Why do my knees hurt after cycling?
The bicycle is considered quite safe for the knee joints, and even useful with moderate load. It is recommended for arthrosis of the knee joints - small and medium loads reliably reduce pain and improve joint function. Here, unlike running, there is no axial and shock load.
But it all depends on the number of cycling sessions and their intensity. The occurrence of pain can be affected by a sudden increase in load or changes in bicycle settings and settings.
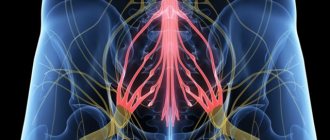
The most common complaint among cyclists is pain in the front of the knee joint. This is the so-called patellofemoral pain syndrome, associated with overload and improper functioning of the extensor apparatus of the knee joint. It is more common in runners, but often occurs in cyclists during intense and prolonged exercise.
Read on: Runner's knee: how to diagnose, treat and prevent injury
There are two more overload syndromes in cyclists:
- iliotibial tract friction syndrome – pain along the outer surface of the knee joint;
- pes anserine tendonitis – pain along the inner surface.
Knee pain after cycling most often begins due to incorrect placement of the saddle and pedals, as well as pedaling technique - it is these errors that appear as the volume and intensity of training increases.
One of the most common mistakes is setting the saddle too low or moving the saddle too far forward. It is believed that the most optimal setting is when, with the pedal position at 6 o'clock (that is, in the lowest position), the angle of flexion in the knee joint is 25 degrees.
Placing your feet too wide can lead to pain in the knee joint during intense exercise.
Training plans for marathon and half marathon. and start preparing today.
All this affects the functioning of the leg muscles and causes pain. When the saddle is lowered, the entire biomechanics of the knee joint changes. The inner head of the quadriceps, which is needed for full extension of the knee joint, stops working, and the outer head of the quadriceps is overloaded.
This leads to displacement of the patella from the outside during movement, overload of the extensor apparatus, and the development of pain in the anterior sections - that is, behind the kneecap.
Arthrosis
This disease is considered a disease of older people. Cartilage wears off over time due to wear and tear of the body. Symptoms of the disease include:
- aching pain that increases after physical activity;
- the appearance of pain outside of a state of rest;
- crunching in joints;
- change in the shape of the kneecap;
- dysfunction of the joint.
The pain of arthrosis can be eliminated through a course of treatment, but this disease cannot be cured. This is due to the fact that no means have yet been created that regenerate articular cartilage.
What happens if knee pain is left untreated?
If knee problems caused by cycling are left untreated, constant pain will soon discourage you from exercising.
With prolonged pain syndrome, premature wear of the cartilage of the patella and femoral condyles may begin, which will lead to arthrosis of the knee joint and progression of pain.
It is important to understand that in the vast majority of cases the solution is quite simple, and the effect of treatment is achieved quite quickly - if you do not delay treatment.
Lack of water
If your knees hurt after cycling, the reason may be a lack of fluid. The smooth movement of the legs is carried out thanks to the lubricant present in the joints. To produce it in the required volume and protect the knees, fluid is required. Therefore, it is advisable to take drinking water with you. It is better to consume it every 20 minutes, and not when a noticeable feeling of thirst appears. You should drink in small sips.
Isotonic drinks are suitable for consumption; they quickly normalize the water-salt balance. The brands used are Allsport and Gatorade. In addition to water, they contain carbohydrates and electrolytes - potassium, sodium. You should not choose carbonated drinks, even if it is mineral water.
What to do if your knees hurt from cycling
1. Ideally, you should immediately reduce your load and consult a doctor - a specialist in sports medicine.
It’s useful to start by figuring out for yourself what might be wrong: assessing the position of the saddle, pedals and feet - the doctor will still need this information later. We need to remember whether there have been injuries to the knee joint in the past, and take into account age. The cause may be a degenerative tear of the meniscus, progression of arthrosis, and so on - and only a doctor can determine this.
2. Sometimes, for certain symptoms, it is recommended to do an MRI to rule out structural damage from high-intensity stress. MRI subsequently needs to be interpreted correctly to distinguish changes that are present in all individuals from changes that are of clinical significance.
3. Orthopedic testing is also of great importance. Thanks to him, sometimes even before an MRI it is possible to correctly establish the diagnosis and cause of pain.
4. During intensive cycling, it is recommended to perform special exercises that can reduce the negative effect of monotonous long-term and intense exercise. Such exercises include:
- Training the inner head of the quadriceps: squats with wide legs with a fitness band above the knees, tightening the hips.
- Stretching the iliotibial tract, which runs along the outer side of the thigh: it can be rolled out on a massage roller and stretched while standing.
- Training the hip abductors: leg raises with an elastic band around the hips, planks with leg raises, exercises on simulators for the abductors.
For pain in the knee, such exercises help relieve pain and restore correct pedaling biomechanics.
It is not necessary to give up cycling completely, but you need to significantly reduce the volume and intensity of exercise. Pain syndrome is a reason to think about the individual selection and installation of a saddle, pedals and cleats - all this is of great importance for preventing problems in the future.
Read on topic: How to choose clipless pedals for a bicycle
It is worth considering that doctors are moving away from hardware physiological therapy - and for syndromes such as knee problems, it is not clinically effective. Therefore, if a doctor prescribes a magnet, laser or ultrasound, he is guided by an outdated technique, and one cannot count on a positive effect from the treatment.
Arthritis
This is an inflammatory lesion of the joints. Arthritis can be detected in both adults and children or adolescents. The catalyst for the disease is considered to be hypothermia, injuries, diseases - tuberculosis and tick-borne borreliosis.
Arthritis manifests itself as:
- heat at the knee;
- swelling;
- redness of the skin over the joints;
- prolonged pain;
- difficulty bending the leg;
- asymmetry of the lesion.
If arthritis is detected, it is necessary to temporarily exclude cycling and other physical activities that can injure the joint.
How to eliminate short-term pain
If the joint hurts after long trips, but after some time the pain subsides, first of all you need to:
- adjust the bike height;
- install the saddle parallel to the road;
- choose the correct speed mode for the bike to reduce the load on your knees;
- observe the drinking regime. In summer, the intervals between drinking water should not exceed 20 minutes;
- Before starting the ride, do a warm-up;
- wear clothes that are appropriate for the season.
Most often, these activities turn out to be effective and help eliminate pain in those who perform them.
Medicines
If your knees hurt, your doctor may prescribe treatment with medications. Typically used in these cases:
- chondroprotectors – “Dona”, “Teraflex”, “Structum”;
- non-steroidal anti-inflammatory drugs – “Xefocam”, “Ortofen”;
- special microelements and vitamin complexes.
Ointments, creams, and gels are also used to heat the application areas. Popular products are “Finalgon”, “Nikoflex”, “Apizartron”.
Contraindications:
- The presence of allergic rashes, purulent wounds, fibrous lesions in the operation area,
- Fresh injury to the periarticular area.
- It is prohibited to perform arthroscopy on people who have malignant neoplasms in the body. In this case, it is recommended to first undergo full treatment (radiation therapy and chemotherapy), and then allow the body to recover.
In some cases, even if there are any local problems or allergic reactions, it is possible, together with the doctor, to select a method of arthroscopy that will have minimal consequences for the patient.
Other reasons
The cause of pain may be a very short warm-up or lack thereof. Beginners usually neglect it, believing that it is not required. But due to lack of warm-up, injury may occur: the muscles need to be warmed up, especially during morning workouts.
The problem may also be related to flat feet. Due to improperly distributed load, there is a strong impact on the knees, so for such an illness you need to buy special shoes. But before this, it is worth visiting an orthopedic doctor who will recommend the level of physical activity - long trips may be prohibited.
The cause of the pain may be a previous injury. Moreover, it can be both fresh and old, for example, it happened several months ago. Stress on the knee can be a catalyst for inflammation of an old injury.
Prices
Treatment of Hallus Valgus (“bones” on the leg). One leg - 70,000 rub. Two legs - 120,000 rub.
Arthroscopy of the knee joint—from 35,000 to 150,000 (excluding anesthesia, hospitalization and consumables) depending on the volume of the operation. Consultation with a GarantKlinik specialist is required.
Arthroscopy of the shoulder joint - from 30,000 to 65,000 rubles (excluding anesthesia, hospitalization and consumables) depending on the volume of the operation. Consultation with a GarantKlinik specialist is required.
GarantKlinik is the base of the Sechenov Moscow State Medical University, so our prices are similar to the state ones.
Recovery
Complete rehabilitation occurs 4-5 weeks after surgery.
Since in the case of arthroscopy, tissue damage is minimal, the rehabilitation period is short.
As a rule, after the intervention, a person is allowed to get out of bed on the second day. Movement during the period of hospitalization is not prohibited. Already on the 2nd day, the patient can be discharged and continue recovery at home. The doctor gives each patient a list of necessary procedures that speed up healing and develop the joint.
On days 7-12, the doctor examines the healing site and removes the sutures. After 2-3 weeks a person can already put on his usual shoes
When carrying out rehabilitation, the following methods are used to accelerate healing and restore the functionality of joints:
- Physiotherapy. Exercises aimed at developing the operated joint. A set of exercises is selected individually by an orthopedic surgeon.
- Careful hygiene, especially if the operation is performed on the joint of the lower extremities. The rate of healing of postoperative sutures directly depends on maintaining cleanliness.
- Wearing special orthopedic shoes with soft insoles. In some cases (if the operation was performed to eliminate valgus bursitis), structures are used to separate the toes or additional devices that hold the operated area in its natural position.
- Physiotherapeutic procedures: massage, magnetic therapy, laser therapy. Physiotherapy is prescribed by a physiotherapist and only after a personal examination of the patient.
Arthroscopy does not require long-term wearing of correction devices. Most rehabilitation techniques can be used at home by the patient after consultation with the attending physician.