September 24, 2019
18020
0
4.5 out of 5
Ankylosing spondylitis or ankylosing spondylitis is a chronic inflammatory process that gradually affects an increasing number of joints. This is accompanied by severe pain and a significant limitation of mobility, which in severe forms of the disease can completely deprive a person of his ability to work. And given the fact that the disease usually manifests itself before the age of 30, this requires urgent action.
SL-Clinic specialists will help you diagnose ankylosing spondylitis in a timely manner, help you cope with it and stop its progression. With us you will find an attentive and sensitive attitude, a high level of medical services and the latest treatment methods that ensure maintaining a high quality of life even with a diagnosis of ankylosing spondylitis. The prices of services can be found by looking at the price list.
What is ankylosing spondylitis
Until now, medicine still does not know exactly the reasons for the development of the disease. A large role in this is played by genetic predisposition, namely the presence of the genetic marker HLA-B-27. Triggering factors may include:
- infectious diseases, especially those caused by streptococci;
- injuries of the spine, pelvis, intervertebral hernia;
- hypothermia;
- disturbances in the functioning of the endocrine system;
- diseases of the genitourinary system.
Ankylosing spondylitis affects joints in a specific sequence. The inflammatory process is initially localized in the area of the junction of the ilium and sacrum on one or both sides (sacroiliitis). It gradually spreads to the lumbar spine and continues to move towards the neck. As the disease progresses, the inflammatory process involves the hip joints, feet and even finger joints.
Over time, osteophytes, which are bone growths, form along the edges of the articular surfaces of the vertebrae. The intervertebral discs become thinner and subsequently the vertebrae fuse together, which leads to a complete lack of mobility in this segment of the spine. When most of the vertebrae are affected, the person loses the ability to bend and straighten.
Classification of forms
Based on research data, experts distinguish the following forms of the disease:
- central, localized on the spine;
- kyphosis, in which inflammation affects the vertebrae of the cervical and thoracic spine;
- rigid, leading to smoothing of the natural curves of the back;
- rhizomelic, the area of localization of which is the spine and root joints;
- peripheral, involving the joints of the lower extremities;
- Scandinavian, which is characterized by damage to the joints of the hands;
- visceral, which combines the symptoms of any of the listed forms with simultaneous inflammation of the kidneys, heart or arteries.
Possible complications
Ankylosing spondylitis is dangerous due to damage to internal organs, in particular:
- heart muscle (partial or complete blockade, valve defects, inflammation of the aorta);
- eye (inflammation of the iris and ciliary body - iritis and iridocyclitis);
- lungs (fibrosis);
- kidneys (amyloidosis, uremia, renal failure).
Men are more susceptible to the development of complications, especially those who neglect medical care and refuse to look for and influence the causes of their own condition.
Clinical picture
The course and manifestations of ankylosing spondylitis are unpredictable. In some cases, it progresses so quickly that after a few years it leads to disability, in others (more often in women) it may not provoke significant changes in the condition of the joints for ten years.
At the same time, diagnosing the pathology in the early stages is quite problematic, since it often develops unnoticed. And in the future, its manifestations can easily be mistaken for signs of osteochondrosis and other degenerative diseases of the spine.
The main symptoms of ankylosing spondylitis are:
- impaired mobility, which affects gait;
- fast fatiguability;
- discomfort of varying degrees of intensity in the lower back, and subsequently throughout the entire back, often occurs at night and in the morning, and then gradually disappears during the day;
- elimination of pain when changing body position;
- irradiation of pain to the buttocks and heels;
- discomfort in the ligaments and places of their attachment to the bones;
- thickening of fingers;
- gradual involvement of an increasing number of joints in the pathological process.
The spine is the first to suffer, and not all at once, but in separate areas. Mild discomfort intensifies and turns into severe pain in the affected area. Often the knee joints or hands are among the first to be affected. This is accompanied by pain, redness of the skin around them and swelling.
Depending on how the onset of the disease occurs, there are several types of its debut:
- by type of radiculitis;
- by type of mono- or oligoarthritis;
- by type of rheumatoid arthritis;
- febrile type;
- according to cardiological type, etc.
The progression of the disease provokes curvature of the spine, which causes intercostal neuralgia and impaired lung function. As a result, the patient may experience difficulty breathing. If the joints of the cervical spine begin to suffer, headaches, nausea, and attacks of dizziness often occur. In advanced cases, it is possible to form a hump (thoracic kyphosis) and change the position of the head: it drops lower and moves forward.
Ankylosing spondylitis is characterized by alternating periods of remission and exacerbation. The duration of each of them can be several years. But it is dangerous to consider a decrease in the intensity of manifestations until their complete disappearance as recovery. Ankylosing spondylitis does not stop developing, and under the mask of calm the first signs of destruction of other joints and the occurrence of complications may be hidden. It is especially dangerous to miss a lesion of the sacral joint.
Statistics and etiology of the disease
The first mentions of cases of ankylosing spondylitis are found in medical records of the European Middle Ages. Doctors of that time were quite surprised to discover skeletons with characteristic ossification of the spine, the individual elements of which formed a strong “bone” column. In the mid-19th century, the disease became the subject of general medical study, as evidenced by surviving records of patient complaints and examinations of deceased people. The works of the Russian doctor Vladimir Bekhterev, the German Adolf Strumpel and the Frenchman Pierre Marie are accepted as the basis of etiology and are currently being studied in medical institutions.
Current statistics on ankylosing spondylitis indicate a gender link. In men it occurs 4-6 times more often and has a more aggressive, accelerated course than in women. The latter note:
- low degree of pain syndrome;
- preservation of full spinal function for a long time;
- arthritis occurs with long-term remission;
- signs of sacroiliitis (inflammation of the sacroiliac joint) are recorded relatively rarely.
The area of development of the pathological process is the spine, large joints of the lower extremities and the sacroiliac joint. With extra-articular localization, the first signs of the disease are damage to the eyeballs in the form of redness of the sclera, inflammation of the iris or cornea. Characteristic signs are observed in 5-10% of patients, which in some cases makes it possible to make an accurate diagnosis at the initial stage of development of ankylosing spondylitis. Less common is an alternative onset of pathology in the form of inflammation of the walls of the aorta or muscle fibers of the heart muscle, developing against the background of an actively occurring pathological process in the joints of the spinal column.
Diagnostic methods
The effectiveness of therapy largely depends on when the correct diagnosis was made. To diagnose ankylosing spondylitis in the early stages of development, an x-ray examination is sufficient, but the difficulty lies in differentiating it from other neurological and rheumatological diseases.
Only an experienced rheumatologist who is well acquainted with the clinical picture of the disease will be able to quickly recognize ankylosing spondylitis and select the optimal treatment regimen. At SL-Clinic you will find specialists who are familiar with the manifestations of pathology first-hand and are able to diagnose the disease in the early stages based on a score of existing symptoms and data from laboratory and instrumental examinations.
During the examination of the patient, the rheumatologist performs a series of functional tests to detect sacroiliitis and determine the limitation of mobility. Also assigned:
- rheumatic tests;
- UAC;
- blood chemistry;
- genetic testing to detect HLA-B-27;
- X-ray of the pelvis, as well as the spine in direct and lateral projections;
- CT;
- MRI.
The price of each diagnostic procedure can be found in diagnostic laboratories. And our specialists will help you decipher the research results as soon as possible.
Treatment of ankylosing spondylitis
Unfortunately, it is impossible to be completely cured. But stopping the progression of the pathology, preventing the development of complications and immobilization of the patient is a real task. Therapy is long-term, systematic and consists of separate stages. The prognosis depends on when it is started and the correct selection of therapeutic measures.
Treatment is complex and includes:
- drug therapy;
- kinesitherapy;
- physiotherapy;
- massage.
Drug treatment
Drug treatment is necessary to eliminate pain and inflammation in all affected joints. For these purposes, patients are prescribed a complex of medications, which together have a comprehensive effect on the body. This:
- NSAIDs are the mainstay of therapy. They have anti-inflammatory and analgesic effects. When taking drugs from the NSAID group, a significant improvement in the patient’s condition is observed within two days.
- Corticosteroids are drugs with powerful anti-inflammatory properties, prescribed when NSAIDs are ineffective in patients with severe manifestations of ankylosing spondylitis. In difficult cases, intra-articular injections are indicated.
- Muscle relaxants – eliminate increased muscle tone, which is often observed when the spine is affected by ankylosing spondylitis. This leads to improved mobility and reduced pain.
- Drugs that increase blood circulation are necessary to improve the nutrition of affected tissues and normalize metabolic processes.
- Immunosuppressants - used in severe forms of the disease to suppress the immune system and, accordingly, autoimmune disorders. Some drugs, for example, the well-proven Remicade, are administered exclusively under the supervision of a doctor, and you should remain under observation for at least 2 hours after this.
- Chondroprotectors – promote the regeneration of cartilage tissue in affected joints.
When the disease is highly active, pulse therapy is used. It involves drip administration of 1 g of a drug from the group of corticosteroids, usually prednisolone, for 3 days.
Kinesitherapy
Kinesitherapy or movement therapy is one of the main aspects of the treatment of ankylosing spondylitis. Patients are advised to walk a lot, visit the pool and regularly engage in exercise therapy. A set of physical therapy exercises is selected for each patient individually by the doctor. Only a specialist will be able to correctly calculate the required load, which will benefit the patient.
Exercise therapy is based on stretching exercises: hanging, twisting, bending, etc. The whole complex should be performed at least twice a day, every day. The total duration of the lesson is on average 20–30 minutes.
Without regular exercise therapy, all attempts to stop the progression of ankylosing spondylitis will be ineffective. In addition, exercise therapy helps normalize the position of the spine and improve posture.
Physiotherapy and massage
To increase the effectiveness of drug therapy, patients are prescribed a course of physiotherapeutic procedures:
- magnetic therapy;
- ultrasound therapy;
- Bernard currents;
- paraffin therapy;
- reflexology;
- salt, bischofite or hydrogen sulfide baths.
During the period of remission of ankylosing spondylitis, massage sessions are indicated. To avoid exacerbation of the inflammatory process, they must be carried out with a correctly selected intensity of exposure. Therefore, massage should only be done by a qualified chiropractor who is well acquainted with the peculiarities of the course of ankylosing spondylitis.
New drugs for therapy
Today, in the practice of modern rheumatology, immunosuppressive drugs are increasingly prescribed for AS. There is a wide range of drugs that suppress the immune system. These drugs are used in the treatment of inflammatory conditions, autoimmune diseases, and after organ transplantation to prevent transplant rejection.
Are there any prospects that modern methods already exist? If we talk specifically about the invention of new methods in the treatment of ankylosing spondylitis, then there are none yet. However, a cytostatic drug called Methotrexate is used. Its action is aimed at reducing the functional abilities of the immune system, which helps slow down the progression of the pathology.
Many patients are afraid of the fact that they will have to use oncological drugs. It is immediately worth noting that in this case the dosage will be significantly less than for a malignant tumor, so they will not have an extremely negative effect on the body.
What other news in the treatment of AS is there today? It is worth noting the drug Sufasalazine, which relatively recently began to be used in the treatment of rheumatic disorders. It is used for the same purpose as described above - to control the immune system and suppress the pathological process.
The discovery was made of biological drugs, which, according to experts, are much safer for humans and act directly on the source of inflammation. They can be used for quite a long time, but there will be no severe negative impact on tissues, organs and systems.
Surgical treatment of ankylosing spondylitis
If conservative therapy does not lead to an improvement in the condition, and the disease continues to progress, greatly reducing the patient’s quality of life, surgical treatment is recommended. Its tactics are determined based on the characteristics of the diagnosis and may include several types of surgical intervention, including:
- Vertebrotomy is the straightening of a deformed area of the spine due to resection of the posterior vertebral structures, followed by extension of the vertebral bodies to bring them closer to their normal position.
- Spondylodesis – fixation of vertebrae to each other is indicated for their instability, pathological lordosis and kyphosis. Abnormally fused vertebrae are separated, their correct position is restored and bone implants are installed between their surfaces, after which they are fixed with metal structures.
- Decompression operations are used to eliminate neurological disorders resulting from ankylosing spondylitis. Depending on the nature of the reasons for their development, microdiscectomy, nucleoplasty, kyphoplasty, vertebroplasty, etc. are used.
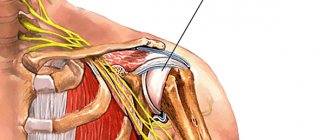
- Prosthetics using different designs is carried out if it is possible to replace the affected joint with an implant simulating its functions. Most often this is possible when the knee joints, hip, shoulder or pelvis are affected.
The primary goal of surgical treatment is to improve the patient’s ability to the maximum extent possible and reduce the risk of complications. But its success largely depends on the quality of the recovery period.
There is no strict treatment regimen for ankylosing spondylitis. For each patient, it must be selected individually, taking into account the degree of joint damage, concomitant diseases, age, nature of work activity and many other factors. The disease behaves unpredictably, but the doctors at SL Clinic are ready to fight with you for every vertebra and every joint using conservative and surgical methods, leaving no chance for it to rob a person of the joy of movement.
The cost of correction of hyperkyphosis in ankylosing spondylitis starts from 610,000 rubles and depends on: - The implant manufacturer; — Clinic (where the operation will be performed) and the class of the ward. The price includes: — Stay at the clinic before and after surgery; — Implants. — Operation; - Anesthesia; — Neurophysiological monitoring. — Postoperative observation. — Observation and consultation during the rehabilitation period. All clinic services and costs are shown in the price list
Features of symptoms
The most common symptom is back pain, which worsens during sleep and improves with exercise. In addition, a person may feel:
- moderate pain in the groin, sacrum;
- stiffness of movements;
- curvature of the spine and stoop;
- feeling of chest tightness;
- dizziness and tinnitus;
- swelling of the joints.
With ankylosing spondylitis, the temperature may also rise at the end of the day, weight may decrease, and the person will quickly get tired. The eyes may become inflamed, sometimes heart valve failure develops and difficulty breathing occurs. Complications in the functioning of the nervous system are not uncommon. Similar symptoms occur with arthrosis, osteochondrosis, spondylosis, rheumatoid arthritis, so it is very important to make a correct diagnosis.
Ankylosing spondylitis has symptoms similar to arthrosis