Traumatologist-orthopedist (adults and children)
Bogatov
Victor Borisovich
21 years of experience
Highest qualification category. Doctor of Medical Sciences, Professor of the Department of Traumatology and Orthopedics, First Moscow Medical University. I.M. Sechenov.
Make an appointment
Tendonitis is a disease that manifests itself as an inflammatory process in the tendon area. Pathology can occur in acute or chronic forms. In the second case, degenerative processes develop in the affected tendon. In most cases, the source of inflammation is localized in the tissues adjacent to the bone. Symptoms of tendonitis are nonspecific: the patient suffers from pain when moving the limbs and local fever. The formation of mild edema and a zone of moderate hyperemia is possible. Treatment of pathology in the initial stages involves the use of conservative techniques. An advanced inflammatory process may require surgical intervention.
General information
Tendonitis occurs in patients of all ages. The risk group includes professional athletes and people engaged in monotonous physical labor. The source of inflammation is formed due to excessive stress to which the human tendons are exposed. Tissue microtraumas cause pain and increased local temperature.
Most often, the pathology affects the tendons located next to the elbow, knee and hip joints. Less commonly, inflammation develops in the ankle and wrist joints. Age-related changes in joint tissues lead to weakening of ligaments - the likelihood of developing inflammation increases. Patients over 60 years of age may suffer from the deposition of calcium salts, leading to the appearance of a calcifying form of the disease.
Tenosynovitis
Tenosynovitis is an inflammation of the tendon and its surrounding membranes, also known as synovial membranes.
Some tendons are covered with synovial membranes, but some tendons are not covered. The synovium produces a small amount of oily fluid that is secreted into the space between the tendon and its synovium. This oily fluid helps the tendon move easily and without resistance when the bone to which the tendon is attached moves. Common signs of tenosynovitis are pain, swelling and tenderness in the joint area. In most cases, it is necessary to sharply reduce movement in the inflamed joint to allow for faster recovery. Often, the pain lasts for several days and disappears without any treatment. But in other cases, pain and swelling persist for many months, especially if no treatment is given.
Any tendon in the human body can be susceptible to tenosynovitis, but there are certain areas that are most susceptible to this pathology. For example, the hand and wrist, since they are often used to perform the same type of repetitive movements.
While there is no actual evidence to suggest what exactly can prevent tenosynovitis from occurring, it is still recommended to avoid repetitive movements as much as possible. Nowadays, there are certain exercises to strengthen the muscles surrounding the damaged tendons.
Reasons for the development of pathology
Symptoms of tendinitis identified by an orthopedist during an examination of the patient may indicate the causes of inflammation in the tendon. Often tissue microtraumas result from a high level of human motor activity. The pathology is common among professional tennis players, golfers, javelin throwers and skiers. The monotonous movements typical of gardeners, carpenters or painters often cause inflammation of the tendons.
A quarter of clinically diagnosed cases of tendonitis develop under the influence of other factors: rheumatic pathologies or diseases of the thyroid gland. Inflammation of the tendons can be a consequence of gonorrhea, intoxication of the body or abnormalities of the bone skeleton (different lengths of limbs, etc.).
Pathogenesis
Tendons are formed in the form of dense, inelastic cords consisting of bundles of collagen fibers. Thanks to them, muscle tissue connects to bones. Tendons provide the transmission of movement from muscles to the skeleton and maintain stable joint function. Intense and monotonous movements interfere with the process of natural restoration of collagen fibers - the first signs of tendinitis appear.
The tendon structures swell and individual strands of collagen begin to break down. If the load remains high, foci of fatty degeneration, necrosis and deposition of calcium salts form in the tissues. Hardened calcifications lead to re-injury of the previously damaged area. The inflammatory process gradually spreads to the entire tendon.
Hand tendinitis: ICD 10
Tendinitis is a disease in which the inflammatory process is localized at the site of bone attachment or muscle-tendon junction. Tendonitis of the hand ICD 10 has the code M65, this code includes synovitis and tenosynovitis. After a comprehensive diagnosis, a specialist determines the nature of the disease and the characteristics of its course, after which an additional index is assigned.
Patients who come to the Yusupov Hospital with signs of tendinitis undergo a comprehensive examination. Detection of the pathological process at an early stage is possible through the use of high-precision European equipment. In addition, specialists establish the causes of the disease and associated disorders that could provoke the inflammatory process.
Types of pathology
Tendinitis can affect tendons of any size - inflammatory processes develop in the tissues of the finger, hand, foot, elbow or knee. The classification of pathology used by orthopedists takes into account the localization of the source of pathology. Doctors distinguish the following forms of the disease:
- lateral,
- medial,
- inflammation of the patellar tendon,
- inflammation of the tendon of the shoulder joint.
The lateral type of pathology develops in the tendons adjacent to the wrist muscles (extensor brevis and longus, brachioradialis muscle, etc.). The patient experiences pain spreading along the outer surface of the elbow joint. Over time, professional and amateur athletes develop hand weakness. A person begins to experience difficulty performing basic actions: twisting clothes, lifting a cup of drink, shaking hands.
The medial form of the disease affects the tendons adjacent to the flexor muscles of the forearm, elbow and palm. The pathology is diagnosed 7–10 times less frequently than lateral tendonitis and develops in individuals who regularly perform rotational movements of the arms. Those at risk include golfers, seamstresses, professional scorekeepers, gymnasts, tennis players and baseball players. The main symptom of the disease is acute pain localized on the inside of the elbow joint.
Inflammation of the patellar tendon is diagnosed in people who frequently perform jumps. Microtrauma is caused by short-term intense loads on the quadriceps muscle. In the initial stages of development of the pathology, pain occurs after the patient completes physical activity. Later, pain appears during exercise or at rest.
Inflammation of the shoulder tendons affects the tissue adjacent to the rotator cuff muscles. Pain occurs during any activity that requires hand mobility. Acute attacks can develop at night. An increase in the size of the focus of inflammation leads to the formation of pronounced edema.
Etiology
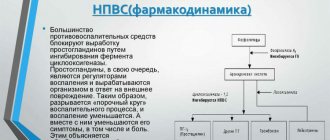
Inflammation is a complex pathophysiological reaction that develops as a result of tissue damage. In the area of the pathological process, cells of the immune system accumulate, which produce certain biologically active compounds (prostaglandins) that respond to the characteristic manifestations of the inflammatory reaction (pain, tissue swelling, hyperemia). The main provoking factors leading to inflammation are:
- Intense physical activity on the shoulder.
- Previous injuries that affect the cuff to varying degrees (fall on an outstretched arm, bruise, dislocation, fractures of the upper third of the humerus).
- Infectious inflammation, which is the result of the activity of pathogenic (disease-causing) or opportunistic microorganisms.
- Aseptic inflammation developing against the background of local hypothermia in the shoulder area.
- An autoimmune process is a pathology of the immune system in which antibodies are “erroneously” produced to one’s own tissues, in particular the structures of the musculoskeletal system.
- Degenerative-dystrophic processes in which the nutrition of the tissues of the structures of the musculoskeletal system is disrupted, leading to their destruction with the subsequent development of an inflammatory reaction.
After the doctor has diagnosed tendinitis of the supraspinatus tendon, treatment is prescribed taking into account the causes that led to the inflammation.
Symptoms
Symptoms of the disease appear gradually. In the early stages, the patient experiences pain at the time of maximum physical exertion. The rest of the time, the injured tendon does not cause any discomfort to the child or adult. Over time, the pain syndrome becomes more intense: discomfort occurs with minimal physical activity. If left untreated, the patient may be unable to perform everyday activities such as washing dishes, putting on clothes, fastening buttons, tying shoelaces.
The skin next to the source of inflammation turns red and swelling forms. Local temperatures may rise. Palpation of the tendon increases the pain. With sudden movements of the injured limb, the patient may hear a crunching or crackling sound.
Useful
Treatment of any type of shoulder tendinitis is not a quick process. Therefore, you should think about prevention - play sports according to the individual capabilities of the body, do a warm-up before any physical activity. You should consult a doctor at the slightest suspicion of problems. The earlier the pathology is detected, the easier it is to get rid of it.
We invite you to familiarize yourself with other equally useful information: about the symptoms and methods of treatment of rheumatoid arthritis, what treatment is required for gonarthrosis of the knee joint, and how to strengthen blood vessels using traditional methods. We look forward to your feedback, dear readers. If you are faced with a problem such as tendinitis of the shoulder joint, what treatment helped you?
Diagnostics
Diagnosis of tendinitis is performed by an orthopedist. The doctor examines the patient and collects data for anamnesis. Confirmation of the primary diagnosis is carried out through radiography, ultrasound and magnetic resonance imaging of the injured tendon.
X-rays can reveal foci of calcification that have formed in collagen fibers. Ultrasound imaging of tendons demonstrates tissue thickening and decreased echogenicity. MRI is used to determine the location of the inflammation and its size.
Treatment
The treatment strategy for tendinitis is determined by the orthopedist, taking into account the data obtained during diagnostic procedures. In case of severe pain, the patient is advised to undergo short-term immobilization of the limb. Drug therapy includes anti-inflammatory drugs. Tissue swelling is eliminated through phonophoresis and electrophoresis.
Relief of the pain syndrome will allow the patient to begin therapeutic exercises. If acute pain persists, the child or adult receives glucocorticosteroid drugs by injection. The ineffectiveness of conservative therapy becomes an indication for surgical intervention.
During the operation, surgeons can perform complete or partial cutting of the tendons from the muscles for the purpose of subsequent lengthening. The postoperative rehabilitation period can last several months.
Prognosis and prevention
Timely initiation of treatment for inflammatory processes in the tendons allows doctors to form a favorable prognosis for most patients. When the pathology is advanced, systematic relapses and severe injuries to the extremities are likely. Surgical treatment allows for complete restoration of limb mobility in 85–90% of cases.
Prevention of tendinitis is based on avoiding excessive stress on the tendons. Amateur and professional athletes should do a thorough warm-up before starting training or competition.