In vertebrology, vertebral lumbarization is relatively rare. This is a malformation of the bone skeleton, which can be congenital or acquired. It is very difficult to diagnose the pathology, since for a long time it gives absolutely no clinical manifestations.
At its core, lumbarization is the process of rejection of a vertebra from another part. It is quite difficult to say that lumbarization of the last thoracic vertebra has occurred, since absolutely no visible changes may be observed. The only characteristic sign is thickening of the body and arches of the lower thoracic vertebra and its slightly displaced position.
Much more often, lumbarization of the first sacral vertebra is observed. It is impossible to determine this pathology before a certain age (22–26 years). Only after the process of fusion of the vertebral bodies into a single sacrum is completed can one see on radiographic photographs that the uppermost vertebra remains mobile and has a dividing cartilaginous intervertebral disc. This process is called lumbalization. The name comes from the name of the lumbar region in Latin - lumbar.
Pathological changes can begin at an early age. Children aged 5–7 years may complain of tired back muscles. But they cannot explain what exactly bothers them. Therefore, adults often attribute these signs to childish whims. In adolescence, such children suffer from poor posture and weakness of the back muscles. At the first opportunity, they strive to relax their back muscles. It must be unbearable for them to sit without support on their back. This leads not only to back pain, but also to cramping in the thigh and calf muscles.
A round back, scoliosis, frequent colds, refusal to lead an active lifestyle - all these clinical signs should alert parents and become a signal to show their child to an experienced vertebrologist.
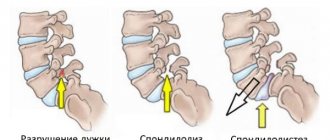
The treatment is based on the principle of rehabilitation - adaptation of the muscular frame of the back to the changed configuration of the lumbar spine. With regular visits to a chiropractor, sessions of therapeutic exercises, reflexology, massage and osteopathy, you can completely restore the functionality of the spine and reduce the risk of developing spondylosis, spondyloarthrosis and degenerative dystrophic dorsopathy.
In Moscow, you can make an appointment for a free appointment with a vertebrologist at our manual therapy clinic. The appointments are conducted by experienced doctors. The doctor will be able to make a preliminary diagnosis of lumbarization during the initial examination and examination. Based on the results of the initial consultation, individual recommendations for further treatment and examination will be given.
Underdevelopment of the sacrum: pathogenesis of lumbarization
Congenital defects of the spine are always associated with a violation of embryonic development, when the formation and laying of bones and organs of the nervous system occurs. One of the most important organs of the embryo is the neural tube, the rudiments of which are formed at 4-5 weeks of pregnancy. During this period, the fetus develops primary vertebrae (also called membranous vertebrae), consisting of a body and a neural arch. At the same time, areas of cartilaginous tissue are formed, which by 7-8 weeks of gestation will gradually begin to be replaced by bone structures.
Embryo development
The process of bone tissue formation in the sacral region differs significantly from other vertebrae, since additional ossification points in this segment of the spine appear only in the seventh month of intrauterine development. In total, the embryo develops 12-13 coccygeal and sacral vertebrae, which during the process of reduction fuse with other structures of the bone skeleton, and their number is reduced to 9-10 (5 sacral vertebrae and 4-5 coccygeal vertebrae). Complete fusion of the sacral vertebrae into a single sacrum occurs by the age of 17-20, but if the process of neurulation at the stage of embryonic development was disrupted, various anomalies and defects develop, one of which is lumbarization.
Causes of pathology of vertebral development
The additional segment is formed from a segment that would have been the first vertebra in the sacral region. Such separation from the sacral region of the back can be complete or incomplete. When completely separated from the lower section, it appears as a separate anatomical segment, and it is in this case that the sixth lumbar vertebra is determined. If the separation is incomplete, there remains a connection between the sacral region. Only a certain part of the first vertebra is separated, while the mobility of the lumbar region is significantly reduced, with pathological growth of bone tissue in the area of the joints of the lumbar region.
The appearance of an additional spine in the lumbar region does not have clinical significance for some time, because at the beginning of life, if it is a congenital anomaly, there will be no discomfort. But, given the load that the lumbar region receives from the upper parts of the spine, the formed soft bending line in this area is physiological. And the compensatory condition during the formation of the sixth vertebra forms an increase in the lateral curvature of the spinal axis, which will already be pathological and will cause not only pain, but also a weakening of the function of the lumbar region, as a result, a posterior displacement of the sacrum may appear. The complete formation of vertebral structures and the adaptive position of the vertebrae appear the basis for this type of anomaly at the age of 20-25 years is the beginning of its manifestation in the form of initial signs: rapid fatigue after exercise (physical). Sometimes there is the appearance of sharp pain in the lumbar region due to certain conditions (falling, lifting heavy objects), creating a factor for activating the clinical forms of the pathology. Repeated traumatization of the spinous processes resumes the appearance of pain after the use of anti-inflammatory drugs. As a result of the cause of secondary changes in soft tissues and circulatory disorders in the lumbar spine, resulting from increased load on this section, which, in combination with these changes, cause compression of the nerve root by the processes of the last lumbar and first sacral vertebrae. In this case, the sixth vertebra separated from the sacrum can put pressure on the sacrum itself and form sciatic syndrome.
Forms of manifestation of lumbarization
| Form | Ischial | Lumbar |
| Reason for appearance | The sciatic nerve is compressed, resulting in innervation of the buttock and lower limb area | Additionally, emerging trauma to the spinous processes causes torsional or rotational displacement of the anatomical position of the vertebrae |
| Signs | Skin sensitivity is impaired from the lumbar region to the thigh, with manifestations of pain in the buttocks and lower extremities | Aching pain in the spinal column and lower back. The difference from the sciatic form will be the cessation of pain after taking medications with an analgesic and anti-inflammatory effect |
Additional complications when changing the curvature of the spine create the risk of early development of deforming arthrosis in the lumbar region.
Consequences
The presence of an additional sacral vertebra causes the following consequences:
- the lower back becomes less mobile, as a result of which a person’s movements become constrained;
- the sacrum moves posteriorly, which affects posture and leads to the development of lordosis;
- the center of gravity of the body changes.
One of the most important consequences of lumbarization is the “slipping” syndrome: when the patient tries to lift a heavy object, the additional vertebra “slips”, and its processes put pressure on the sacrum and on the nerves extending from the spinal cord. The result is an attack of severe pain in the lumbosacral region.
Determining the cause of lower back pain
To possibly detect a congenital fusion, doctors use:
- radiography;
- computed tomography.
Thanks to a regular x-ray, it will be possible to see how many vertebrae are present, which will make it possible to diagnose sacralization or lumbarization. Both pathologies look similar on an x-ray, so you will need to recalculate the number of vertebrae. The image will also show what form of fusion is present - complete or incomplete.
The specificity of the diagnostic method is that the x-ray will show a decrease in height of the intervertebral disc. The examination will show whether the space between the lumbar and sacral vertebrae has narrowed or is missing. Using an x-ray, a specialist will determine exactly what type of sacralization the patient has - true or false.
With a false union, accumulations of calcium salts are visible between L5 and S1. An x-ray will allow you to see a gap in this segment that is to some extent hidden by ossified ligaments; their shadows are visible in the image.
It is sometimes not possible to count vertebrae on an x-ray
Thus, doctors pay attention to the anatomical formations near the sacrum
What is lumbarization and sacralization of the vertebrae
New lumbosacral vertebra - neoarthrosis
In the lumbar spine there are five vertebrae L1-L5, which are movably connected to each other due to the intervertebral discs and joints between the transverse processes. The sacrum consists of 5 fused vertebrae S1-S5, so in an adult it is a single bone, to which the coccyx, which is a rudiment of the tail, is movably attached. Lumbarization and sacralization of the vertebrae in the lumbar and sacral spine is a developmental defect that is characterized by changes in the structure and shape of the corresponding components.
- Lumbarization is a variant of the defect, characterized by the fact that the first vertebra of the sacrum does not fuse with the rest. It is mobile, therefore it is considered as the “additional”, “sixth”, L6 vertebra of the lumbar spine. The appearance of a transition, a new joint and a mobile 6th vertebra is called neoarthrosis. Lumbarization is established when there are six lumbar vertebrae.
- Sacralization - a developmental anomaly is accompanied by the fact that the last, fifth vertebra of the lower back fuses with the sacrum. At the same time, there are only 4 movable vertebrae in the lumbar region.
With age, compression of the nerve in the lumbar region occurs due to thinning of the cartilage discs, and constant pain occurs.
In a large number of cases, there are no changes in clinical symptoms for a long period. Over time, usually after the age of 40, the transitional lumbosacral vertebra causes compression of the spinal roots at the exit from the spinal canal. At the same time, the functional state of the thoracic and thoracolumbar spine changes. An inflammatory reaction develops around the pinched root, resulting in the following symptoms:
- Painful sensations in the lumbar and sacral areas, which have an aching, pulling character. They usually intensify after physical exertion or prolonged standing or sitting.
- The appearance of sharp pains while running, changing body position, bending, taking a deep breath or exhalation, which are called “lumbago” and can mean sharp compression of the spinal root.
- Gait disturbance. She becomes “shaky”, unstable.
- Discomfort appears while going down the stairs, but it disappears while going up. The manifestation of the symptom is associated with tension in the back muscles and additional pinching of the spinal roots.
- A noticeable reduction in the severity of discomfort in the supine position.
- Irradiation of pain into the right or left leg, while it mainly spreads along the back surface.
- Right- or left-sided numbness of the skin in the buttock area, the back of the leg, which can spread down to the foot. Sometimes, against the background of numbness, unpleasant sensations appear in the form of tingling and burning.
- Decreased muscle strength in the leg, which may be present on the left or right. Sometimes there is a two-way process.
Forms
There are two forms of lumbarization:
- complete lumbarization. The first vertebra of the sacrum completely loses its connection with the remaining vertebrae, forming an additional anatomical structure. On X-ray photographs, the vertebra “separated” from the sacrum looks like a vertebra of the lumbar spine;
- incomplete lumbarization. The first vertebra is partially connected to the sacrum. With this form of lumbarization, mobility of the lumbar region may be lost over time, which is associated with the appearance of bone growths.
Based on the morphology of the vertebra separated from the sacrum, two forms of lumbarization are distinguished:
- one-sided. In this case, the vertebra has signs of both the first sacral and the fifth lumbar;
- bilateral. The separated vertebra is similar in shape to either the first sacral or the fifth lumbar.
Shooting pains in the lumbosacral region in combination with spinal curvature and limited mobility can signal lumbarization s1
Complete, incomplete, partial, one-sided, two-sided - classification
https://www.youtube.com/watch?v=OqYeeDEsXRA
In medicine, congenital pathologies are divided into groups. There are sacralization:
- complete, in which the structural elements of the L5-S1 segment completely merge;
- partial - the vertebrae are fused with processes and arches, which is why their mobility is limited to some extent;
- deep, which is characterized by penetration of L5 into the sacral region without fusion of the vertebrae.
Anatomical pathology can be true or false. Varieties, taking into account the degree of fusion, are classified as true disorders, although some doctors consider the deep form to be a false type.
It is found, for example, in patients forced to be treated for ankylosing spondylitis, and in elderly people in whom ossification of the ligaments becomes a consequence of age-related changes. The classification of pathology provides for the presence of several more types of congenital conditions of the spinal column. Doctors distinguish fusion:
- bone;
- cartilaginous;
- articular
Bone sacralization is characterized by the complete absence of the intervertebral disc. When cartilaginous fusion develops, the disc is present, but only in a rudimentary form. With articular anomaly, the size of the disc decreases.
In the listed species, the form is either one-sided or two-sided sacralization.
Lumbarization is divided into the following types, regarding the separation of the first sacral vertebra:
- complete, in which S1 has no connection with other vertebrae of the sacral region, representing an anomaly of the sixth vertebra in the lumbar region. The photographs obtained during the examination of the patient clearly show complete lumbarization;
- incomplete, when S1 partially connects to the lower back without losing connection with the sacral region. This type of disease gradually begins to limit the motor activity of the lumbar region. This is due to the formation of bone growths. The patient is often diagnosed with spondylosis.
Taking into account the anatomical characteristics of the disease, lumbarization is divided into:
- bilateral - the first lumbar vertebra is identical to the last or first sacral;
- unilateral - S1 may be similar to the first sacral, and on the other hand - to the fifth lumbar vertebra;
Symptoms
Often the development of pathology occurs without the manifestation of noticeable symptoms, but in complex cases the following signs of the disease occur:
- Pain syndrome in the lumbar region. Symptoms appear in people under 30 years of age with all kinds of physical stress on the spine: bending the back, performing an unsuccessful jump, lifting heavy objects. Lumbarization of the s1 spine also manifests itself in pain discomfort in a standing position and relief after taking a lying position.
- The appearance of compaction in the lumbar lordosis. Upon palpation, noticeable enlargements of the spinal processes on the side are detected. Movement in this area is limited, and when palpated, the patient experiences acute pain.
- In a supine position, the patient experiences severe pain when trying to lift the lower limb. This symptom is often characterized by pain in the buttocks, and is associated with compression of the sciatic nerve by the processes of S1 or L5.
- Pathological changes in the spine may be accompanied by other diseases: osteochondrosis, scoliosis, etc.
- Often before the onset of pain, numbness is felt in the sacral area.
- Other noticeable symptoms may appear: non-standard gait, changes in the center of gravity, displacement of the spinal axis.
Classification
Depending on the form of formation and the degree of separation from the vertebra, lumbarization has two types:
- Incomplete lumbarization of the s1 vertebra, leading to the appearance of ruptures in individual vertebral segments, while maintaining the connection between the upper part of the sacrum with the rest of the spine. The disease develops with the appearance of pain symptoms and partial immobilization of the lumbar region.
- Complete separation provokes deformation processes in the upper part of the sacrum, leading to the appearance of a completely autonomous element belonging to the lumbar region.
As the disease progresses, the following types of anatomical changes appear:
- Unilateral separation - rupture of one side of the segment;
- Bilateral separation is a complete separation of a vertebra that becomes similar to the first vertebra of the sacrum or the outermost element of the lumbar region.
It is important to promptly identify the development of pathology, since lumbarization of the vertebra can lead to the onset of spondylosis - the appearance of bone growths around the articular processes. Localization of the disease can be of two types:
- Lumbar form: pain symptoms appear along the spinal column and lumbar region. Often the pain is aching in nature, which can be eliminated by simply taking anti-inflammatory drugs: Declofenac, Nise. With additional trauma with such pathology, acute pain occurs - lumbago. Similar sensations are caused by pressure on the spinous process of L5 and S1 due to a shift from their anatomical position.
- The sciatic form is characterized by pain spreading to the legs and gluteal area. The main reason for this manifestation of the disease is compression of the sciatic nerve emerging from the pelvic area into the buttocks, affecting the legs. Occasionally, pain is accompanied by changes in the sensitivity of the skin in the thigh or waist area.
https://youtube.com/watch?v=OqYeeDEsXRA
Rarely, pain occurs in the lower back when performing a jump with bent knees on the heels. In this position, the sacrum affects the lumbar region. With the formation of an additional segment, the length of the spine increases, the free space decreases, as a result of which the possibility of compression of the nerve roots by soft tissue increases. The appearance of pain forces the patient to limit his movements back and forth and in the lateral plane. In many cases, such a disease does not manifest itself in the form of clinical symptoms, and therefore does not require medical therapy.
Why is a spinal abnormality dangerous?
The sooner a deviation from the norm is detected, the less likely it is to develop serious complications. The absence of unpleasant symptoms is not a reason to refuse treatment for lumbarization of the S1 vertebra.
Ignoring the problem can lead to the development of the following pathologies:
- osteochondrosis;
- scoliosis;
- kyphosis;
- spondylosis.
In children, a mandatory medical examination upon admission to preschool and school institutions helps to identify pathological changes. If appropriate treatment is not carried out at this age, this will provoke the progression of other abnormalities against the background of underdevelopment of the sacral region.
These include:
- backward displacement of the sacrum when lifting weights;
- deterioration of blood circulation in tissues adjacent to the abnormal segment;
- radicular syndrome;
- violation of the spinal axis.
All these pathological changes negatively affect a person’s posture, the tone of the abdominal muscle tissue and the functioning of the pelvic organs.
Treatment of pathology
Due to the fact that the pathology is congenital, all treatment will be symptomatic.
That is, it is aimed at reducing pain and inconvenience caused by such deformation. Unfortunately, it is currently impossible to cure this disease even through surgery. But there are still some ways that can make the pathology less noticeable:
Therapeutic exercises and physical education. At a time when the pathology is not aggravated, therapeutic massage of the lumbosacral area and swimming are used. The main task of this activity is to eliminate muscle spasms. Since they very often accompany lumbarization and are one of the main reasons why pain occurs;
Nonsteroidal anti-inflammatory drugs. The main thing to remember here is that self-medication can lead to a deterioration in well-being. Therefore, you should not choose medications based on the experience of friends or the Internet. Go for a consultation with an orthopedic doctor, who will prescribe medications based on your individual characteristics. Such medications will help reduce pain and alleviate the patient’s general condition;
Consumption of vitamin B. Preparations with this vitamin (various ointments, preparations, etc.) improve blood circulation in the body. Such medications are used to reduce the number of muscle spasms and improve metabolism in the lumbosacral spine;
- Local blockade. This includes various injections with painkillers (Novocaine is usually used), electrophoresis. All this helps to significantly reduce pain;
- Impact on acupuncture points. Typically, acupuncture is used for this. Prevents muscle spasms, eases the general condition of the spine, relieves pain. The procedure should not be used without consulting a doctor, since in some cases such an effect can only cause harm;
Special corsets and belt. It is recommended to use such a device during physical activities (running, walking), in transport. Also used as a prophylaxis against pain;
Sanatoriums. In such institutions, patients undergo a full course of treatment, which includes all aspects of pathology treatment: sports activities, balneotherapy, etc. According to many patients, this method is very effective, as it is possible to forget about pain for a long time;
Avoid overload. Lifting heavy objects and prolonged static activities are prohibited. It is allowed to engage in physical therapy only, and then only after consultation with a doctor. For sleeping, it is advisable to choose a hard orthopedic mattress.
Surgery
Surgery is prescribed extremely rarely if the patient’s acute pain does not go away even after taking painkillers. An indication for surgery is also impaired spinal stability.
The purpose of the procedure is artificial fusion of bone segments. To do this, the S1 and S2 vertebrae are fixed together with an iron plate, and the lumbosacral region is immobilized using a special corset.
If artificial fusion is not possible, the S1 vertebra is fixed directly to the sacrum, and a special disc is installed between the bone segments S1 and S2.
Symptoms of pathology
Typically, back pain with this pathology appears at a young age (20-25 years). At the same time, many patients with lumbarization note that the pain syndrome first appeared acutely, against the background of lifting heavy objects, falling on straight legs, jumping or lateral bending of the body. There are two clinical forms of lumbarization: lumbar and sciatic.
With the lumbar form of lumbarization, patients are bothered by aching pain in the lower back and along the spine. An acute pain attack - lumbago - is possible. The pain usually disappears after taking anti-inflammatory drugs (Nise, diclofenac). The resumption of the pain syndrome is usually associated with additional trauma: increased load, lifting a heavy object, falling, etc. A characteristic sign of the sciatic form of lumbarization is the irradiation of pain to the buttocks and lower extremities. In some cases, in patients with lumbarization, a violation of skin sensitivity in the thigh or lumbar region is detected. The reason for the development of the sciatic form of lumbarization is compression of the sciatic nerve.
When examining patients with lumbarization, an increase or flattening of the lumbar lordosis is revealed. The mobility of the spine in the lateral and anteroposterior direction is usually limited. On palpation, moderate or minor pain occurs in the lower parts of the spine. The most painful point is determined on the side of the V lumbar vertebra. The sciatic form of lumbarization is characterized by a positive Lasegue symptom (increased pain in the buttock area and along the back of the thigh when trying to raise a straightened leg while lying on the back). A specific sign of lumbarization is pain in the lumbar region that occurs when jumping on your heels in a position with bent knees. In addition, there is an increase in pain when standing and a decrease in the lying position, as well as pain when going down the stairs, while going up does not cause any discomfort.
The main causes of back pain when an additional lumbar vertebra appears:
- Secondary changes in soft tissues;
- Poor blood supply to the spine due to increased load on the spine;
- Nerve root entrapment by the spinous process of L5 or S1;
- S1 pressure on the sacrum (formation of sciatic syndrome).
The lumbar form of lumbarization is characterized by pain in the lower back and along the spinal column. Most often they are aching in nature and go away after taking anti-inflammatory drugs (diclofenac, nise).
Acute pain (lumbago) with this pathology occurs after additional trauma to the spine. In such a situation, the spinous process of S1 or L5 presses on the sacrum due to their displacement relative to the anatomical position (torsion or rotation).
The sciatic form is characterized by irradiation of pain to the gluteal region and lower extremities. It occurs due to compression of the sciatic nerve (it emerges from the small pelvis in the gluteal region and innervates the lower limb).
Sometimes the pain syndrome is combined with impaired skin sensitivity in the lower back or thigh.
If there is an additional lumbar vertebra, the available space is reduced, increasing the likelihood of soft tissue compression of the nerve roots. Against the background of pain, there is limited mobility of the spinal column to the sides and in the anteroposterior plane.
All of the above changes are observed with severe pathology, when pinching of the nerve roots appears. In most cases, lumbarization s1 does not require treatment, as it does not lead to any clinical symptoms.
Reviews
Lumbarization of the S1 vertebra, according to doctors, does not pose a threat to human life. But the pathology requires timely treatment, which will eliminate the likelihood of developing secondary changes. The prognosis of specialists for both conservative therapy and surgery is favorable.
But it is worth understanding that throughout one’s life a person must observe restrictions associated with physical activity. Only careful attention to your health will help you maintain your full ability to move and lead a normal lifestyle.
Treatment methods
Treatment is indicated only in cases where the disease is accompanied by pain or leads to the development of scoliosis. During the formation of the spine, children and adolescents undergo periodic examinations in order to notice anomalies in time. If, in the presence of an additional lumbar vertebra, the remaining parts develop and function normally, such patients can live as usual.
The doctor selects the treatment regimen based on the type of lumbarization and associated complications. Basically, all methods are aimed at relieving pain and supporting the spinal column during its formation:
You can also read: Diagnosis of low back pain
- massotherapy;
- physiotherapy (electrophoresis, ultrasound);
- special physical education;
- wearing a fixing corset.
Excessive physical activity, sports, and falls are contraindicated for all patients. It is recommended to sleep on a hard mattress so as not to provoke mobility of the abnormal vertebra.
In some cases, surgery is performed to restore the last sacral vertebra. It is fixed with rigid metal structures, and pathological growths from the last lumbar vertebra are removed. Surgical intervention is necessary only when the pain syndrome cannot be relieved by conservative methods.
Lumbarization is not a reason to limit mobility and active lifestyle. The patient recovers both after surgery and during non-invasive treatment. The only limitation is related to lifting heavy objects. The patient will have to ensure that he does not lift more than the permissible weight throughout his life.
Some tips
Lumbarization is not amenable to drug treatment. And in order to maintain the condition of the spine and prevent complications from occurring, in addition to the use of basic therapy, the patient will have to follow several rules throughout his life:
- Sleep only on hard surfaces. Patients with lumbarization are recommended to choose anatomical mattresses with an increased level of hardness for sleeping.
- Do not lift heavy objects. People with this pathology should not lift objects whose weight exceeds 3-4 kg. This must be taken into account not only in everyday life, but also when choosing a profession. Such patients are prohibited from working as storekeepers, loaders, builders, etc. If there is still a need to lift a heavy object from the floor, before doing this, you must first sit down and only then pick up the thing.
- Limit physical activity. You cannot engage in heavy sports or make sudden movements.
By systematically following all these rules and medical recommendations, the risks of complications and impaired motor functions are reduced to a minimum. As practice shows, almost 80% of patients fully retain the ability to move throughout their lives.
It is necessary to understand that lumbarization is a harmless pathology. With the right approach to treatment, you can live with it for many years. However, the lack of adequate treatment can lead to the development of other spinal problems that can lead to disability.
Last news
Quite recently, a unique program of the Union State to help children with pathologies and spinal deformities, developed by leading experts in the field of vertebrology from Russia and Belarus, was launched.
Today, these plans have been put into practice, giving the first little patients a healthy future, without pain and limitations.
In the news release of the Diyor 24 TV channel, a report was released from the Namangan region of the Republic of Uzbekistan about the visit to the regional hospital of traumatologists from the Research Institute of Traumatology and Orthopedics, Tashkent, and Professor S.V. Vissarionova from the Research Institute of Children's Orthopedics, St. Petersburg.
Pushkin (suburb of St. Petersburg), Parkovaya street 64-68, Federal State Institution “NIDOI im. G.I. Turner"
source
Types of anomalies
Klippel-Feil syndrome
Short neck syndrome or Klippel-Feil syndrome consists of concretion (fusion) of the cervical vertebrae. Sometimes not only the cervical, but also the upper thoracic vertebrae are fused together. The anomaly is manifested by a pronounced shortening of the neck, a decrease in the hair growth limit, limited movements when turning the head to the side, and a “proud head position” (the head tilts slightly backward). In some cases, patients with Klippel-Feil syndrome have pronounced folds of skin from the ears to the shoulders.
Short neck syndrome is diagnosed based on symptoms and X-ray data of the cervical spine, and is often combined with other anomalies of the spine (cervical ribs, Spina bifida), cardiovascular and nervous systems. Neurological symptoms may be absent. In some cases, compression of the roots is possible, accompanied by impaired sensitivity, decreased hand strength, or paresis.
Cervical rib syndrome
As a rule, it is asymptomatic and is detected accidentally during an X-ray examination. Sometimes symptoms characteristic of a cervical rib appear after an infection, injury or hypothermia. Patients may be bothered by pain, weakness in the arm muscles, accompanied by disruption of normal vascular tone and skin nutrition (sweating, cold, pale, bluish skin).
Spina bifida
The most common developmental anomaly of the spinal column. In most cases, spina bifida is caused by non-fusion of the arches of the fifth lumbar or first sacral vertebra. Nonfusion of the arches of other vertebrae and splitting of the vertebral body are detected less frequently.
The closed version of the pathology is more common. It may be asymptomatic or accompanied by moderate pain in the lumbar and sacral areas. With the development of cicatricial changes in the area of the roots, sensitivity disorders and paresis appear along the innervation of the compressed nerve. The regulation of vascular tone and skin nutrition are disrupted, causing the development of edema and the appearance of ulcers.
Open clefting is less common. Affects 1 in 1000-1500 newborns. The pathology belongs to the category of severe anomalies, accompanied by other congenital defects (spinal cord dysplasia, impaired development of the roots and membranes of the spinal cord). A particularly unfavorable option is a defect in which not only the vertebrae are split, but also the spinal cord. Through the splitting of the vertebra, the membranes and substance of the spinal cord protrude outward.
In the area of the newborn's back, at the level of the cleft, there is a hernial protrusion, not covered by muscles and skin. The hernial sac may contain only the membranes of the spinal cord (meningocele) or the membranes and substance of the spinal cord (meningomyelocele). In severe herniations of the spinal cord, sensory disturbances, trophic disorders, and disturbances in motor and pelvic functions are detected. Spina bifida is diagnosed using a CT scan of the spine. MRI is performed to visualize soft tissue structures (spinal cord, ligaments, intervertebral discs).
Lumbalization and sacralization
Fusion of the sacrum with the fifth lumbar vertebra and separation of the first sacral vertebra from the sacrum can be asymptomatic. When the roots are compressed, sensitivity disorders, paresis and trophic disorders develop in the area of innervation.
Wedge-shaped vertebrae
A common developmental anomaly of the spine. Unlike ordinary vertebrae, wedge-shaped vertebrae (hemivertebrae) consist of a hemibody and a semi-arch with a spinous process. They can occur in all parts of the spine. They are one of the reasons for the development of scoliosis.
Diagnostics
To make a diagnosis, you need to undergo a number of examinations:
- visual inspection. The doctor needs to determine whether there is lordosis in the lumbar region accompanying lumbarization. It is also important to determine whether there are restrictions in movement in the lumbar region;
- X-ray examination. This method is the most accurate. To make a diagnosis, it is necessary to take a picture in two projections;
- SCT, MRI. These methods are required to identify lesions in the soft tissues surrounding the spinal column.
[node:field_similarlink]
Effective treatments
Since S1 lumbarization is a congenital disease, therapy is based on eliminating symptoms; it is not yet possible to influence the disease in other ways. The pathological process is incurable, surgical intervention is indicated only in advanced stages of the disease, when the patient suffers from acute attacks of pain and the mobility of the lumbar region is limited.
The main methods of treating S1 lumbarization include:
- carrying out therapeutic exercises. Manipulations allow you to strengthen the muscle corset, increase the range of movements, and reduce the severity of pain;
- massage, acupuncture. The procedures initiate blood circulation and metabolic processes, reduce discomfort, and have a positive effect on the patient’s well-being;
- taking NSAIDs, muscle relaxants, vitamin B. The doctor chooses specific medicinal products, taking into account the clinical picture and the severity of discomfort.
Self-therapy can lead to aggravation of the situation, so consult a doctor and start proper treatment.
Diet for lumbarization
Diet for rheumatism
- Efficacy: therapeutic effect after 2-6 months
- Terms: 2-6 months
- Cost of products: 1800-1900 rubles. in Week
There are nutritional approaches aimed at maintaining spinal health. The main recommendations include:
- regular consumption of white meat;
- enriching the diet with raw seeds and sprouts of sprouted wheat grains;
- meeting the body's needs, mainly consuming dairy products, cereals, vegetables, dried fruits and their fresh analogues;
- ban on caffeine, synthetic and fast food products;
- maintaining weight by limiting simple carbohydrates.
How to recognize anomalies of joint tropism?
This congenital anomaly mainly occurs at the level of the V lumbar (L5) and I sacral (S1) vertebra. Rare cases are pathologies localized in the III and IV (L3, L4) IV and V (L4 and L5) vertebrae of the lumbar spinal column. Anomaly of tropism is characterized by incorrect orientation of the vertebrae according to the axis, for example at the level of the presacral articulation - one of them is not located sagittally, like the others, but vertically. It is accompanied by the following structural deformations:
- Wedge-shaped process. Occurs as a result of underdevelopment.
- A triangular-shaped formation at the anterosuperior corner of the body, called the persistent apophysis.
- Uneven length of the articular processes of the vertebrae.
- Agenesis.
- Nonfusion of the vertebral arches.
- Not fusion of bodies (typical for the thoracic region).
- Non-fusion of the arches on both sides, spondylosis (occurs in the lower back).
Intervertebral joints, which are already improperly aligned, serve as a target for inflammation and the development of dystrophies. They are characterized by degenerative changes in the facet joints. The occurrence of severe pain and decreased tendon reflexes is based on the fact that the roots of the spinal cord are compressed by ossified and scar tissue. The lower back muscles are tense, which also aggravates the condition. It is painful for a person to bend and turn. Sedentary work creates discomfort. A history of trauma and a sedentary lifestyle contribute to the progression of pathological symptoms. Often, pain can occur after hypothermia. The pain appears in the following places:
- paravertebral points;
- vertebral area;
- when bending your back forward;
- localization of the spinous processes.
Instrumental diagnostics
Differentiation of tropism is carried out with fractures, separations of bone and cartilaginous growths, and calcification of the ligament. In making an accurate diagnosis, the main role is played by:
- X-ray (shows vertebral asymmetry);
- spiral computed tomography;
- MRI.
Why does an additional vertebra appear in the lumbar region?
An additional vertebra is always a pathology that negatively affects the configuration and functionality of the entire musculoskeletal system. Its presence leads to deformation of large joints of the lower extremities, entails a change in posture, a displacement of the conditional center of gravity of the human body and a number of other pathological changes
It is very important to promptly identify an additional lumbar vertebra and carry out full rehabilitation in order to reduce the risk of degeneration and dystrophy of the cartilage tissue of the intervertebral discs and large joints of the lower extremities
It is important to understand why such an anomaly appears and how this orthopedic problem can be effectively prevented. According to recent medical research, the following pathogenic factors are believed to be potential causes of lumbarization:
- anomalies of intrauterine development provoked by the mature age of the expectant mother and her consumption of strong alcoholic beverages during pregnancy;
- compensatory reaction in response to the development of spinal deformity in the thoracic region (for example, with scoliosis);
- degenerative dystrophic dorsopathies, in which reflex overstrain of the muscular frame of the back occurs;
- maintaining a sedentary lifestyle;
- predominantly sedentary work;
- atony of the muscular frame of the back;
- development of spinal pathologies (ankylosing spondylitis, spondyloarthrosis, protrusion and hernia);
- excess body weight;
- systemic pathologies in which inflammation and destruction of cartilage and connective tissues occur in the human musculoskeletal system;
- dysplasia and fibrodysplasia of cartilage tissue;
- incorrect foot placement;
- degeneration of large joints of the lower extremities;
- short leg syndrome.
An additional vertebra in the lumbar region can form after a back injury. Bruises, sprains, ruptures of tendon and ligament tissue lead to increased lability of the first sacral vertebra. Partial deformation of the cartilage tissue of its intervertebral disc also entails an anomaly in the process of fusion with the sacrum.
In athletes, lumbarization of the sacral vertebra is the limit of the physiological norm. Especially if the type of professional occupation is associated with the need to develop excessive flexibility of the spinal column.
Anatomical features
The sacrum is the last element connecting the spine to the pelvis, which undergoes heavy loads every day. All vertebrae of the sacrum in the standard state do not move, and are interconnected by a special connective tissue: syndesmoses, similar in structure to intervertebral discs, but differing in a more durable composition. The special structure of this section makes it possible to support subsequent elements of the spine.
Lumbarization is the appearance of a separate part of the sacrum during the development of the spine when the upper part of the sacral spine is not fused with the neighboring parts.
The length of the lumbar region increases, which when lifting heavy things leads to a shift in the newly formed part of the spine. Lumbarization changes the structure of the spine, causing pain and provoking the appearance of scoliosis.