervous system, both the motor sphere and the intellectual and emotional sphere. It mainly affects people over the age of 60 and in addition to muscle weakness, patients with Parkinson's disease experience tremors and muscle stiffness. They often have difficulty starting and stopping movements, and are often depressed.
Rare causes of muscle weakness
Genetic diseases affecting muscles
Muscular dystrophies are hereditary diseases that affect the muscles and are quite rare. The best known such disease is Duchenne muscular dystrophy. This disease occurs in children and causes a gradual loss of muscle strength.
Some rare muscular dystrophies may begin in adulthood, including Charcot-Marie-Tooth syndrome and Facioscapulohumeral dystrophy syndrome. They also cause a gradual loss of muscle strength and often these conditions can lead to disability and wheelchair use.
Sarcoidosis is a rare disease that causes clumps of cells (granulomas) to form in the skin, lungs, and soft tissues, including muscles. The condition may resolve on its own after a few years.
Amyloidosis is also a rare disease in which abnormal protein (amyloid) accumulates (deposits) throughout the body, including in the muscles and kidneys.
Other rare causes: Direct muscle damage can occur in rare inherited metabolic diseases. Examples include: glycogen storage diseases and, even more rarely, mitochondrial diseases, which occur when the energy systems inside muscle cells don't work properly.
Myotonic dystrophy is a rare genetic muscle disorder that causes muscles to fatigue quickly. Myotonic dystrophy is passed on from generation to generation, and, as a rule, with each subsequent generation the manifestations of the disease become more pronounced.
Motor neurone disease is a progressive nerve disorder that affects all parts of the body. Most forms of motor neuron disease begin in the distal extremities, gradually affecting all muscles of the body. The disease progresses over months or years and patients rapidly develop severe muscle weakness and muscle wasting.
Motor neurone disease most often affects men over 50, but there have been many notable exceptions to this rule, including renowned astrophysicist Stephen Hawking. There are many different forms of motor neuron disease, but no successful treatment has yet been developed.
Myasthenia gravis: is a rare muscle disease in which the muscles quickly fatigue and require a long time to restore contractile function. The impairment of muscle function can be so severe that patients cannot even keep their eyelids open and speech becomes slurred.
Poisons – Poisonous substances also often cause muscle weakness and paralysis due to their effects on the nerves. Examples are phosphates and botulinum toxin. If exposed to phosphates, weakness and paralysis may be permanent.
Addison's disease
Addison's disease is a rare disease characterized by hypoactive adrenal glands, which leads to a lack of steroids in the blood and an imbalance of blood electrolytes. The disease usually develops gradually. Patients may notice changes in skin color (tanning) due to skin pigmentation. There may be weight loss. Muscle fatigue can be mild and is often an early symptom. The disease is often difficult to diagnose and special examinations are required to diagnose this disease. Other rare hormonal causes of muscle weakness include acromegaly (overproduction of growth hormone), an underactive pituitary gland (hypopituitarism), and severe vitamin D deficiency.
Metabolic disorders in children with joint hypermobility syndrome
Joint pain occurs quite often in children, especially at a young age, and the causes of arthralgia are very diverse. One of them is joint hypermobility (JH), which is most often a consequence of connective tissue dysplasia. Joint hypermobility syndrome (JHS) is a condition in which children or adults with HS have certain musculoskeletal complaints, but there are no signs of any rheumatic disease. Despite the fact that HS occurs in the population with a frequency of 10–15%, only a small proportion of these patients complain of joint pain. In our work, we tried to find the reasons that contribute to the appearance of arthralgia in children with HS. For this purpose, a comparative analysis of clinical manifestations was carried out in two groups of patients with pronounced signs of connective tissue dysplasia (CTD), differing from each other in the presence or absence of arthralgia.
To identify metabolic disorders in most of the children examined, the content of microelements in the hair was determined. It is known that microelement status characterizes mineral metabolism in the body. At the same time, the most relevant for children is the state of metabolism of calcium, phosphorus, magnesium, iron, copper, sulfur, cobalt, selenium, zinc, manganese, fluorine, vanadium, silicon and boron, since these microelements are involved not only in the process of growth and development of the child , but also take an active part in collagen metabolism.
In order to diagnose connective tissue metabolic disorders at the biochemical level, a study of the synthesis and breakdown of bone collagen was carried out. The content of osteocalcin, deoxypyridinoline, beta-Cross laps and TPINP tests in blood serum and the level of pyrilinx D in daily urine were analyzed.
Increased joint mobility can be caused not only by weakness of the ligamentous apparatus, but also by a decrease in muscle tone. Recently, many reports have appeared about the presence of secondary carnitine deficiency in patients with CTD [2]. In this regard, the next objective of the study was to determine the level of carnitine in the blood of children suffering from recurrent joint pain due to HS.
Carnitine is a biologically active substance related to B vitamins, which plays an important role in cellular metabolism and, above all, in energy metabolism. It transports fatty acids across cell membranes from the cytoplasm into the mitochondria, where these acids are oxidized (beta-oxidation process) to produce large amounts of metabolic energy (in the form of ATP). Carnitine is involved in the binding and removal of organic acids from tissues, which, being intermediate products of oxidative processes, can inhibit the activity of a number of enzymes and negatively affect membrane structures.
Secondary carnitine deficiency can be caused by various reasons. For example, a low content of amino acids or cofactors for carnitine synthesis, insufficient intake from food, decreased reabsorption in the gastrointestinal tract or kidneys, as well as rapid consumption, for example, in athletes with excessive muscle load. With carnitine deficiency, the target organs are primarily skeletal muscles and myocardium, and secondarily, brain cells and other organs. The main clinical manifestations of carnitine deficiency are: decreased performance, muscle weakness, drowsiness, impaired functional state of the cardiovascular system and liver.
Clinical characteristics of children and research methods
We examined 106 children (64 boys, 42 girls) aged from 3 to 18 years with signs of CTD. All children were divided into two groups: 1st group - children with arthralgia - 47 people, 2nd group - (comparison group) consisted of 59 children with pronounced signs of CTD, but without arthralgia. The clinical examination included an assessment of physical development, identification of phenotypic, clinical, instrumental and laboratory signs of DST. The severity of CTD was determined by the scoring method [3]. To exclude the inflammatory nature of joint complaints in children of the 1st group, a full arthrological examination was carried out - a clinical and biochemical blood test, determination of rheumatoid and antinuclear factors, antibodies to chlamydia, bacteria of the intestinal group (pseudotuberculosis, salmonellosis). Additionally, the results of the Mantoux reaction, throat and nasal swabs on the microbial landscape and viruses were analyzed. All children were examined by an ophthalmologist using a slit lamp.
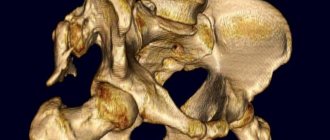
In the presence of chronic foci of infection, patients consulted an ENT doctor or dentist. An X-ray or ultrasound examination of the joints was performed. The level of total carnitine in the blood was determined by the enzymatic method using commercial kits. The study of the microelement composition of hair was carried out in the laboratory of the Center for Biochemical Research (St. Petersburg) using the method of atomic absorption spectroscopy (Karl Zeiss AAS-30 spectrometer). An indirect indicator of the breakdown of type 1 collagen (beta-Cross laps test) and the intensity of bone formation (osteocalcin, total aminoterminal propeptide of type 1 collagen, TPINP) were determined using the Elecsys test system. Bone densitometry of the lumbar spine was carried out using dual-energy X-ray absorptiometry DXA (L2-L4) using an osteodensitometer equipped with a “children’s” program. The obtained data were processed using statistical methods (c2, Student's test) using the SPSS 16 statistical package.
Results and discussion
A moderate degree of severity of CTD was diagnosed in 25 out of 106 examined children, in the rest (81 people) it was severe. Using statistical research methods, it was found that in children with arthralgia, changes in the skin (tender, hyperelastic), thin (pronounced venous pattern), hemorrhagic syndrome (tendency to nosebleeds, increased “bruising”), severe hypermobility and subluxations were significantly more common. joints, flat feet, “straight back” syndrome, a tendency to form “corns” or hygromas and hallux valgus. The anamnesis of these children significantly more often contained indications of hip dysplasia and a tendency to frequent viral and bacterial infections. When examining patients in this group, asymmetry in the length of the lower extremities, cracking in the joints, asthenic type of constitution, and poor tolerance to physical activity were revealed with greater frequency than in the control group (). Children with arthralgia were significantly more likely to be diagnosed with biliary dyskinesia, mental and behavioral (asthenic, affective, panic) disorders.
The results of the study are presented in.
The presented data clearly demonstrate that children with hypermobility syndrome also have other signs of connective tissue dysplasia, which must be taken into account in the differential diagnosis of the causes of HS. In addition, they were significantly more likely to have signs characterizing tissue vulnerability and a tendency to hemorrhage. This may explain the fact that most children had joint pain associated with physical activity or injury. Often, the prerequisite for the appearance of arthralgia was overstretching of the ligamentous apparatus of the joints, for example, when performing “bridge” and “split” exercises.
In young children, joint pain was usually provoked by prolonged walking in uncomfortable or poorly worn shoes, especially in cases of planovalgus foot deformity. Children are characterized by an acute onset of the disease, which is manifested by sudden lameness and a virtual absence (due to age) of complaints of joint pain. In adolescents with HS, the cause of arthralgia was most often a reaction from the periarticular soft tissues, which arose as a result of microtraumatization of tendons and ligaments, even with minor physical exertion, with the subsequent development of mild inflammatory phenomena. In a number of subjects, arthralgia arose against the background of changes in meteorological conditions or hormonal status.
According to our observations, arthralgia in children often imitated bone pain and was often combined with severe osteopenia. In this situation, densitometry was decisive in the differential diagnosis of pain syndrome. In our study, the incidence of decreased bone mass as determined by densitometry was approximately the same in both groups. In the group of children with arthralgia, 28 children were examined, a decrease in bone mass was detected in 17 (60.7%), in the group without arthralgia, 19 children were examined, a decrease in indicators was recorded in 12 people (63.15%).
A number of children experienced somatization of conflicts in the family and school, which was also typical for young children. So, for example, if a second child appeared in the family, then in order to attract attention, the children complained of pain in their legs. Almost half of the patients with arthralgia were found to have foci of chronic infection.
The main manifestations of HS syndrome in children were complaints of pain in the joints (usually the knees, somewhat less frequently the hips, ankles, etc.), lameness, dysfunction of the joints, poor tolerance to physical activity, and the inability to travel long distances.
In one group of children, joint pain occurred more often in the evening. They were quite intense in nature and sometimes led to short-term contracture of the joint. Another group of our patients had intermittent complaints of joint pain, usually after physical fatigue, in the afternoon, at night, or less often in the morning. The pain was not constraining in nature and, despite its pronounced intensity, the range of motion in the joints was most often completely preserved.
All patients with joint pain had no other signs of inflammation, such as joint swelling, increased local temperature, etc.
In 4 out of 47 (8.5%) children with arthralgia, asymmetry in the length of the lower extremities was identified, which led to static disorders and, as a consequence, to local dysplasia of the hip joint, which was always accompanied by varying degrees of scoliosis. Almost all (85.1%) were diagnosed with flat feet, which is one of the significant causes of pain. Therefore, a large place in the treatment of arthralgia is given to the correction of flat feet.
X-ray examination of the joints in children of this group did not reveal any pathology. However, during an ultrasound examination of the joints in 11 children, dystrophic changes in the cartilaginous structures were noted. Laboratory examination indicators indicated the absence of an inflammatory process.
Based on the results of a laboratory examination of the parameters of collagen synthesis and breakdown in children of both groups with CTD, the majority showed signs of increased synthesis and breakdown of bone collagen. However, there are no significant differences in the indicators of collagen metabolism in groups of children with CTD, differing in the presence or absence of arthralgia.
The results of a study of the content of microelements in hair in comparison with their safely acceptable levels (NOS) in children are presented.
The results of the study showed that more than half of the examined children with CTD have varying degrees of deficiency of macro- and microelements (magnesium, calcium, iron, zinc, silicon, manganese, copper, selenium), which are involved in the synthesis and maturation of collagen fibers, proteoglycans, mineralization bone tissue, as well as stabilizing the cell membranes of numerous connective tissue components. We did not obtain significant differences in the content of macro- and microelements in the groups of patients with CTD depending on the presence or absence of arthralgia.
In 20 children with complaints of joint pain, the level of carnitine in the blood serum was determined ().
The results of the study indicate a significant decrease (compared to the group of children who did not have signs of CTD) in the content of total carnitine in children with GHS, which confirms the presence of secondary mitochondrial deficiency in them.
Thus, the studies conducted in children with hypermobility syndrome revealed a significant decrease in the level of most macro- and microelements, total carnitine in the blood serum, an impairment in the synthesis and breakdown of collagen, which requires appropriate metabolite correction.
To correct microelement deficiency, microelement preparations can be used. To stimulate collagen metabolism in the absence of calcium oxalate crystaluria - vitamin C, magnesium salt of orotic acid in combination with piascledine, chondroprotectors and amino acids (L-lysine, L-proline).
In case of carnitine deficiency, it is necessary to use the drug Elkar 20% (L-carnitine). Studies conducted at the Pediatric Medical Academy (St. Petersburg) showed the high effectiveness and safety of the Elkar drug. For children, Elkar is prescribed at a dose of 30–50 mg/kg body weight per day in 2 divided doses. The course of treatment is 1 month.
Literature
- Skalny A.V. Reference values for the concentration of chemical elements in hair obtained by ICP-AES // Microelements in Medicine, 2003, No. 4, p. 55–56.
- Nikolaeva E. A., Semyachkina A. N., Vozdvizhenskaya E. S. et al. Correction of carnitine deficiency in children with hereditary metabolic diseases // Pediatric Pharmacology, 2003, No. 4, pp. 1–4.
- Kadurina T.I., Abbakumova L.N. Assessment of the severity of undifferentiated connective tissue dysplasia in children // Medical Bulletin of the North Caucasus, No. 2, 2008, p. 15–21.
- Kadurina T. I., Gorbunova V. N. Connective tissue dysplasia. Guide for doctors. "Elbi-SPb", 2009. 704 p.
T. I. Kadurina *, Doctor of Medical Sciences, Professor L. N. Abbakumova **, Candidate of Medical Sciences, Associate Professor
*MAPO, **SPbGPMA, St. Petersburg
Diagnosis of muscle weakness and treatment
If you have muscle weakness, you should consult a doctor, who will primarily be interested in answers to the following questions:
- How did muscle weakness appear and when?
- Is there a dynamic of muscle weakness, both increasing and decreasing?
- Is there a change in general health, weight loss, or have you recently traveled abroad?
- What medications is the patient taking and has anyone in the patient’s family had muscle problems?
The doctor will also need to examine the patient to determine which muscles are affected by weakness and whether the patient has true or suspected muscle weakness. The doctor will check to see if there are signs that the muscles feel softer to the touch (which may be a sign of inflammation) or if the muscles tire too quickly.
The doctor should then perform a nerve conduction test to determine if there is any abnormality in the conduction of the nerves into the muscles. In addition, the doctor may need to test the central nervous system, including balance and coordination, and may order laboratory tests to determine changes in hormone levels, electrolytes, and other parameters.
If this does not allow determining the cause of muscle weakness, then other diagnostic methods may be prescribed:
- Neurophysiological studies (ENMG, EMG).
- Muscle biopsy to determine the presence of morphological changes in the muscles
- Tissue scanning using CT (MSCT) or MRI in areas of the body that may affect muscle strength and function.
The combination of medical history data, symptoms, objective examination data and the results of laboratory and instrumental research methods allows, in most cases, to find out the true cause of muscle weakness and determine the necessary treatment tactics. Depending on the genesis of muscle weakness (infectious, traumatic, neurological, metabolic drug, etc.), treatment should be pathogenetic. Treatment can be either conservative or surgical.
The ligamentous apparatus is weak. Treatment of HMS syndrome
Treatment of a patient with HMS syndrome depends on the specific situation.
The variety of manifestations of the syndrome also requires a differentiated approach to each individual patient. An important point is to explain in an accessible form the causes of his joint problems (“weak ligaments”) and convince the patient that he does not have a serious illness that threatens inevitable disability. For moderate arthralgia this is sufficient. Recommendations to eliminate stress that causes pain and discomfort in the joints will be useful. Decisive in the treatment of severe pain are non-drug methods, and first of all, optimizing lifestyle. This involves matching the loads and the threshold of their tolerance for a given patient. It is necessary to minimize the possibility of injury, which includes vocational guidance and the exclusion of team sports. For persistent pain in one or more joints, elastic orthoses (knee pads, etc.) are used. Timely correction of detected flat feet is very important. At the same time, the doctor is required to have basic podological knowledge - the shape and rigidity of the insoles is determined individually, and the success of the treatment largely depends on this. It is often possible to cope with persistent arthralgias of the knee joints using this only method.
In ensuring the stability of the joint, not only the ligaments play a significant role, but also the muscles surrounding the joint. If it is impossible to influence the condition of the ligamentous apparatus through exercises, then strengthening and increasing muscle strength is a real task. Gymnastics for GMS syndrome has a peculiarity - it includes so-called “isometric” exercises, during which significant muscle tension occurs, but the range of motion in the joints is minimal. Depending on the location of the pain syndrome, it is recommended to strengthen the muscles of the thighs (knee joints), shoulder girdle, back, etc. Swimming is useful.
Drug therapy is applicable as symptomatic treatment for arthralgia. Since the pain associated with GMS syndrome is mainly non-inflammatory in nature, it is often possible to see a complete lack of effect from the use of non-steroidal anti-inflammatory drugs.
In this case, greater results can be achieved by taking analgesics (paracetamol, tramadol). Intra-articular administration of corticosteroids in the absence of signs of synovitis is absolutely ineffective.
For periarticular lesions (tendinitis, enthesopathies, bursitis, tunnel syndromes), treatment tactics are practically no different from those in ordinary patients. In moderate cases, these are ointments with non-steroidal anti-inflammatory drugs in the form of applications or compresses; in more persistent cases, local administration of small doses of glucocorticosteroids that do not have a local degenerative effect (suspension of methylprednisolone crystals, betamethasone). It should be noted that the effectiveness of local corticosteroid therapy largely depends on the correctness of the topical diagnosis and the technique of performing the procedure itself.