Osteoporosis
(some call it “bone osteoporosis,” which is incorrect, since the word already contains the root “osteo,” which means “bone”) is a disease that is systemic and progressive, the main symptom of which is a decrease in density and disruption of the structure of bone tissue. Decreased bone density leads to an increased likelihood of developing fractures. A characteristic feature of osteoporotic fractures is their occurrence due to minor loads. It is the ease of fractures that is the main danger in osteoporosis, since extremely important bone structures of the human body - the spine, the femoral neck - can be susceptible to fractures. Fractures lead to immobility of the patient, which in old age is fraught with a significant number of complications - from the appearance of bedsores to the development of congestive pneumonia, which can be life-threatening. Few people know, but osteoporosis is now the fourth leading cause of death in people - it is second only to cardiovascular diseases, tumors and diabetes. And the main cause of death in patients with this diagnosis is a fracture of the femoral neck.
Causes of osteoporosis
- postmenopausal osteoporosis
in women (associated with low production of female sex hormones after menopause; the vast majority of women over 60 years of age describe its symptoms); - senile osteoporosis
is a broader concept than menopausal osteoporosis. The aging of the human body is accompanied by disruption of the internal structure of a significant number of organs, including bone tissue. It is the general aging of a person that causes a decrease in bone strength in old age; - glucocorticoid osteoporosis
develops in patients receiving long-term treatment with glucocorticoids - hormones of the adrenal cortex and their synthetic analogues, one of the side effects of which is disruption of the functioning of bone tissue; - secondary
is called
osteoporosis,
the cause of which is any chronic serious disease; Moreover, osteoporosis is one of the symptoms or complications of a primary disease - that is why it is called secondary, it seems to develop second. The cause of secondary osteoporosis can be diseases such as diabetes mellitus, malignant tumors, chronic kidney disease with the development of renal failure, some lung diseases, thyrotoxicosis (excessive thyroid function), hypothyroidism (reduced thyroid function), chronic hepatitis, parathyroid adenoma ( primary hyperparathyroidism). Also, the cause of its development may be a long-term deficiency of calcium and vitamin D in food - this disrupts the flow of calcium into the blood, and therefore the body’s needs for calcium are met at the expense of reserves in the bones. The result is osteoporosis.
Benefits of Bee Products for Bone Health
Not only plants can have a positive effect on the condition of bone tissue. Modern researchers have discovered a unique ability to restore the balance of sex hormones in some bee products. For example, drone jelly (drone brood).
It contains insect sex hormones. They, of course, cannot replace a person’s own hormones, and therefore there is no talk of any hormone replacement therapy when taking them. What they can really do is stimulate the sex glands to produce their own sex hormones.
Researcher from the Beekeeping Research Institute (Ryazan region), Ph.D. Burmistrova L.A. showed that drone jelly has a gonadotropic effect. She gave bee product to unilaterally castrated male rats whose testosterone levels were 10 times lower than normal. This made it possible to restore the androgen concentration in animals to the original level.
What’s surprising: ancient Chinese emperors used the ability of drone jelly to increase testosterone levels long before modern research. They used the bee product to gain “the strength of a lion” or, in modern terms, to increase potency. As we now know, testosterone is needed not only for potency, but also for strong bones and much more.
In addition to bee hormones, drone milk is rich in other substances necessary for the restoration of bone tissue: vitamins, minerals, amino acids, poly- and monounsaturated fatty acids. It’s just that it’s difficult to preserve them for a long time: at normal room temperature, the bee product spoils within two hours; it can be stored in the refrigerator for no more than a day. As for the freezer, during freezing/thawing, a significant part of the valuable components is destroyed.
Mechanism of development of osteoporosis
In bone tissue, two mutually opposite processes constantly coexist - osteogenesis (formation of bone tissue) and resorption (destruction) of bone tissue. Bone is a living structure that provides important support and organization functions to the human body. The human bone is a complex network of interconnected and intersecting bone beams, the direction of movement and strength of which make it possible to counteract the mechanical loads acting on the bone as a whole (the weight of the bone and muscles, the weight of internal organs and external loads, loads due to body position or acting on external acceleration, etc.). The nature of loads changes throughout a person’s life - body weight changes, height often changes with age, the nature of activity changes - all this forces the bone to adapt to new conditions and remain resistant to the forces acting on it. Bone beams are destroyed in one place and formed in another - this process is called bone remodeling and occurs constantly.
Special cells, osteoclasts, are responsible for the destruction of bone tissue during remodeling, which, like bulldozers, “bite” into bone tissue and destroy it. The formation of new bone beams is carried out by “mason” cells, osteoblasts, which form new bone tissue - the bone matrix, into which calcium salts are deposited, ensuring the strength of the constructed structure.
Increased bone resorption processes combined with weakened bone formation processes are the main cause of the development of osteoporosis. Osteoporosis occurs when old bone tissue is destroyed and new bone tissue is formed in insufficient quantities. Also, the reason for its appearance may be insufficient intake of calcium salts into the bones - in this case, the bone becomes soft and ceases to perform frame and supporting functions.
It should be remembered that the causes of osteoporosis are always directed against the formation of new bone, or “help” the destruction of bone tissue - both of which ultimately lead to fractures.
Hip joint
Calcium deficiency can cause discomfort and/or pain in the hip joint after bending forward, backward and/or turning the body to the right and left. The pain intensifies after physical activity and does not subside for a long time at rest. When visiting a doctor, a diagnosis was made - osteoporosis of the hip joint. In addition to medications prescribed by the attending physician, for the purpose of therapeutic prevention, the disease can be treated with folk remedies. The following methods of alternative treatment will help get rid of pain symptoms and compensate for the lack of calcium in the osteoarticular hip joint:
- a remedy for men in case of decreased bone mass due to testosterone deficiency. Pour a tablespoon of chopped dry plant product (one of your choice) - calamus, celery, woodruff or field grass - with ½ glass of boiled water. The healing product is infused for 12 hours. Take home medicine in equal portions 3 times a day before meals;
- In case of hormonal imbalance, it is effective to carry out drug treatment of osteoporosis in women using the following traditional medicine recipe. A tablespoon of dry and crushed medicinal plant (one of your choice) - horehound, alfalfa, red clover, sage or fenugreek - is brewed with two glasses of boiling water. The medicine is infused for 30-40 minutes. Take one glass daily for a month on an empty stomach.
Risk factors for osteoporosis
In childhood and adolescence, the process of bone tissue formation significantly prevails over its resorption. The older a person gets, the more bone destruction begins to prevail over its formation. The process of bone resorption intensifies especially in women after menopause. That is why osteoporosis in women is a typical and very common disease that occurs in old age.
There are factors that increase the risk of developing osteoporosis:
- female gender (women are much more susceptible to this disease than men);
- osteoporosis in blood relatives in the family (genetic predisposition to this disease is very important);
- age (as we mentioned earlier, with age the likelihood of developing the disease increases significantly);
- low mobility (immobilization, fixation of the patient’s limbs or body in case of injury, significant patient weight, mental disorders that make movement difficult - all these conditions are causes of the development of osteoporosis);
- drug therapy using glucocorticoids, high doses of thyroxine (a synthetic analogue of the thyroid hormone); bone tissue is also negatively affected by long-term use of aluminum-containing drugs - for example, antacids used to reduce the acidity of gastric juice during gastritis or peptic ulcers;
- the patient is overweight or underweight.
The patient cannot always change anything about the causes of osteoporosis, even if he understands that they can be dangerous. Indeed, neither gender nor age (the main risk factors) can be changed. However, there are factors that the patient can and should change in order to reduce the risk of developing such a dangerous disease. Smoking, excess consumption of alcohol and caffeine-containing drinks, lack of exercise, low consumption of foods rich in calcium (for example, dairy), little sun exposure, insufficient vitamin D intake - all of these factors can be changed, which is why they are called modifiable factors. risk.
Folk recipe
Before you begin to treat osteoporosis with home therapy, you need to make sure that your body does not have an allergic reaction to certain types of food and medicinal plants.
Let's consider the most popular and effective traditional medicine recipes that help with osteoporosis of a particular musculoskeletal segment of the skeletal frame.
Osteoporosis - symptoms and signs
Unfortunately, osteoporosis is a hidden disease that occurs for a long time without noticeable symptoms, and therefore its diagnosis is often delayed. Very often, the first symptom is a fracture - only after the fracture does the patient begin the examination and learn that the cause of the injury was osteoporosis.
At the same time, there are symptoms that make it possible to notice this disease at an earlier stage, before fractures appear. Patients are often concerned about changes in posture, stooping, decreased height, and accelerated destruction of dental tissue. Bone pain is one of the important signs to suspect the development of osteoporosis. Most often, pain occurs in the spine, hip bones, bones of the forearms and wrist. Often the pain intensifies with prolonged exposure to an uncomfortable position or mechanical stress. When there is a fracture or a sharp decrease in the height of the vertebrae, the pain is localized in the back, between the shoulder blades, and in the lumbar region. A symptom of calcium deficiency in the blood may be the appearance of convulsive muscle contractions.
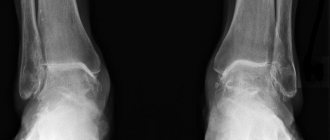
Diagnosis of osteoporosis
Currently, diagnosing osteoporosis does not present significant difficulties. We only need to remember that traditional radiography is not able to assess the degree of development of osteoporosis, so other methods are used for diagnosis. Radiography allows one to only suspect the presence of osteoporosis based on a characteristic change in bone density on X-ray images, however, to plan treatment and assess the dynamics of changes in bone density, it is necessary to have quantitative information about the condition of the bone - i.e. it is necessary to be able to express bone density digitally.
Quantitative assessment of bone density is central to the diagnosis of osteoporosis. For this study, a special term was invented - “densitometry”,
those. density measurement. It is often written differently – “osteodensitometry”, emphasizing that bone density is measured.
Densitometry can be of three main types:
- X-ray densitometry (synonyms: DEXA, dual-energy X-ray computer densitometry);
- computed tomographic densitometry;
- ultrasonic densitometry.
With X-ray densitometry
X-rays of bones are taken at standard points (usually there are three standard points: femoral neck, lumbar spine, radius). After receiving the X-ray image, a special computer program calculates the bone density in the area of interest to the doctor and compares it with indicators characteristic of a healthy person of the same age (this is called the Z-index) or for a healthy person aged 40 years (this indicator is called the T-index ).
Diagnosis of osteoporosis
is carried out according to the deviation of the T-index from normal values:
- from 0 to -1 – normal bone density;
- from -1 to -2.5 – osteopenia (loss of bone tissue);
- less than -2.5 – osteoporosis.
With computed tomographic densitometry
Computed tomography is performed on a multislice tomograph, followed by calculation of bone density and comparison with the reference one. As a result, the density of 1 cubic centimeter of bone tissue in the study area is calculated, and the T- and Z-indices are calculated. The advantage of computed tomographic densitometry is its high accuracy and the ability to calculate bone tissue density regardless of the patient’s weight, the presence of adhesions, and metal structures, which can make it difficult to obtain results with conventional X-ray densitometry. The disadvantage of densitometry on a tomograph is the increased radiation exposure to the patient’s body.
Ultrasound densitometry
carried out by measuring the speed of passage of an ultrasonic wave through bone tissue. It has been proven that a decrease in bone density makes it looser and does not allow the bone to quickly conduct sound waves. The lower the bone density, the slower the sound wave travels along the surface of the bone. The ultrasound densitometer is equipped with special sensors for measuring the speed of ultrasound along the surface of the bones, and the built-in software of the device allows you to calculate bone density with the determination of T- and Z-indexes.
Ultrasound densitometry uses superficially located bones to determine density - the phalanges of the fingers, the radius on the forearm, the anterior surface of the tibia, the fifth metatarsal bone on the foot. The indicators calculated using ultrasound densitometry (T- and Z-indices) can be compared with similar indicators obtained from X-ray densitometry (that is, if osteoporosis was detected during X-ray densitometry, then ultrasound densitometry will reveal the same changes). At the same time, if the patient underwent X-ray densitometry during the first study, which revealed osteoporosis, and then treatment for osteoporosis was prescribed, then the second study should be carried out using the same assessment method, that is, also X-ray densitometry - only in this case will it be most reliable evaluate the effectiveness of treatment. Of course, the same rule applies to ultrasound densitometry - if treatment is carried out based on the results of the initial ultrasound examination, then monitoring of the treatment results should be carried out using ultrasound densitometry.
Diagnosis of osteoporosis using ultrasound densitometry has a number of advantages - ultrasound densitometry is not accompanied by radiation and can be carried out in a convenient environment for the patient for a fairly short time. The safety of the study is so high that ultrasound densitometry can be performed on both children and pregnant women.
In short, densitometry allows you to completely solve the problem of diagnosing osteoporosis, while any densitometry method is cheap, painless, and accurate.
Densitometry should be performed on all women aged 65 years
– following this simple rule could significantly reduce the incidence of fractures among older women. At the same time, densitometry is absolutely indicated for other groups of patients, including young patients. Among the indications for densitometry, the following should be noted:
- early onset of menopause;
- hormonal disorders in women, accompanied by estrogen deficiency, with the development of amenorrhea (absence of menstruation);
- low body weight (including due to a disease such as anorexia nervosa);
- presence of blood relatives suffering from osteoporosis;
- the presence of primary hyperparathyroidism (parathyroid adenoma);
- the presence of secondary hyperparathyroidism due to chronic renal failure;
- thyrotoxicosis (due to diseases such as diffuse toxic goiter, polynodose toxic goiter, toxic thyroid adenoma);
- decreased testosterone levels in men;
- long-term immobilization for fractures or other injuries;
- Itsenko-Cushing syndrome and disease;
- long-term use of glucocorticoids;
- the presence of rheumatic diseases (spondyloarthritis, rheumatoid arthritis), which are often combined with the development of osteoporosis.
It is important to understand that osteoporosis significantly complicates the treatment of joint diseases. Osteoporosis of the joints reduces the strength of the bones that articulate at the joint. Nowadays, endoprosthetics of hip and knee joints for arthrosis has become widespread. In this case, instead of a joint, the patient is fitted with a metal endoprosthesis, which is attached to the bones that form the joint. The stability of the resulting structure directly depends on the strength of the bones that bear the load of the endoprosthesis. The presence of osteoporosis of the joint creates preconditions for instability of the endoprosthesis, bone fractures in the area where the endoprosthesis is attached, and the development of severe complications. Therefore, diagnostics aimed at identifying osteoporosis is mandatory for all patients planning to undergo endoprosthetics.
Laboratory tests are of auxiliary importance in the diagnosis of osteoporosis. There are a number of markers (they are also called “osteoporosis tests”
), allowing to assess the severity of osteoporosis and the dynamics of its progression (osteocalcin, bone fraction of alkaline phosphatase, B-crosslaps, pyridinoline, etc.), however, their diagnostic significance is lower than the significance of densitometry.
When examining a patient with a suspected disorder of bone tissue density, important laboratory indicators are also mandatory:
- ionized calcium, parathyroid hormone, 25-hydroxyvitamin D;
- TSH, T4 St. (thyroid hormones);
- for women – sex hormones (estradiol, testosterone, etc.);
- for men – the level of free testosterone in the blood.
Specialist recommendation
The risk of osteoporosis should be addressed during the prenatal period of human development. An expectant mother should not neglect taking vitamin and mineral components, that is, be more attentive to the choice of foods that allow her to accumulate bone mass and mineralize it, in order to provide her child with a healthy future.
The problem of osteoporosis develops in a person from childhood, and in order to maintain strong bones, it is necessary to follow simple rules of therapeutic prevention throughout life:
- Quit smoking and alcohol.
- Saturate your body with enough calcium, phosphorus, magnesium and so on.
- Lead a physically active lifestyle.
Take care of yourself and always be healthy!
Treatment of osteoporosis
Currently, we can confidently say that the treatment of osteoporosis
should be carried out in specialized centers with significant experience in managing patients with this pathology. Osteoporosis is a complex multifactorial problem, the development of which is caused by endocrine, age-related, and behavioral factors; therefore, doctors of several specialties (endocrinologist, rheumatologist, cardiologist, neurologist) often take part in the treatment of osteoporosis. At the same time, one doctor must be in charge, must be the “conductor” of this orchestra, must know how to treat osteoporosis and determine examination tactics, as well as decide which specialists should be involved in consultations if necessary. Most often, this doctor is an endocrinologist - it is endocrinologists who most often treat osteoporosis these days.
The North-Western Center for Endocrinology, as a specialized endocrinology center, provides comprehensive diagnosis and treatment of osteoporosis in St. Petersburg, Vyborg and other cities of the Leningrad region. The center's endocrinologists independently perform ultrasound densitometry on patients, which allows them to quickly establish a diagnosis and determine how to treat osteoporosis, as well as objectively evaluate the results of the therapy.
The main goals in the treatment of osteoporosis are increasing bone mass (by increasing the deposition of new bone tissue and reducing the destruction of existing bone tissue), preventing the development of fractures, reducing or completely eliminating pain, and ensuring optimal motor mode for patients.
Treatment of osteoporosis consists of several important and interconnected stages:
- First of all, the main diseases that cause osteoporosis are treated (thyrotoxicosis, hypothyroidism, Itsenko-Cushing syndrome and disease, hypogonadism, etc.);
- therapy aimed at increasing bone mass (calcium preparations, vitamin D, drugs from the bisphosphonate group - Fosamax, Forosa, Fosavance, Zometa, Aklasta, Bonviva, etc.);
- drugs aimed at reducing the intensity of pain.
In this article, we will not dwell in detail on therapy aimed at treating the underlying disease, if any, as this will take too much time. Let's discuss the modern concept of treating osteoporosis, aimed at increasing bone mass.
Currently, combination treatment of osteoporosis using:
- vitamin D preparations (aquadetrim, vigantol), or activated forms of vitamin D (alfacalcidol, alpha D3-Teva, etalfa);
- calcium preparations (containing calcium carbonate or calcium citrate);
- drugs from the bisphosphonate group.
If the first two groups of drugs (vitamin D and calcium) are aimed at increasing the formation of bone tissue by increasing the supply of calcium to the patient’s body, then the second group (bisphosphonates) is aimed at suppressing bone resorption (bone breakdown). The main effect of bisphosphonates is to block the work of osteoclasts, the cells responsible for the destruction of bone tissue. Currently, even very long-term, up to 10 years, use of bisphosphonates is considered safe. The cheapest and most studied drug from this group is sodium alendronate (Fosamax, Forosa), which is taken once a week. Other drugs that appeared later allow you to take them once a month, or once every few months. Bisphosphonates for osteoporosis are the main “strike force” of doctors, due to their effectiveness and safety.
Correctly selected treatment for osteoporosis allows you to increase bone density by 5-10% per year, which greatly reduces the risk of developing fractures. It should only be recalled that this therapy is long-term, designed to last for years of use. You should not think that treatment for one or two months will give any noticeable result.
Folk remedies for osteoporosis
Before turning to drug treatment for osteoporosis, you should use simple, traditional methods. Such simple and affordable products as eggs, honey, lemons, milk, onions, carrots, garlic, and butter will help you with this. There is a wide range of medicinal plants for the treatment of this ailment and are used for internal use in the form of teas, mixtures, tinctures, as well as for compresses, lotions, and ointments. Let's look at examples of recipes for treating brittle bones and joints.
Shilajit will make your bones strong
One of the best medicines for osteoporosis is mumiyo. It is necessary to take it twice a day before meals (about 20 minutes), dissolving a pea the size of a match head in 70 ml of water. Admission period is 20 days.
Eggshells will increase bone density
The following recipe helps well with osteoporosis. 6 raw chicken eggs along with their shells are poured with juice obtained from 10 lemons. A week later, when the eggs have completely dissolved, the mixture is saturated with 300 grams of honey and an incomplete glass of cognac (150 g). The resulting drug should be stored in a dark place and consumed 1 teaspoon after meals.
Washed eggshells, ground to a powdery consistency, should be taken 2-3 grams every morning.
Walnut leaves improve immunity
To prevent brittle bones, a recipe for a drink made from dry nut leaves is suitable. 50 g of leaves are poured into a liter of boiling water and left for 10 minutes, filtered. Drink 3-4 glasses per day.
Birch buds heal fractures and sprains
A glass of fresh birch buds should be filled with a half-liter bottle of vodka and left to steep for a week. Apply a compress from the resulting infusion to the affected area every day at night. In parallel with this, you can use tablets or vitamins prescribed by the doctor to speed up the healing of the fracture.
Horsetail will strengthen bones
Prepare a decoction of 200 g of horsetail, knotweed and wild rosemary. Pour the herb mixture into a liter of water and simmer over low heat for 1 hour. Take 100 g every day for a month before meals.
100 g of dry horsetail mixture is poured into 1 liter of milk, brought to a boil, and then wrapped and left for 3 hours. The strained drink is consumed 3 times a day. Treatment should last 12 weeks.
Nasturtium will help cope with brittle bones
Brew 50 g of dried leaves of large nasturtium in 600 ml of boiling water. Strain the infusion and drink 1 glass with honey during meals. The best effect will appear when using this infusion in the winter season.
Calcium carbonate + milk + kefir + sour cream
To one part (0.5 liter) of milk heated to +70 degrees, add the same part of kefir and 100 grams of sour cream, as well as 10 g of calcium carbonate. Remove the well-heated but not boiled mixture from heat. Take daily for 2 months, several doses per day so that the daily norm is 100 g.
Dill with parsley
Grind 200 g of fresh dill and parsley, pour 0.5 liters of boiling water over it, leave for 3 hours, strain and consume 100 g 3-4 times a day. The drink helps strengthen bone tissue and is effective against atherosclerosis. This tea should not be taken by pregnant women.
Dream-grass with Chernobyl and Woodruff
Mix with hot water +70 degrees:
- 1 tbsp. l. sleep-herbs;
- 1 tbsp. woodruff;
- 2 tbsp. Chernobyl.
After an hour's tincture, take 50 ml, without straining, so that the daily dose is 0.5 liters. Duration of treatment is 3-6 months.
Dandelion infusion
Brew 1 tbsp. dry dandelion grass in a glass of boiling water, leave for 0.5 hours. Dosage: 70 ml 3 times a day for 3-6 months.
Dandelion contains calcium and antioxidants, protecting bones from age-related changes.
Clay water against osteoporosis
Clay water contains silicon, which is part of bones. For treatment, clay water is prepared, for which 1 table is dissolved in 150 ml of water. l. any clay. Use 70 ml 3 times. per day before meals for 3 weeks. Then you need to take a week's break and continue as usual for another 3 weeks.
Burdock flower oil
Burdock flowers are poured with vegetable oil and kept for several days in a dark place. Rub the finished oil on the knees, joints, bones 1-2 rubles. for the day and also for the night.
Application: 2-3 months.
Larkspur (comfrey root)
The root is crushed and mixed with pork fat melted in a water bath, and left for a couple of days in the dark. This ointment is used to lubricate sore areas of the legs, arms, and lower back.
Pour 10 g of larkspur root into a glass of boiling water, add a few drops of Dimexide and infuse. Infusion is used to irrigate the affected areas 2 times. per day for a month.
Golden mustache+olive oil
Golden mustache with a set of microelements and vitamins has a beneficial effect on bone tissue and is a cure for osteoporosis, osteochondrosis, and atherosclerosis.
Preparation:
The crushed leaves and tendrils of the plant are poured with olive oil so that the plant is completely covered. The mixture is “simmered” in a water bath, infused and filtered. The ointment is used to lubricate sore bones and joints 2 times. per day for a month.
In addition to these plants, infusions of cinquefoil, alfalfa, horsetail, geranium, and juniper berries contribute to the absorption of calcium.
What diet is necessary for osteoporosis?
The diet for osteoporosis has no special secrets - you just need to ensure sufficient intake of vitamin D and calcium into the body, which are necessary for the formation of new bone tissue. The richest foods in calcium are dairy products, fish, cabbage (including broccoli), and various nuts. The main source of vitamin D in the body is fish (or fish oil). Significant amounts of vitamin D are produced in the skin when exposed to sunlight.
At the same time, when planning nutrition for osteoporosis,
It should be remembered that dietary “exercises” alone are not able to eliminate either calcium deficiency or vitamin D deficiency. In the vast majority of cases, diet is only one element of the treatment of osteoporosis and must be accompanied by taking calcium and vitamin D supplements in the form of tablets - this is the only way eliminate long-term chronic vitamin D deficiency.
Calcium containing products and herbal medicine
The daily requirement of vitamin D for an adult according to international standards is 100 IU (1 IU of vitamin D is the biological equivalent of 0.025 mcg of ergocalciferol). A person receives this vitamin energy booster, which ensures high-quality absorption of calcium, from ultraviolet sunlight and some food products. It is believed that sea fish and seafood are the best natural and natural source of vitamin D. However, you can replenish your vitamin reserve and saturate your body with calcium using other foods. The content of the mineral component in 100 g of product can be found:
- in dried fish bones – 3000 mg;
- in sesame – 1150 mg;
- in hard cheese – 650 mg;
- in gelatin – 500 mg;
- in soybeans – 230 mg;
- in porcini mushroom (dried) – 200 mg;
- in dried apricots – 175 mg;
- in green onions, sunflower seeds and milk – 100 mg;
- in garlic – 50-60 mg;
- in figs, raisins, carrots, white cabbage – 50 mg;
- in dates and dried apples – 40-45 mg;
- in egg yolk – 30-45 mg;
- in lemon – 35-40 mg;
- in potatoes – 10 mg.
A dietitian will help you balance your diet properly with calcium. Before treating bone osteoporosis with folk remedies, you should exclude products that enhance the removal of mineral components from bone tissue:
- flour and sweet products;
- salty foods;
- coffee, tea, cocoa;
- fatty foods;
- alcohol;
- carbonated drinks;
- food with coarse fiber.
Medicinal plants are also a vitamin energy source. The required amount of calcium can be found in nettle, burdock, comfrey, St. John's wort, dandelion, meadow clover, yarrow and other natural plant components.
Complications of osteoporosis
The main and most dangerous complication of osteoporosis is fractures. The most dangerous fractures are fractures of the vertebrae and femoral neck. At the moment, it is “thanks to” hip fractures that osteoporosis is in fourth place among the causes of death in the world (second only to vascular diseases, oncology, and diabetes mellitus). Osteoporosis of the spine leads to the development of compression fractures even when exposed to minor loads (for example, when falling from your own height, or when landing after a jump). It is important to understand that immobility following a fracture of the spine or femoral neck in a significant number of cases ends in bedsores, congestive pneumonia, infectious complications, and thrombosis. Only early surgical treatment can reduce mortality from hip fractures, but, unfortunately, it cannot be performed in many elderly patients due to the presence of severe concomitant pathology. Osteoporosis of the spine cannot be corrected by surgery at all. That is why the only effective method of treating osteoporosis is early diagnosis and combined conservative therapy - this is the only way to avoid the development of fractures.
How is osteoporosis prevented?
Prevention should include several areas aimed at eliminating the previously listed risk factors for osteoporosis.
It is important to ensure sufficient intake of calcium and vitamin D from food - for this you should eat dairy and other calcium-rich foods listed above. You should reduce your consumption of alcohol and caffeine-containing drinks and foods.
There are a number of scientific studies showing that long-term use of calcium and vitamin D supplements for the purpose of prevention can reduce the risk of developing osteoporosis. Taking moderate doses of calcium with vitamin D for 3-4 years does not lead to side effects, but can improve bone density. It is enough to take calcium carbonate in a dose of 500 mg with 200 IU of vitamin D twice a day (for example, calcium D3 Nycomed, 1 tablet 2 times a day; or Calcemin-Advance, also 1 tablet 2 times a day). Taking calcium and vitamin D supplements is safe even if you have urolithiasis. However, the issue of preventive therapy should still be decided after consulting an endocrinologist.
Physical activity is the next factor to prevent the development of osteoporosis. Prevention using physical activity can increase the load on the bone and stimulate its strengthening.
For women during menopause, an important factor in the prevention of osteoporosis is the use of hormone replacement therapy, which allows them to “imitate” normal ovarian function for a long time and reduce the risks associated with the extinction of the natural hormonal function of the ovaries. Such therapy is also an effective factor in the treatment of osteoporosis, if it has already occurred. Of course, the selection of treatment is carried out by an endocrinologist.
One should not forget about the need to monitor thyroid function if the development of osteoporosis is suspected. To do this, it is enough to perform an ultrasound of the thyroid gland and pass a basic set of tests (usually for the first examination it is enough to donate blood for TSH, T4 free, and antibodies to thyroid peroxidase). When taking tests, do not forget about the need to monitor the level of ionized calcium annually! Timely detection of an increase or decrease in blood calcium levels greatly facilitates treatment.
Why does brittle bone disease target women more often?
It has long been no secret to experts that women suffer from osteoporosis several times more often than men. Their bone density begins to decline after the age of 40. With the onset of the postmenopausal period, these processes only intensify. Specialists from the Center for Expertise and Quality Control of Medical Care of the Ministry of Health of the Russian Federation published the results of a study according to which more than 75% of patients with hip fractures are women. A third of these patients are over 85 years of age.
The special “love” of osteoporosis for women is explained simply. With the onset of menopause and the shutdown of ovarian function, the level of sex hormones in their body decreases quite sharply. But they are the ones who orchestrate the processes of bone tissue renewal.
Particularly critical is the drop in testosterone concentration. Androgen, although called the male sex hormone, is also present in the female body and performs extremely important functions. Thus, it stimulates the division of mesenchymal cells of the bone marrow and their transformation into osteoblasts - bone cells that produce intercellular bone substance and incorporate calcium. Actually, this substance, and even the “matured” osteoblasts themselves, which have become osteocytes, are bone.
It turns out that testosterone triggers a chain of transformations, the result of which is the appearance of new sections of bone to replace the old ones that need to be dismantled. It is clear that hormone deficiency will cause inhibition of this process. The bone will continue to deteriorate, because this is one of the natural aspects of its renewal, but at the same time, creative work in it will stop.
In order for the two scales called Destruction and Creation to be leveled, it is necessary to restore the balance of sex hormones. A natural question arises: how to do this? We'll talk about this too, but a little later. Before learning about the most effective folk remedies for treating osteoporosis, it is worth finding out how the disease generally manifests itself in the initial stages.