Juvenile arthritis in children (JRA) is a general name for a group of joint diseases in patients under the age of 16 years. Often this term refers to childhood rheumatoid arthritis, the main cause of disability in children and adolescents with musculoskeletal disorders.
In Russia, juvenile arthritis in children is quite common. According to statistics, every thousand child is affected by it. The disease does not spare even infants. Children's juvenile arthritis is more common among girls (about 2 times).
After the first episode, the disease progresses rapidly, so early diagnosis in juvenile arthritis is critical.
Causes of juvenile arthritis in children
Children's juvenile arthritis (also rheumatoid, idiopathic) is a multifactorial disease. Scientists associate its occurrence with environmental conditions, genetic characteristics and even infections. It has not yet been possible to unambiguously establish the causes of juvenile arthritis in children, but a certain connection with heredity and the patient’s medical history has been identified. Arthritis occurs more often in children whose families have a history of rheumatoid diseases.
Juvenile arthritis in children is classified as an autoimmune disease because it has a systemic effect on the child’s body. The patient's immune cells mistakenly perceive his own cells as “enemy”, pathogenic agents, and attack them. In this case, the integrity of the connective tissue is disrupted. The joints are most often affected, but the disease actively affects the eyes, heart, lungs, kidneys, digestive and other systems of the body.
Juvenile arthritis in adolescents and children can “sleep” for years, waiting for an immune surge, so it is important to distinguish it from reactive and other types of arthritis that can worsen in childhood and adolescence due to illness.
Where is the research being conducted?
Hardware scanning is available in any clinic that has the necessary equipment.
You can book the necessary procedure on the website of the unified appointment service, or by calling the consultation center, the number of which is also posted on each page of the portal.
Select the name of the service, clinic (by address, prices or rating), reserve time for a session and receive a special discount from the service.
Symptoms of juvenile arthritis in children
A distinctive symptom of juvenile arthritis in children is the presence of constant pain (aching, shooting, bursting) in the elbow, shoulder or knee joints. Less commonly, juvenile arthritis begins in the ankle and metatarsal joints, lumbosacral spine, wrist and other joints of the hands. In juvenile chronic arthritis in children, the lesions are almost always symmetrical.
Symptoms differ depending on which lesions predominate - articular or articular-visceral. The articular-visceral form means that the child has pathological changes in the internal organs. In both cases, the inflammatory process lasts in children for a long time - at least 6 months.
In the articular form (about 3-4 out of 5 cases), the following symptoms of juvenile arthritis in children are observed:
- change in gait;
- pain in the joints (especially in the morning) - sometimes acute, in which even wearing clothes causes pain;
- noticeable stiffness and limitation of mobility in the joint, caution of the child in movements, various disorders of motor activity;
- deformation of the joint, sometimes its spherical or spindle-shaped shape;
- swelling in the area of the affected joints;
- crunching in joints;
- weakness and dystrophic changes in muscles (affected limb or whole body);
- local temperature increase.
The articular-visceral (systemic) form of childhood juvenile arthritis can manifest itself:
- pallor of the skin (with redness of the skin over the sore joint);
- the appearance of ulcers or unhealthy pigmentation on the skin;
- general swelling of the body;
- fever and chills;
- heart rhythm disturbances;
- enlarged lymph nodes;
- breathing problems;
- abdominal pain;
- redness of the eyes and conjunctiva, blurred vision, uneven pupils;
- cough (including with sputum);
- a pinkish rash without itching on the body or in the area of the affected joint - may resemble stripes or stains, spots.
Older children are already able to tell adults what and where it hurts. Juvenile arthritis is the easiest to diagnose in teenagers.
In children from 1 to 3 years old, the presence of an inflammatory process is usually determined not by the child’s words, but by observing his behavior. Therefore, it is important to know the symptoms, causes and treatment of juvenile arthritis in children. A child suffering from JRA becomes inactive. If he needs to carry out some tasks related to movement, he may become capricious or irritated. Often the child tries to press, “rock”, warm, cover, hide the affected joint, noticeably worries even when accidentally touching it, and takes forced poses. On the side, lameness and swelling of the joints are also observed.
Little patients with childhood juvenile arthritis refuse to stand on their feet for a long time. They have a hard time with educational games and sitting on the potty.
Other symptoms include:
- rapid fatigue unusual for a child;
- weight loss and poor appetite;
- low-grade or high temperature (up to 40°C).
As juvenile arthritis progresses in children, deformities in the joints and growth retardation become noticeable. Exacerbation of JRA with greater or less intensity occurs against the background of almost any infection.
Symptoms of knee arthritis
Clinical manifestations of gonarthritis tend to gradually progress as the disease develops; minor trauma or excessive stress leads to a worsening of the condition.
The left knee joint is affected less frequently, since in most people the leading limb is the right, and it bears the main load. Early diagnosis allows you to identify the disease at an early stage before the first signs and exacerbation stages appear. The most common signs of knee arthritis are:
- pain in the joint during active activities and then at rest, limited range of motion, morning stiffness, gait disturbance
- swelling
- sound phenomena - clicks. crunch
- local temperature increase
- inability to kneel due to pain
- joint deformity
- stiffness after prolonged sitting
- paresthesia in the area of inflammation
Diagnosis of juvenile chronic arthritis in children
A rheumatologist can help diagnose juvenile arthritis in children by examining the patient, interviewing him and his parents, as well as laboratory and instrumental studies.
Among the first tests carried out are the following:
- general and biochemical blood test;
- immunological analysis;
- analysis for rheumatoid factor;
- analysis for the presence of antinuclear factor.
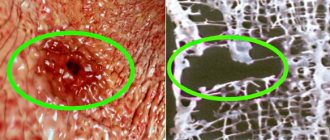
For differential diagnosis and identification of visceral complications of juvenile arthritis in children (systemic lesions), computed tomography, magnetic resonance imaging, electrocardiography, ultrasound, x-ray of joints and chest, and tuberculin test may be prescribed. All children undergo a mandatory examination by an ophthalmologist using a slit lamp.
Clinically and laboratory-wise, pediatric rheumatoid arthritis differs from adults and is diagnosed mainly before the age of 4 years.
Treatment of juvenile arthritis in children
Treatment of juvenile arthritis in children includes drug therapy, therapeutic exercises, orthopedic regimen, healthy daily routine and a nutritious diet.
It is aimed at stopping the inflammatory process, combating systemic manifestations and organ damage, destructive changes in joints, as well as maintaining normal mobility in the joints
Depending on the form and rate of progression of the disease, juvenile arthritis in children is treated on an outpatient or inpatient basis.
Treatment of juvenile arthritis in children with drugs
The main tool in the treatment of juvenile arthritis in children is immunosuppressive therapy. Parents are often frightened by this name, because immune suppression is perceived as an a priori bad effect. However, in conditions where high immunity becomes the cause of a child’s disability, it is important not to delay or interrupt the use of immunosuppressants. Otherwise, the disease may worsen and develop into a series of almost continuous relapses.
The following immunosuppressants are used as basic therapy:
- methotrexate;
- adalimumab;
- infliximab;
- cyclophosphamide.
Non-steroidal anti-inflammatory drugs (NSAIDs) are also used to relieve inflammation, pain and fever in juvenile arthritis in children:
- meloxicam;
- indomethacin;
- diclofenac;
- piroxicam;
- ibuprofen;
- etoricoxib;
- ketoprofen.
In especially severe cases, the doctor prescribes hormonal glucocorticoid drugs (GC):
- prednisolone;
- methylprednisolone;
- hydrocortisone;
- betamethasone.
Uncontrolled use of both of these medications without a doctor’s prescription can lead to stomach ulcers and severe endocrine disorders in a child.
In the vast majority of cases, drugs are taken for life (immunosuppressants) and in regular courses (NSAIDs, GCs) - in tablets, in the form of ointments, creams, intramuscular and intra-articular injections. If they are also ineffective, genetic engineering biological therapy is prescribed for the treatment of juvenile arthritis in children.
Non-drug therapy for juvenile arthritis
To relieve symptoms and preserve joint function in children, the following is used:
- mud therapy (usually in a sanatorium);
- ultra-high frequency therapy;
- magnetic therapy;
- ultrasound therapy;
- paraffin therapy and more.
In the acute phase of juvenile arthritis in adolescents and children, joint immobilization using splints and other orthoses, as well as bed rest, are indicated. Orthopedic insoles and other devices are widely used.
During remission, exercise therapy and therapeutic massage have a positive effect on the child’s musculoskeletal system.
In case of severe destruction of the joint, surgery to replace it is indicated.
Causes of pathology
The sources of the disease in the medical literature are divided into two groups: infectious and autoimmune (aseptic). The first group includes the following pathogens that can cause arthritis of the knee joint in children:
- coccal infections;
- coli;
- Candida fungi;
- protozoan microorganisms;
- tuberculosis bacillus.
An aggressive “agent” enters the joint zone from the outside (as a result of injury), and the primary form of the disease develops. If a microorganism or fungus enters the synovial cavity through the blood, a secondary infection occurs.
The second group is formed by autoimmune inflammatory reactions, when the patient’s body is affected for a long time by other infections or foreign proteins. In this case, your own immune system begins to attack the tissues of your own body. There are several forms of pathology:
- Reactive. Characterized by a reaction to streptococci, gonococci or chlamydia.
- Post-vaccination. It is formed after a routine vaccination, when an immune response is received by foreign proteins introduced with the solution.
- Allergic. Increased sensitivity to certain microscopic stimuli.
- Juvenile lesion. It has no clinical explanation, but the primary disorder occurs in the synovium.
- Systemic arthritic disorders. They act as a complication of other diseases (psoriasis, lupus, diabetes, etc.).
Unfavorable factors also include frequent or severe injuries, previous surgery, incorrect treatment of ARVI, genetic predisposition, and congenital damage to the described area.
Prognosis for juvenile chronic arthritis in children
Juvenile rheumatoid arthritis is a disease that tends to progress rapidly. The activity of the disease depends on the form of onset of the disease - in one joint, in 2 or 3 or in multiple joints at the same time. If the disease begins in the form of polyarthritis (symptoms are observed in 4 or more joints), the number of affected joints increases over time.
The number of children requiring mobility and/or self-care assistance has decreased significantly over the past decade. In 95% of cases, treatment avoids disability. Among the remaining 5% there are still children with early onset of the disease, positive rheumatic factor. Juvenile arthritis in adolescents has fewer consequences than in early childhood. Every 7-10 patients suffering from inflammation of the uvea are at risk of losing their vision.
The following features indicate an unfavorable prognosis for juvenile chronic arthritis in children:
- acute course with fever and active progression of the disease within six months;
- the need for rapid re-administration of systemic GCs;
- inflammation of the serous membranes;
- localization of the disease in the hip joints;
- erosive destruction of joints and narrowing of the lumen of the joint space.
In more than half of the cases, with timely consultation with a doctor and lifelong therapy, severe destruction of the joints can be avoided. Under favorable circumstances, the child can attend school on an equal basis with peers, dance and participate in sports games in a gentle manner, with minimal restrictions. With juvenile arthritis in children, doctors and parents are increasingly able to achieve a full life for the child. Early contact with a doctor contributes to drug-free remission - that is, the patient does not need to constantly receive therapy.
Clinical guidelines for juvenile arthritis in children
The condition of the tissues and the nature of the lesions in juvenile arthritis can worsen and change. Therefore, clinical recommendations for juvenile arthritis in children necessarily include routine follow-up with a doctor and regular examinations to monitor the condition.
When the disease has been put into remission, it is important to follow the following rules to prevent exacerbations:
- have less contact with animals, people and surfaces on which infectious agents may be present;
- follow sanitary and hygienic recommendations in the room where the child lives, as well as in cases where one of the family members is sick;
- avoid hypothermia and prolonged exposure to the sun;
- if possible, avoid moving and traveling to regions with a different climate (to avoid acclimatization symptoms);
- Do not allow vaccination (except for the Mantoux test) and take immunostimulating drugs without consulting your treating rheumatologist.
Parents should ensure that the child does not attend educational institutions “undertreated” until all symptoms of infectious diseases disappear. Clinical guidelines for juvenile arthritis in children should be followed throughout life.
Be vigilant and let your children stay healthy!