Tendinitis, also known as tendinosis, is an inflammatory disease of the tendons, or more precisely, inflammation and degeneration of tendon tissue.
Occurs during heavy physical activity or injury to the tendons, for example during sports.
The disease is usually associated with acute trauma and inflammation. It often affects the elbows, wrists, fingers, thighs and other parts of the body.
The affected body parts have their own funny names and terms, such as Achilles tendinitis, tennis or golfer's elbow, jumper's knee and pitcher's shoulder.
Tendonitis can occur in men and women at any age, but is more common in adults who play sports. Older people are also susceptible to the disease because tendons tend to lose elasticity and become weaker with age.
Tendinosis has similar symptoms, but it is a chronic or long-term condition and is degenerative, meaning it is permanent and steadily progresses.
Quick Facts About Tendinitis:
Here are some key facts regarding tendonitis. More details are provided below in the main article.
- Tendinitis usually occurs due to overuse or damage to the tendons.
- Treatment includes rest, ice therapy, and prescription/over-the-counter pain relievers.
- Without treatment, the disease can lead to tendon rupture, which may require surgery.
What is tendonitis?
Tendon is a dense and elastic tissue that attaches muscles to bones. Flexible, strong and fibrous tendons can withstand enormous loads.
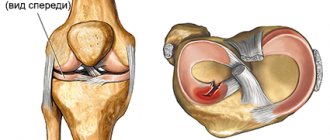
Ligaments connect the bones in the joints, and tendons connect the muscles to the bones, the swelling of these tendons is called tendinitis.
Tendons and ligaments work together to exert traction. Tendons and ligaments are tough and fibrous tissues, but are called soft tissues because they are soft compared to bone tissue.
If it is not the tendon itself, but the sheath around the tendon that becomes inflamed, the condition is called tenosynovitis. Tendinitis and tenosynovitis can occur together.
Location of the disease
Since there are a large number of tendons in our body, the disease itself, called tendonitis, can affect any part of the body.
Other terms are used as synonyms to refer to this disease: tendinosis, tendinopathy, or enthesopathy, if we are talking about damage to the tendon at the site of its attachment to the bone.
Kinds
Different types/types of tendinitis affect different parts of the body.
Achilles tendinitis
The Achilles tendon (calcaneal tendon) is located between the heel and the calf muscle.
Achilles tendonitis is a common sports injury.
The disease can also be caused by wearing the wrong shoes. The disease is also more common among patients with rheumatoid arthritis.
Tendinitis of the supraspinatus muscle of the shoulder joint
With supraspinatus tendinitis, the tendon around the top of the shoulder joint becomes inflamed, causing pain when you move your arm, especially difficulty lifting your arm up.
Some patients may find it painful to lie on the affected shoulder at night. If other tendons in the same area are affected, the patient may experience rotator cuff syndrome or impingement syndrome.
Tennis elbow or golfer's elbow (ulnar epicondylitis)
A common symptom of lateral epicondylitis, commonly known as tennis elbow, is pain on the outside of the elbow. The pain may radiate down to the wrist.
Medial Epidondylitis or Golfer's Elbow – Pain is felt on the inside of the elbow and is more common in golfers. The pain can also, in rare cases, extend to the wrist.
De Quervain's tenosynovitis (de Quervain's disease, stenosing tenosynovitis)
In stenosing tenosynovitis, the sheath surrounding the thumb tendon, between the finger and the wrist, becomes inflamed. With thickening and swelling in this area, it becomes painful to move the thumb.
trigger finger syndrome
Snapping finger syndrome occurs when the finger becomes locked in a bent position, causing the tendon sheath in the palm to become clouded and inflamed, preventing the tendon from moving smoothly. Sometimes a nodule forms along the tendon.
Wrist tendinitis
Occurs in badminton players and production line operators who repeatedly perform the same movements with the wrist. Tendinopathy is another type of injury that affects the tendons of the wrist. This is a degenerative condition, not inflammation.
Anatomy of the Achilles tendon
Developed Achilles tendon
present only in humans and is an evolutionary adaptation to upright walking. It is believed that the human musculoskeletal system has not yet had time to fully adapt to upright walking, so its individual elements experience increased loads.
Although evolutionary selection gave the Achilles tendon
high endurance (its tensile strength reaches 400 kg) and has made it the thickest tendon in the human body, it is nevertheless considered one of the most vulnerable.
The Achilles tendon from above, in its widest and thinnest part, is attached to the fusion of the heads of the triceps muscle (formed by the gastrocnemius and soleus muscles), and from below, tapering at a level of 3-4 cm above the heel bone, it is attached to the calcaneal tubercle.
Due to its anatomical features, the Achilles tendon
is responsible for normal supination and pronation of the foot (the main biomechanical processes that occur during human movement). It also provides anatomically correct movement and stability in the knee, ankle and subtalar joints.
Mechanical properties of the Achilles tendon
fully correspond to these tasks: when running, it can withstand loads that are 8 times the weight of the person himself.
Causes and risk factors
Common reasons include:
- sudden injury;
- heavy physical activity;
- constant (same) movements for a long time.
Tendonitis often develops in people whose activities involve repetitive movements.
Other risk factors include:
Age : Tendons become less flexible as adults age and are more susceptible to injury.
Profession : A person whose work involves repetitive movements, work in uncomfortable and uncomfortable positions (painters, production workers), heavy loads, suffers most from the disease.
Sports : Some sports involving repetitive movements can lead to tendonitis, for example:
- run;
- tennis;
- swimming;
- basketball;
- golf;
- bowling;
- baseball.
Diseases
: People with diabetes and rheumatoid arthritis are more likely to develop tendonitis.
If the pain suddenly intensifies or the joints become suddenly stiff, the person should seek medical help immediately.
Epidemiology/Etiology
An injured tendon has a higher rate of matrix remodeling, resulting in mechanical instability and increased susceptibility to injury. The results of histological studies of samples taken from patients with established tendinopathy show either no or minimal significant inflammation. Typically, they indicate proliferation, loss of collagen fiber density, increased proteoglycan content, and neovascularization. Inflammation appears to play a role only in the initiation, but not in the spread and progression of the pathological process.
Previously, it was believed that failure to heal and the resulting tendinopathy of the tendon was associated with chronic overload, but subsequently the same histopathological characteristics were described in tendons that were not overloaded. Lack of load on the tendon is accompanied by the same changes in cells and matrix as in the case of an overloaded tendon. This also leads to a decrease in its mechanical strength.
Diagnostics
The doctor will first ask about symptoms and perform a physical examination of the patient. The most obvious sign for a doctor upon examination will be a grinding sound (an unpleasant creaking sound), it occurs because the tendon sheath becomes thicker and becomes inflamed.
The following studies may also be required:
- Diagnostics by ultrasound (ultrasound examination (ultrasound));
- Magnetic resonance imaging (MRI);
- X-ray (helps detect calcium in tendons).
Physical therapy
The use of eccentric exercises has been proposed to accelerate tendon remodeling through the formation of interfiber bonds. What causes tendon healing in the eccentric mode is not known for certain, but it is assumed that the forces generated during eccentric loading are greater than during concentric exercises.
It is possible that eccentric exercise not only has a beneficial mechanical effect on the tendons, but also acts on pain mediators, reducing their presence in the affected tissues. In any case, the positive effects of eccentric exercise are evidenced by studies conducted on athletes and people leading a sedentary lifestyle.
However, there are many questions regarding what variables can influence the outcome of training: should the training be painful, how long should it be, what method of progression should be chosen, etc.
To date, three basic principles have been formulated for the eccentric training regime:
- Tendon length - if the tendon is pre-stretched, its length at rest will be greater, and the tension during movement should be less.
- Load – by gradually increasing the load on the tendon, we can expect an increase in its strength.
- Speed – Increasing the speed of contraction requires more force.
However, more research is needed to confirm these conditions.
Treatment
All therapy is aimed at relieving pain and reducing inflammation.
In many cases it is enough:
- give your joints a rest;
- conduct heat and cold therapy;
- take prescription/over-the-counter pain relievers;
- splinting the damaged joint (application of immobilizing splints and bandages for injuries).
Rest
Rest and rest will relieve inflammation. If tendinitis is caused by sports activity or typing (the same type of activity), the person should take a break from this activity or reduce the intensity at which they were working.
Immobilization splints and bandages will help reduce movement. In severe cases, bed rest with a splint may be required.
If you don't take a break and rest, this can lead to serious complications.
Warm and cold
An ice pack or warm towel can relieve pain and swelling in the affected area.
An ice pack can be applied for 10-15 minutes 1-2 times a day.
Important! Do not apply ice or cold products directly to the skin. Wrap them in a towel.
Taking a warm bath, applying a moderately hot towel, or applying gels, creams and ointments to warm the affected area may also help.
Ice is best used for injuries that occurred within the last 48 hours. After this, applying a hot towel will be the best option.
Painkillers and warming ointments
- Over-the-counter pain relievers : Ibuprofen, Paracetamol, Pentalgin and other non-steroidal anti-inflammatory drugs (NSAIDs) usually help with tendon pain.
- Warming ointments: Bystrumgel, Finalgon, Apizartron will help relieve pain and reduce replenishment.
- Corticosteroid injections : Injections near the tendon will help relieve symptoms of tendinitis. However, repeated injections can weaken the tendon, greatly increasing the risk of rupture.
- Physiotherapy : Rubbing and massaging the affected area will reduce pain and speed up the healing process.
- Stretching and exercise : A physical therapist may also prescribe specific exercises designed to stretch and strengthen the affected tendon and muscles.
Shockwave therapy and surgery
If the disease persists for a long time and calcium salt crystals are deposited in the tendons, extracorporeal shock wave therapy (ESWT) can be tried. The shock wave will pass through the skin, destroying calcium deposits. The deposits can also be removed surgically.
Without proper treatment, tendonitis can lead to tendon rupture. This is a more serious disease, which in 80% of cases requires surgical intervention.
FORECAST
With timely consultation with specialists and competent treatment with strict adherence to all doctor’s recommendations, the prognosis for complete recovery is favorable. In such cases, it is possible to completely stop the inflammatory process and minimize the risks of relapses. Chronic tendonitis requires long-term therapy and, unfortunately, can rarely be completely cured. But with proper management of the patient, doctors are able to achieve long-term remission.
At the Center for Restorative Medicine in Naberezhnye Chelny you can make an appointment with an orthopedist. Prices for consultation with a specialist can be found on the website or clarified by phone,
Prevention
The occurrence of tendonitis will be less likely if a person adheres to the following preventive measures:
- Exercise : Activities to strengthen the muscles around the tendon can help prevent tendonitis from recurring. It is important to seek professional help from a physiotherapist; he will prescribe a set of exercises.
- Stretching : Stretching is essential when playing sports. Proper stretching will prevent the development of tendonitis.
- Repetitive movements : These can significantly increase the risk of developing or continuing tendinitis.
It is also advisable not to stay in one position for too long, especially if you feel uncomfortable. It’s better not to be distracted for long, rest and return to work later.
Symptoms of tendinitis
This disease can be diagnosed by a number of symptoms.
Among the main ones:
- redness on the skin;
- pain (from mild to severe);
- creaking sound;
- stiffness in the morning;
- swelling of tissues;
- hyperthermia of the damaged area;
- increase in body temperature.
How to recognize tendonitis in common wrist pain, learn from Dr. Karpinsky:
The more significant the damage, the more noticeable the symptoms. With weak development of tendinitis, unpleasant sensations appear when moving. If diagnosis and treatment are neglected, inflammation will cause scarring. Next is joint immobility.
With Reiter's disease, a rheumatic disorder, a clear symptomatic picture of Achilles tendonitis is observed. The pain appears unexpectedly, is long-lasting and intense. When you touch the inflamed area, it intensifies. Unpleasant sensations increase towards night.