Joint pain that is harmless at first can cause disability without proper treatment. This happens not only with arthrosis, when articular cartilage gradually degrades. Ankylosing spondylitis, or ankylosing spondylitis, or ankylosing spondylitis, also leads to sad consequences - this diagnosis can be heard at an appointment with a rheumatologist. The symptoms of the disease are very similar to osteoarthritis, but the principles of treatment differ. What do doctors advise in such cases?
In men, ankylosing spondylitis is diagnosed 2-3 times more often than in women
What is ankylosing spondylitis
This term refers to chronic progressive joint disease. In 80% of cases it begins with back pain (intervertebral joints are damaged), much less often with peripheral arthritis in the joints. The inflammation begins where tendons and ligaments attach to bone and spreads to the small joints between the vertebrae. Gradually the bones fuse and the spine slowly turns into one solid bone.
Since even the ligaments ossify, the person completely loses flexibility and cannot move. The inflammatory process spreads to the peripheral joints, which may already be affected by arthrosis, as well as to the eyes, lungs, kidneys and heart. Without timely treatment, the prospects are very sad.
Where to go?
The fact that the patient is entitled to a disability group and certain measures of state support (including preferential medications, free treatment in a sanatorium) must be reported by the local doctor, usually a therapist. The patient is given a referral to undergo a medical commission, as well as an application form filled out in the name of the chief physician of the medical institution to which the patient is attached under the compulsory medical insurance policy. After this, the person needs to undergo a set of examinations and tests and receive a therapist’s conclusion, as well as collect a set of necessary documents with which to appear at the meeting of the ITU commission on the appointed day (the date is agreed upon in advance).
Getting a disability
Why does ankylosing spondylitis develop?
No one knows the exact cause, but it is assumed that the disease develops due to malfunctions of the immune system, especially in the presence of provoking factors:
- too low birth weight;
- infectious disease at the age of 5-12 years (infections of the genitourinary system and intestines are of particular danger);
- hypothermia;
- spinal and pelvic injuries;
- the presence in the body of enterobacteria that cause arthritis, etc.
The HLA-B27 gene is present in almost everyone who has been diagnosed with ankylosing spondylitis
Is it possible to be denied disability?
After studying all the materials, the commission may come to the conclusion that the applicant does not need to be assigned a special status and associated benefits.
The main reasons for refusal are:
- Absence of serious disturbances in the functioning of the body;
- High degree of financial well-being.
What to do if you refuse
A negative decision of the commission can be appealed in two ways:
- Request a re-examination;
- Go to court.
To repeat the examination, you need to write a statement expressing your disagreement with the decision received and demanding its revision. If the re-examination does not bring the desired result, the only option left is to go to court, which is the last resort. The resulting court decision is not subject to appeal.
Application form for appeal
Sample statement of claim
Forms of ankylosing spondylitis
Depending on the location, the disease has the following forms:
- central – only the spine is affected (accounts for about half of all cases);
- rhizomelic - the shoulders and hip joints are also affected;
- peripheral – affects, in addition to the spine, the knee, elbow and ankle joints (diagnosed mainly at the age of 10-16 years);
- Scandinavian - similar in symptoms to rheumatoid arthritis, affects all joints, including small ones;
- visceral - inflammation also extends to blood vessels, kidneys, eyes and other organs.
The earlier ankylosing spondylitis is detected, the better it is treated
With no exceptions
There are situations in which disability is mandatory. As a rule, these include either pronounced manifestations of pathology or the presence of complications.
- Damage to the heart and aortic bulb by the pathological process.
- Bone destruction due to enthesitis.
- Development of Ig-A nephropathy or amyloidosis against the background of ankylosing spondylitis.
- Ischemic optic neuropathy.
- Restriction (more than 60%) or complete absence of movement in the hip joints due to arthritis.
- Significant reduction or absence of function of the temporomandibular joints.
- Spinal cord compression as a result of subluxation of the atlantoaxial joint.
- The occurrence of arachnoid diverticula of the spinal cord.
- The presence of a disease for 10 years that is resistant or difficult to correct with drug therapy.
The disability group assigned depends on the number of manifestations and the severity of their course.
Features of symptoms
The most common symptom is back pain, which worsens during sleep and improves with exercise. In addition, a person may feel:
- moderate pain in the groin, sacrum;
- stiffness of movements;
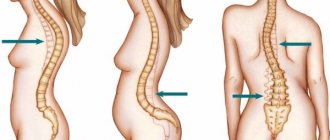
- curvature of the spine and stoop;
- feeling of chest tightness;
- dizziness and tinnitus;
- swelling of the joints.
With ankylosing spondylitis, the temperature may also rise at the end of the day, weight may decrease, and the person will quickly get tired. The eyes may become inflamed, sometimes heart valve failure develops and difficulty breathing occurs. Complications in the functioning of the nervous system are not uncommon. Similar symptoms occur with arthrosis, osteochondrosis, spondylosis, rheumatoid arthritis, so it is very important to make a correct diagnosis.
Ankylosing spondylitis has symptoms similar to arthrosis
Procedure for issuing a certificate
A certificate for a disabled person is issued by a specialized government agency - the medical and social examination (MSE). Before contacting the organization:
- treatment in a regular clinic at the place of registration;
- carrying out activities to prepare documentation.
Attention: ITU goes to the patient’s place of residence if the latter is unable to visit the government agency. The procedure for applying for help is as follows:
The procedure for applying for help is as follows:
The work of medical and social examination
The responsibilities of the government agency include confirming the final diagnosis and issuing the coveted certificate about the group. The decision is made only after studying all the nuances of the situation. For the applicant this means the following:
- His documents will be subject to scrutiny. Each certificate will be examined for accuracy.
- Civil servants will analyze the correctness of:
- making a diagnosis;
- treatment assignments;
- use of medications.
- The patient will be invited for an interview. During its course:
- a visual inspection is carried out;
- the person’s social status, including family status, is clarified.
- The examination will probably require an inspection report of living conditions. Finding sites with a license to play online slots is not so easy. There is a casino table with withdrawal of money to a card and this is a really accessible option for comparing information and parameters that will allow you to draw appropriate conclusions. Playing in a casino with withdrawal is quite simple. It is done by social workers.
Upon completion of all required activities, the commission makes a decision. It could be:
- positive - the establishment of a specific group;
- negative if there are no sufficient grounds.
The applicant is given a certificate. The paper states:
- disability category;
- degree of disability;
- date of re-examination.
Important: you cannot skip the next examination, as the disability is canceled automatically. And this leads to a stop in the provision of appropriate benefits and payments.
How is ankylosing spondylitis diagnosed?
As with arthrosis of the knee, shoulder or hip, this disease involves changes in the articular cartilage. The pathology takes many years to develop, and the first symptoms appear when the joints have already significantly degraded. To clarify the diagnosis, a rheumatologist may prescribe the following examinations:
- X-ray;
- MRI;
- test for histocompatibility antigen, which is responsible for predisposition to this disease;
- Ultrasound of hands and feet;
- laboratory tests - ESR, C-reactive protein (the most informative in determining the current stage of the inflammatory process);
- examinations of other systems (fluorography, electrocardiography, consultation with an ophthalmologist, etc.).
Diagnosing ankylosing spondylitis is very difficult
Examinations for disability
Did you know that...
Next fact
The presence of disability and its degree are determined by a medical and social examination (MSE).
The attending physician refers the patient to MSE if the disease has reached certain indicators:
- rapid development of the disease and lack of remission within 1 year;
- slow development of the disease with prolonged and serious exacerbations, spread of the process to other organs;
- severe disorders of the spine and joints, immobility, difficulty breathing.
Check out the list of required tests to pass the ITU commission. The ITU commission considers the following tests and examinations:
- General blood analysis.
- Blood for ESR, protein, protein fractions.
- X-ray of the spine.
- or MRI of the spine.
- Outpatient card with a description of the patient's complaints and course of illness.
- Extracts from hospitals.
- Extracts from sanatoriums (if available).
How is ankylosing spondylitis treated?
As in the treatment of osteoarthritis, a rheumatologist selects an individual treatment regimen - combines medicinal and non-medicinal methods. The goal of treatment is to eliminate pain and inflammation and slow down the progression of the disease. For this purpose, they resort to medications, physical therapy, recommend special exercises, and in severe cases, surgical intervention (joint replacement, fixation of vertebrae or straightening of a deformed spine).
The best physiotherapy for this diagnosis is UV irradiation, UHF therapy of joints, electrophoresis of novocaine or Parfenov's liquid. You can also get a certain improvement after a course of ultraphonophoresis with hydrocortisone, after taking salt and hydrogen sulfide baths. In the inactive stage of the disease, balneotherapy is indicated.
In case of ankylosing spondylitis, the patient is given an individual exercise therapy program. It includes exercises for stretching the spine, bending, Nordic walking and swimming, yoga or complexes with a gymnastic stick. The main thing is not to experience discomfort, otherwise you can harm the affected joints.
In case of ankylosing spondylitis, you can perform the following complex of exercise therapy, which over time will alleviate the general condition:
Factors leading to disability
A diagnosis is not a reason for disability. People with significant mobility impairments caused by ankylosing spondylitis can apply for the group. Factors that make it possible to register a disability include:
- Stiffness of the spinal column,
- Loss of ability to do physical work,
- Loss of self-care ability
- Severe limb dysfunction
- Concomitant damage to internal organs,
- Progression of pathological changes during treatment.
What medications can be prescribed
Depending on the manifestations, the rheumatologist may include the following drugs in the treatment regimen:
- nonsteroidal anti-inflammatory drugs, such as indomethacin and diclofenac, for pain relief;
- hormonal;
- immunosuppressants (if the cause is immune in nature);
- inhibitors of TNF-alpha and B-cell activation;
- chondroprotectors (in the early stages they stop the degradation of joints, accelerate the restoration of cartilage and reduce pain).
As with other joint diseases, ankylosing spondylitis can have different development scenarios. If it is detected too late and left untreated, it can result in disability. In the early stages, a person has every chance to take control of the disease and continue to lead a full life.
Simple assessment
Laboratory and instrumental research methods do not always make it possible to assess the real severity of the disease. An extremely important factor in obtaining a disability group from a medical and social expert commission is a person’s ability to cope with everyday tasks and take care of himself.
One of the methods for assessing a patient's ability to self-care is a special BASFI scale. The person is given a form on which only 10 questions are written. Next to the questions is a scale with 10 marks. The extreme values correspond to the concepts of “easy” and “impossible”. The self-care ability score is based on the ability to perform some simple activities over the past week.
- Put on socks or tights without assistance or without using any devices that facilitate this action.
- Bend over a small object (pen, pencil), bending at the waist, provided that there are no auxiliary objects to perform this action.
- Reach the top shelf with your hand without outside help or using auxiliary objects.
- Stand up from a chair without using your hands for support, armrests, devices, or assistance.
- Get up from the floor from a lying position without assistance or use of devices.
- Stand in an upright position for 10 minutes without feeling discomfort, without resorting to the help of people or objects.
- Climb up the stairs (12-15 steps) without leaning on the railing, using a cane. In this case, you need to put one foot on each step.
- Look left or right by turning your head while keeping your torso stationary.
- Physically active activity - exercises, gymnastics, gardening, sports.
- The ability to be active throughout the day (at home or at work) without the need for rest.
This scale helps determine which group should be assigned to the patient.
The minimum score on the scale is 10 points, the maximum is 100. For answers whose score does not exceed 40 points, the assignment of disability is doubtful. A score of more than 40 points allows the patient to count on being assigned to a certain group (based not only on the score on the scale, but also on concomitant pathology).
Important information
- Intervertebral hernia provides grounds for receiving benefits. However, the patient is referred for examination only after long-term treatment. And then only if it does not show positive dynamics.
- Diabetes mellitus is directly included in the list of the Ministry of Health and Social Development. If there is such a metabolic disorder, you should confidently seek a referral. The category of disability will be determined during the examination.
- The consequences of a stroke also lead to the patient being recognized as disabled. According to statistics, only one person out of five recovers. Everyone else becomes beneficiaries.
- Vision problems are a special case. When examined by a doctor, I find out the possibility of recovery. And it depends on the reasons for the loss of vision. Therefore, such a disease is dealt with individually. If cure, including through surgery, is impossible, then a group is given.
We describe typical ways to resolve legal issues, but each case is unique and requires individual legal assistance.
How to get a disability group
According to the law, the attending physician must tell the patient that the patient is classified as a disabled person. However, quite often patients themselves ask leading questions to their doctor and only then do they have the opportunity to make their work easier and receive financial benefits from the state. Determines the ITU disability group (medical and social examination). Several doctors are present at this examination - a vertebrologist, a therapist, a neurologist, a traumatologist, etc. During the commission, the patient is interviewed and examined, blood tests, X-rays, CT, MRI, and extracts from the medical history card are carefully studied. Only on the basis of these data the patient receives a disability group.
You should also take into account the fact that doctors and ITU experts examine not only aspects of the patient’s disease, but also his financial security. If the patient claims that his relatives help him or he has large bank deposits, then most likely he will be denied disability, citing that he will not use his benefits, providing himself with better medicines and other methods of treating his disease.
The ITU may also focus on the patient's ability to do their job. If the patient does not disclose the fact that he does not work full-time, often asks for help from employees and superiors, but simply tries to psychologically support himself and tells the doctors that he is completely coping, there is also a risk that the disability group will be denied or his group will be denied not true. Such nuances of questions should be taken into account and be extremely careful during the examination.
The patient's disability may be temporary or permanent. These criteria are also decided at the ITU. Almost always and in all cases, every 5 years the patient is sent for re-examination of the disease and for inpatient treatment, to extend the group or remove it, or to change it.
Criteria for permanent, indefinite disability:
- If the female patient is 55 years old and the male patient is 60 years old;
- If the patient has disability group I or II for 5 years or more, if annual hospitalizations and rehabilitation were carried out in sanatoriums, dispensaries and specialized departments of hospitals, treatment in which was unsuccessful;
- If you have disability group III for 7 years or more with regular hospitalizations and rehabilitations that did not produce a therapeutic effect.
Medical and social examination
ANKYLOSING SPONDYLOARTHRITISAnkylosing spondylitis (Bechterew's disease) is a chronic systemic inflammation of the joints, sacroiliac joints and spine, its ligaments with a progressive tendency to ankylosis. The disease belongs to rheumatic diseases, since it is based primarily on connective tissue damage. The prevalence of ankylosing spondylitis in various countries ranges from 0.4 to 2%. Men get sick more often than women - ratio (5-9): 1.
It has been noted that ankylosing spondylitis occurs 2-6 times more often in family members in cases where the parents suffered from this disease. In most people, the disease develops at the age of 15-30 years, in 8.5% of people aged 10-15 years. After 50 years, the disease occurs extremely rarely. After 20 years of illness, 27% of patients become disabled, 73% of patients experience limited mobility, which forces them to change professions or reduce hours of daily work [Nasonova V.A., Ostapenko M.G., 1989]. The average age of disabled people suffering from ankylosing spondylitis is 44-47 years. The onset of the disease is associated with chronic inflammation of the synovium, similar to synovitis in RA. The disease begins with pain in the sacrum and spine in 75% of cases; in 20% - with pain in peripheral joints, and in 5% - with eye damage (iritis, iridocyclitis). Against the background of hereditary predisposition, genetic determination (the HLA B27 antigen complex is detected in 80-95% of patients), a certain role in the development of ankylosing spondylitis is assigned to infection that stimulates autoaggression, trauma, nervous and physical stress, dysfunction of the endocrine glands, and hypothermia. Subsequently, cartilage is destroyed and the process of ankylosis of the affected joints occurs. Damage to the intervertebral discs and vertebral bodies occurs as spondylodiscitis, accompanied by the formation of bone bridges along the edges of the vertebral bodies, giving the spine the appearance of a “bamboo stick”. The tendency to ankylosis is much more pronounced than in other forms of arthritis. Unlike RA, in patients with ankylosing spondylitis, rheumatoid factor is never detected in the blood, however, in the active stage of arthritis, patients experience an increase in ESR, a positive test for C-reactive protein and hyper-a2- and γ-globulinemia, increased enzyme activity— acid phosphatase and acid proteinase. Limitation of spinal mobility develops in two main ways: ascending - the process begins with damage to the sacroiliac joint and gradually spreads to the spine and ribs; descending - the process begins from the upper thoracic spine; it is rare. The cervical spine is involved in the process in half of patients 10 years after the onset of the disease. Complete ankylosis of the spine usually occurs no earlier than after 15-20 years.
Criteria for assessing work ability. There are four clinical forms of ankylosing spondylitis. The central form (damage to only the spine) occurs in 46.69 patients, rhizomelic (damage to the spine and “root” joints of the limbs - hip, shoulder) occurs in 17-18% of patients; peripheral (damage to the spine and peripheral joints - knees, elbows, ankles, wrists) occurs in 20-75% of patients; Scandinavian (damage to the spine and small joints of the hands and feet) is a type of peripheral form that is very similar to rheumatoid arthritis [Chepoy V.M., 1976].
The limitation of the patient’s life activity in a certain way depends on the clinical form of ankylosing spondylitis. In the central form of the disease, severe functional impairment is rarely observed, despite the development of severe kyphosis. With the rhizomelic form, mobility is significantly impaired and the patient quickly becomes immobilized. In the peripheral and Scandinavian forms, early manifestations of dysfunction of the hand and wrist joints end in loss of self-service elements.
According to the nature of the clinical course, two main types of ankylosing spondylitis are distinguished: primary chronic - characterized by a slowly progressive torpid course (complete ankylosation of the spine does not occur for 10-15 years) and recurrent, occurring with exacerbations, the frequency and severity of which are identical to the progressive form of RA. This is the most unfavorable type of ankylosing spondylitis. Frequent and prolonged exacerbations of the pathological process deprive patients of the opportunity to perform work in a production environment. Functional disorders in the spine and joints depend on the extent of the pathological process and the severity of the pain syndrome.
The course of the articular process can be acute (duration up to 3 months), subacute (6 months), protracted (9 months), chronic (more than 9 months).
Based on the degree of functional disorders of the spine and joints and the prevalence of the pathological process, for expert purposes three stages of ankylosing spondylitis are distinguished.
In stage I (early period of the disease), patients note inflammatory pain in the joints, lumbar region and sacroiliac joints, a feeling of stiffness in the lower back, especially in the morning, which is accompanied by rigidity of the lumbar muscles. Respiratory excursions of the chest are reduced to 3-4 cm (the norm is 6-8 cm). Stibora test - when bending, the arch of the spine is reduced by 2-4 cm and increases, it is 6-8 cm (the norm is 10 cm). Pavelky test - when turning the body, the length from the jugular notch of the sternum to the spinous process of L5 decreases by 2-3 cm and its increase is 5-6 cm (normal - 8 cm). On radiographs: signs of bilateral sacroiliitis (subchondral osteoporosis, unclear contours of the articulations with false widening of the joint space, focal periarticular osteosclerosis of the sacrum and iliac bones), partial ankylosis of the sacroiliac joints. Increased absorption of radionuclide (99Tc pyrophosphate) in the area of the sacroiliac joints compared to the sacrum during scintigraphy before the development of radiological changes. Indicators of the activity of the process depend on the clinical form, type of disease, and the presence of HLA B27 antigen.
In stage II (the advanced period of the disease), immobility of the lumbar region, limitation of movements in the thoracic and cervical regions, radicular pain, pain in large joints, poor posture (round back - “native posture” or “straight plank back”), tension in the back muscles or their atrophy. The type of breathing is abdominal, with a transverse fold on the abdomen. The respiratory excursion of the chest is reduced to 2-3 cm. With the Slibora test, the arc of the spine decreases when bending by 5-6 cm and the increase is 4-5 cm. With rotational movements of the spine, the length between the measured points decreases by 4-5 cm compared to the norm and its increase is 3-4 cm. X-rays of the spine reveal characteristic changes: complete obliteration of the sacroiliac joints, partial or complete ankylosis in the true joints of the spine, in the costovertebral and sternocostal joints, arthritis of the hip and knee joints.
Stage III (terminal) is characterized by a forced body position, a rounded back, atrophy of the muscles of the shoulder pelvic girdle, and a sunken chest. There are no movements in all parts of the spine. Respiratory excursion of the chest up to 0.5 cm. Breathing becomes shallow and frequent. The vital capacity of the lungs decreases sharply. X-ray: the spine appears in the form of a “bamboo stick” with ossification of the entire ligamentous apparatus of the spine, periosteal phenomena in the area of the ischial tuberosities, heel bones, and often ankylosis of large joints. Along with changes in the spine in stages I and II of the disease, there is eye damage in the form of iritis or iridocyclitis in 10-30% of patients, damage to the cardiovascular system (pericarditis, aortitis) in 20-22% of cases, damage to the nervous system (secondary lumbar thoracic, cervical radiculitis). In stages II and III, kidney damage (urolithiasis, amyloidosis) is noted in 31% of patients and lung damage as a result of limited respiratory mobility of the chest, which contributes to the development of respiratory diseases and tuberculosis.
Treatment of ankylosing siondylitis is based on the same principles as RA, and should be systematically long-term and adequate to the activity and severity of the disease. In the late stage of the disease, when the hip joints are affected, endoprosthesis replacement is indicated (to improve self-care). Clinical examination of these patients allows for systematic anti-inflammatory therapy to prevent exacerbations, preserve spinal function and general performance. During periods of remission, radiography of the joints and spine is performed once a year.
The criteria and approximate terms of VUT are similar to those for RA (clinical and laboratory characteristics of exacerbations of the disease, confirmed by activity indicators of degrees II and III. The duration of VUT, depending on the severity of exacerbations and the effectiveness of therapy, ranges from 40 to 90 days. For frequent and prolonged exacerbations, treatment according to sick leave should not exceed 4 months with subsequent referral to medical examination.
Criteria for the restoration of temporarily lost ability to work: a stable decrease in activity to grades 0 and 1, absence or moderate pain, dysfunction of the affected joints no more than grade 2. For persons working in contraindicated types and working conditions, the necessary restrictions are determined in accordance with the conclusion of the CEC of medical institutions.
Contraindicated types and working conditions: - work associated with heavy and moderate physical labor; - labor associated with forced body position, frequent bending, and vibration of the body; — work in unfavorable meteorological conditions (in hot shops, with high humidity, gas pollution); — in peripheral and Scandinavian forms of the disease, work that requires precise and small movements with prolonged standing is contraindicated.
Indications for referral to ITU:
- recurrent, rapidly progressing type of disease (no remission for more than a year);
- a slowly progressive type of disease with frequent, moderate frequency and duration of exacerbations, damage to other organs and systems;
— primary chronic type of disease of stages I and II in the presence of contraindicated types and working conditions and the impossibility of rational employment;
— Stage III of the process;
- rhizomelic form with severe and pronounced dysfunction of the shoulder or hip joints.
The required scope of diagnostic examination methods when referring to MSE should be the same as for RA.
CRITERIA FOR DISABILITY FOR BECHTEROW'S DISEASE IN ADULTS IN 2020 Disability is not established if the patient has: - a minor impairment of body function; minor dysfunction of the spine and/or joints; absence or low degree of disease activity; FC I; absence of extraskeletal manifestations of the disease; absence of complications of the disease and/or therapy. Disability of the 3rd group is established if the patient has: - moderate dysfunction of the spine and/or joints, with a remaining moderate or high degree of disease activity; FC II; the presence of extraskeletal manifestations of the disease with moderate impairment of body functions; absence of complications of the disease and/or therapy. Group 2 disability is established if the patient has: - severe dysfunction of the spine and/or joints, with moderate or high disease activity remaining; FC III; the presence of extraskeletal manifestations of the disease; the presence of complications of the disease and/or therapy; leading to severe dysfunction of the body. Disability of the 1st group is established if the patient has: - significantly expressed dysfunctions of the body, significantly expressed dysfunctions of the spine/joints; FC IV; the presence of extraskeletal manifestations of the disease; the presence of complications of the disease and/or therapy leading to significant impairment of body functions. CRITERIA FOR DISABILITY IN CHILDREN'S BEKHTEREV'S DISEASE IN 2021 Disability is not established if the child has: - absence or minor dysfunction of the joints and/or spine; radiographic stage I, no disease progression; absence or presence of exacerbations (no more than 1 time per year), absence or I degree of activity of the inflammatory process during therapy; FC I; no complications of the disease from drug therapy (NSAIDs). The category “disabled child” is established if the patient has: - moderate dysfunction of the joints and/or spine (FC II degree);
radiographic stage II; progressive course of the disease: exacerbations 2 - 4 times a year, continued activity of the inflammatory process of I or II degree against the background of immunosuppressive therapy; the need to adjust therapy, the possibility of achieving remission only with the use of immunosuppressive therapy with drugs from several (2 or more) pharmacotherapeutic groups (except for NSAIDs), including genetically engineered biological drugs; the presence of complications of the disease and ongoing drug therapy. - severe disturbance of static-dynamic function due to damage to the joints and/or spine; radiographic stage II or III; progressive course of the disease; frequent long-term exacerbations (more than 4 times a year), FC II or III; continued activity of the inflammatory process of 2 or 3 degrees against the background of immunosuppressive therapy; the possibility of achieving remission only with the use of immunosuppressive therapy with drugs from several (2 or more) pharmacotherapeutic groups (with the exception of NSAIDs); including genetically engineered biological drugs; the presence of complications of the disease and ongoing drug therapy. — significantly pronounced disturbances of static-dynamic functions caused by damage to the joints and/or spine; radiographic stage III or IV; rapidly progressing course of the disease; activity of the inflammatory process of 3 degrees; FC III or IV; low efficiency or resistance to ongoing immunosuppressive therapy with drugs from several pharmacotherapeutic groups (2 or more, including genetically engineered biological drugs); the presence of irreversible complications of the disease and ongoing drug therapy. A patient can receive an official conclusion on the presence (or absence) of grounds for establishing disability only based on the results of his examination at the ITU bureau of the corresponding region
.
The procedure for completing documents for undergoing MSE (including the algorithm of actions in case of refusal of attending physicians to refer a patient to MSE) is described in sufficient detail in this section of the forum: Registration of disability in simple language
Source
Disabled status
In total, there are three groups of disabilities, which differ in the severity of damage to various elements of the musculoskeletal system (primarily the vertebrae, intervertebral discs and joints), the ability to continue professional activities and the ability to fully move without the help of special devices.
Indications for obtaining disabled status
| Disability group | Evaluation criterion | Indications for identification (to whom it is given) |
| Severe joint damage (irreversible) with progressive failure of internal organs and endocrine glands. | Damage to the joints and spine of the 4th degree. Labor and independent movement are impossible. |
| Rapid progression of the disease with persistent disorders of internal organs (characteristic of a complicated course of the disease and peripheral arthritis). | Spinal damage of 2-3 degrees, provoking intense pain in the area of the affected segment. Work in industrial and enterprise conditions is impossible in most cases (with the exception of light work at home). Some patients with disability group 2 cannot care for themselves without outside help and experience serious psychological difficulties associated with adaptation to the disease and the social environment. |
| Minor or moderately severe disorders of one of the categories of life activity. | Chronic course with infrequent relapses, quite successfully amenable to drug and hardware control. The patient may experience constant pain in the lower back and back of moderate intensity. Performance is limited, but possible. Changes in the joints are mild. |
Note! Patients who have the status of a disabled person and a disability group have the right to receive financial support measures from the state (disability insurance pension). Its size depends on the established group, the presence of dependents and the region in which the patient lives. For example, the size of the disability pension for disabled people of group 3 with two dependents is about 5,800 rubles (disabled people of group 1 with the same conditions will receive a little more than 13,200 rubles).
Treatment of pathology
Competent treatment of the disease requires an integrated approach, the basis of which is not only inpatient but also outpatient therapy. It will not be possible to completely get rid of spondyloarthritis, but you can significantly improve the patient’s quality of life.
Therapeutic actions will reduce inflammation and relieve the victim of severe pain. For this, a patient with ankylosing spondylitis is recommended to take NSAIDs (non-steroidal anti-inflammatory drugs).
If ankylosing spondylitis progresses rapidly, accompanied by dysfunction of the spinal joints and a number of complications, the following treatment is suggested:
- Taking immunosuppressants.
- Taking adrenal hormones.
- Physiotherapy.
- Stay in a sanatorium.
Therapeutic gymnastics consisting of light physical exercises is recommended. The latter should be selected exclusively by a specialist. He will teach the patient how to properly relax all muscle groups. The training itself should take at least half an hour twice a day.
Regular deep breathing will help reduce the rate of development of sternum immobility. In the initial stages of the disease, the patient is advised to take such measures as:
- Swimming.
- Skiing.
- Exercises to strengthen the spinal and gluteal muscles.
The patient is instructed to sleep on a hard bed, without any elevations in the cervical spine (pillow, bolsters, etc.). If the form of spondyloarthritis is advanced, movements in the spine will be significantly constrained. Surgical intervention is recommended for such a patient.