What it is
Myositis of the back muscles is called inflammation of the muscle fibers , in which hard, painful nodules form in the muscles - foci of inflammation. Often the pathology becomes chronic and leads to a serious complication - muscle atrophy.
Clinical picture
Myositis of the back muscles is characterized by the appearance of local aching pain in the back with increasing intensity , which intensifies with movement. In some forms of the disease, dense cords and nodules can be found in the affected muscles - sources of inflammation that respond with severe pain upon palpation. Swelling and swelling of the muscles may also occur.
As for purulent myositis, it proceeds completely differently . In this case, the inflammatory process is accompanied by fever, chills, and a gradual increase in pain. In this case, the muscle often becomes denser and remains in a state of constant tension.
Myositis is characterized by inflammation of the muscle fibers of the muscles
Classification
There are two main forms of the disease:
- Spicy . It comes up unexpectedly. Characterized by the appearance of severe pain. It develops against the background of sudden muscle tension, acute infections, and injuries. If left untreated, it can become chronic.
- Chronic . The danger of chronic myositis is that it is practically asymptomatic, so a person may not be aware of the presence of the disease for a long time. Pain in this form of the disease occurs rarely, intensifying with adverse effects - hypothermia, changes in weather conditions, prolonged exposure to an uncomfortable position.
The following forms of myositis are also distinguished::
- infectious;
- parasitic;
- toxic;
- myositis in combination with autoimmune pathologies;
- ossifying;
- polymyositis.
Prevalence and significance
Myositis of the back muscles is a fairly common pathology . The disease can occur in a person of any gender and age. Most often, myositis develops in the lumbar spine, less often in the thoracic and cervical regions. Treatment is carried out by traumatologists and orthopedists.
Diagnosis of myositis at the Med&Care clinic
As mentioned above, different forms of the disease have their own clinical picture. If myositis is suspected, a neurologist at our clinic will interview and examine the patient and prescribe the necessary tests and studies.
The most informative instrumental diagnostic method for myositis is ultrasound of soft tissues and ultrasound angiography. Our medical center uses modern expert class ultrasound equipment TOSHIBA APLIO CV. It allows you to detect inflammation of muscle tissue (foci of hyperechogenicity), fibrous layers (hypoechoic areas), abscesses and other pathological processes.
To confirm the diagnosis, electromyography is sometimes used to help evaluate the electrical activity of muscles.
The following are a good help to the doctor:
- General blood analysis. It allows you to confirm or exclude infectious myositis (accompanied by an increase in ESR, the number of leukocytes and neutrophils) and a parasitic form of pathology that provokes the growth of eosinophils.
- Blood test for creatine phosphokinase. Exceeding the permissible norms of this enzyme indicates damage to muscle cells.
- Rheumatic tests that help identify local or systemic autoimmune diseases. Of particular diagnostic value is the analysis for myositis-specific autoantibodies (MSA).
- Biopsy. Taking a biopsy allows you to see structural changes in muscle tissue, the vessels that feed it and nearby connective tissue.
Risk factors, causes
Most often, myositis develops due to bacterial and infectious diseases. The inflammatory process can occur for the following reasons:
- hypothermia;
- are in the midst of or have recently suffered acute viral infections;
- parasitic muscle damage;
- bacterial infections;
- damage to the back muscles (traumatic or as a result of seizures);
- autoimmune lesion;
- toxic damage;
- long-term static load on certain muscle groups.
Most often, myositis occurs due to prolonged exposure to an uncomfortable position, tension of individual muscle groups. Therefore, violinists, drivers and PC operators have a much higher chance of getting myositis than representatives of other professions.
Consequences
The most unpleasant manifestations of myositis are pain and muscle tension. When the first signs of the disease appear, exposure to the cold and physical activity should be minimized. Otherwise, the disease may develop into a protracted form.
Lack of treatment leads to inflammation of new muscle groups and skin , the appearance of intense weakness in the muscles and their shortening. The most dangerous consequence of the disease is muscle atrophy.
Video: “Myositis and myalgia”
Treatment depending on location
Myositis affects any muscle group. The set of therapeutic measures depends on the location of the pathology.
Pain concentrated in the cervical spine indicates myositis of the neck. A sample list of assignments would look like this:
- anti-inflammatory drugs for internal use;
- local application of creams and ointments with a warming, antispasmodic, analgesic effect;
- massage to eliminate spasms, restore blood circulation, improve neck mobility;
- physiotherapeutic procedures to speed up recovery.
The inflammatory process in the muscles of the back and lumbar region most often occurs as a result of a cold, hypothermia, or after high physical activity. Myositis is differentiated from kidney diseases, spinal osteochondrosis, and then treatment is prescribed. The therapy program stipulates bed rest and restriction of movements for the duration of acute pain. Analgesics are prescribed in the form of injection blockades and for internal use, NSAIDs, hardware muscle traction, and reflexology.
Myositis of the chest is often accompanied by an increase in body temperature. Under these conditions, the patient is prescribed bed rest. The main task is to stop the cause of inflammation. To alleviate the condition, painkillers and anti-inflammatory drugs are prescribed. If there is a bacterial component, antibiotic treatment is carried out. For autoimmune pathology, the treatment program includes immunosuppressants and glucocorticosteroids. Electrophoresis of the thoracic region is prescribed as maintenance therapy during recovery. Acupuncture and hirudotherapy have a good effect.
For myositis of the extremities, muscle rest is provided at the initial stage of treatment. It is necessary to exclude any stress on muscles and joints. Injections and external agents are used for pain relief. To relieve the inflammatory process, NSAIDs are prescribed. Thermal procedures are indicated in the absence of swelling and redness. After stopping the acute process, massage procedures, exercise therapy, and reflexology are allowed.
Shoulder myositis is also treated comprehensively: anti-inflammatory therapy, anesthetics, and physiotherapy are used. Additionally, kinesiotherapy can be prescribed - a rehabilitation technique, a type of physical therapy, the purpose of which is to reduce muscle tension, reduce inflammation, and increase mobility. Kinesiotherapy also includes various types of therapeutic massage. The technique is effective for severe pain and functional disorders of the limbs and spine. If the shoulder joint is affected at the same time as the muscle tissue, chondroprotectors and massage products are used for external use.
Symptoms and diagnostic methods
The symptoms of the disease depend on the cause of myositis . However, the most striking sign of myositis is pain in the back, which sharply intensifies with physical activity. Sometimes, upon palpation of the affected muscle areas, dense cords or nodules are detected.
| Symptoms of acute infectious (purulent) myositis include: | Symptoms of chronic myositis include: |
|
|
Other signs of myositis include severe headaches, increased skin sensitivity, and low-grade body temperature . Sometimes there is a general malaise, accompanied by pain when turning and bending the body.
Diagnosing myositis is not easy, because... The most pronounced manifestation of symptoms occurs during the period of exacerbation of the disease. This is why doctors recommend making an appointment when you notice the first symptoms of the disease. You cannot postpone treatment until later, because... acute myositis can develop into chronic.
To make a diagnosis and draw up a treatment plan, the following examinations are prescribed::
- antibody tests;
- biochemical and general blood tests;
- electromyography;
- MRI;
- back muscle biopsy.
Types of myositis
In clinical practice, the following types of myositis are most often encountered:
- Cervical myositis. The most common option. The main manifestation is a dull pain in the neck muscles, most often one-sided. Sometimes it can radiate to the ear, back of the head, temple or interscapular area. Head movement is often limited due to pain.
- Lumbar myositis. The key symptom is a dull pain in the lower back that can radiate down the leg. It intensifies when bending the body, pressing on the muscles of the lower back.
- The most common cases are cervical and lumbar myositis. Photo: starast/Depositphotos
- Dermatomyositis. Manifested by weakness of the muscles of the shoulder and pelvic girdle, as well as the abs and neck. Because of this, patients have difficulty when trying to get up from a sitting or lying position, or climbing stairs. In severe forms of the disease, breathing and swallowing are impaired. In this case, the pain is less pronounced. Dermatomyositis also affects the skin, which is manifested by a heliotrope rash (red rashes on the eyelids, less often on the face, neck and torso) and Gottron's sign (pink or reddish scaly plaques and nodules on the extensor surfaces of the elbows and knees). Additionally, disturbances in the functioning of the lungs and heart may occur.
Myositis in pregnant women
Myositis in pregnant women
In some cases, the triggering factor for the development of myositis or the aggravation of its course is pregnancy. The most common triggers are:
- Effect of the hormone relaxin on skeletal muscles.
- A shift in the center of gravity and additional stress on the abdominal muscles and lower extremities.
- Exacerbation of previously existing pathologies in connection with pregnancy.
Clinical manifestations of myositis during pregnancy are no different from the symptoms of the disease in other categories of patients. However, during treatment, you need to choose the right medications, avoiding drugs with a teratogenic effect. Therefore, treatment tactics must be coordinated with the attending physician.
Treatment
Treatment of myositis should be carried out by an experienced doctor. In this case, you should not practice self-medication, because it is necessary to eliminate not only the pain, but also the cause of its occurrence.
Drugs
Did you know that...
Next fact
The following drugs can be used to treat myositis of the back muscles::
, such as Movalis, Ibuprofen, Ketorolac, Diclofenac. As a rule, they are prescribed in the form of injections. You can use these drugs for no longer than a week, because they can lead to the appearance of medicinal ulcers in the gastrointestinal tract.
Pay attention to the list of drugs used for myositis of the back muscles. Non-steroidal anti-inflammatory drugs- Medicines with angioprotective and venotonic effects . A good example of such drugs is L-lysine escinate, which reduces back pain, relieves inflammation and eliminates soft tissue swelling.
- Anthelmintics . Prescribed to patients with parasitic myositis.
- Antibiotics . They are used if myositis is caused by bacterial flora.
- Immunosuppressors, steroid hormones . Prescribed to people suffering from parasitic myositis.
Also, ointments are used to treat back muscles , which have analgesic and warming effects .
| Anti-inflammatory drugs |
| Anti-inflammatory gels and ointments can be used for most types of myositis, starting from the first day. They have anti-inflammatory, anti-edematous and analgesic effects. |
| Warming ointments |
| Warming ointments are prescribed if the disease is caused by prolonged static loads. They are used to warm up muscles and relieve spasms. |
Such ointments must be applied very carefully so as not to cause skin burns.
Surgery
Surgical treatment of the disease is practiced if the patient suffers from purulent myositis . In this case, the doctor opens the infectious focus, removes the purulent contents from it and applies a drainage bandage. In parallel, local and parenteral antibiotic therapy is carried out.
Exercises, exercise therapy, massage
a course of massage treatments may be prescribed . A massage performed by a qualified specialist can relieve muscle spasms, warm up muscles and improve blood circulation. It should be remembered that massage is contraindicated in patients with dermatomyositis and purulent myositis.
(therapeutic gymnastics) and yoga help well with myositis The latter includes physical exercises aimed at improving the body. Regular exercise helps develop stretching, strengthen muscles, and increase resistance to physical activity.
Treatment at home
In the acute course of the disease, patients must observe strict bed rest with limited physical activity . If there is a strong increase in body temperature, the patient is prescribed antipyretic drugs. The affected area of the back should be kept warm; For this you can use warm scarves, woolen headbands, etc.
You can also resort to using traditional medicine recipes:
- Cabbage leaf compress . Take two leaves of cabbage, sprinkle them with soda and soap them. Apply the sheets to the affected area, wrap your back with a woolen scarf or handkerchief. This compress has an analgesic effect.
- Treatment with potatoes . Boil three or four potatoes in their jackets, mash for better contact with the affected area. Through several layers of gauze, apply the resulting mass to the affected area. The compress is kept on the back until the potatoes have cooled. Then it is removed, and the compressed area is rubbed with vodka and wrapped in a woolen scarf. This procedure should be carried out for several days in a row.
- Compress with burdock leaves . Scald burdock leaves with boiling water, apply them to the sore spot and cover with a flannel diaper.
- Rubbing with bodyaga . Lightly melt 1 tsp. butter, mix with 1/4 tsp. tramps. Rub the prepared mixture into the affected area overnight and cover with a flannel diaper. This should be done no more than once a week. Otherwise, the skin may become irritated.
Most of the recipes listed above are suitable for the treatment of diseases caused by overexertion, hypothermia, and sometimes ARVI.
As for bacterial myositis, they cannot be heated to avoid the development of a purulent process. Therefore, before using any folk remedies, it is better to consult a doctor so as not to aggravate the situation with improper treatment.
Video: “Treatment of myositis”
Prevention
There are several preventive measures to prevent the development of myositis:
- avoid hypothermia and drafts, wear warm clothes in the cold season;
- warm up more often;
- give preference to healthy foods rich in vitamins;
- stop smoking and drinking alcohol;
- observe the rules of personal hygiene;
- lead a healthy lifestyle.
To avoid inflammation of the back muscles, it is necessary to prevent hypothermia of the body. To avoid the development of myositis, it is necessary to move regularly.
You cannot sit or stand in one position for a long time, even during so-called sedentary work.
Those who spend a lot of time driving or working on a computer should take short breaks every 1-2 hours (get up, do a light warm-up, turn your body and tilt your head).
It would be a good idea to diversify your diet by including fish, dairy products, vegetables and fruits.
These products contain vitamins C, A, E, potassium, iodine, vitamins B12 and D, polyunsaturated acids. They are necessary for the body to strengthen and maintain health, especially the muscular and skeletal systems.
Clinical and radiological manifestations of progressive fibrodysplasia ossificans in children
Fibrodysplasia ossificans progressiva (FOP), myositis ossificans progressiva (OPM), Munchmeyer's disease, disease of the “second skeleton” is a rare, congenital, disabling disease with an incidence of 1 in 2 million people.
Fibrodysplasia is characterized by congenital bone pathology and progressive heterotopic ossification of muscles, tendons, ligaments, and aponeuroses [1, 2]. There is no racial, gender or geographic predisposition. The disease most often occurs as a result of a spontaneous new mutation. Hereditary transmission is autosomal dominant, maternal mosaicism is possible.
In 2006, a predominantly same heterozygous mutation (c.617G>A; p.R206H) was discovered in the glycine and serine residue (GS) of the activin A receptor type 1 (ACVR1)/activin-like kinase 2 (ALK2) activation region ) receptor type 1 bone morphogenetic protein (BMP), regarded as a genetic cause of FOP. Seven additional mutations were subsequently identified in the GS region and ACVR1 kinase region in patients with “atypical” forms of the disease [3, 4].
The c.617G>A mutation results in the replacement of arginine by histidine at codon 206 (p.R206H). Structural homology modeling of proteins predicts that amino acid substitution leads to conformational changes in the receptor, which causes changes in its sensitivity and activity [3].
In FOP, active production of CMP-4 is expected above a threshold, which explains excessive ossification and ectopic bone formation postnatally [4].
Congenital phenotypes caused by FOP metamorphosis include a number of congenital deformities (deformations) and skeletal anomalies: deformed big toe (the main diagnostic sign of the disease), metaphyseal dysplasia, short phalanges, short thumbs, synostosis - symphalangism of the fingers, fusion of the surfaces of the cervical joints , fusion of costovertebral joints, proximal medial tibial osteochondromas, short wide necks of the humerus, sparse hair, deafness, etc. [1, 4, 5].
In the domestic literature, there are isolated studies on the development of FOP in children, mainly at school age [6–8].
In this report, we present the most typical clinical and radiological manifestations of FOP in 30 children aged 1.5 to 14 years, observed in the clinic of pediatric diseases of the First Moscow State Medical University named after. I. M. Sechenov in 1968–2010 and two cases with the identified FOP gene.
Children complained of the appearance of soft elastic formations on the head, which gradually spread down and became denser. The onset of the disease was often accompanied by malaise, low-grade fever, painful lesions, their gradual hardening, increasing general stiffness and contractures in the area of large joints. The speed of spread of the process ranged from 2–3 months to 3–5 years.
In some patients, spontaneous disappearance and/or recurrence of lesions was observed, in others the process steadily progressed. Gradually, the children seemed to be enveloped in a bone shell, a “second skeleton”, became inactive, had difficulty dressing independently, eating, changing position in space and eventually became disabled, dependent on the help of adults (Fig. 1, 2). Children of preschool age could lag behind their peers in development; older children were more withdrawn, but did well in school.
Sharp skeletal deformation, kyphoscoliosis, contractures in the joints, multiple ossifications on the back in an 8-year-old girl and a 14-year-old boy (own observations, 1970s)
Rice. 1. Photos of the first patients with FOP
About half of the children had a typical sign of the “classic” variant of FOP: pathology of the first toes: shortening, subluxations, symphalangism, monophalangism, etc.
Rice. 2. Contractures and extraskeletal bone formations on the back and anterior surface of the abdomen in two patients, 10 and 1.5 years old
Radiographs revealed extraskeletal, bone-density shadows (ossifications), both single and merging into large conglomerates. Typically, multiple linear shadows of bone density were detected, localized in the soft tissues of the extremities and trunk. Often the shadows intertwined with each other like the branches of a tree. The most common locations were the lateral surfaces of the chest and the inner surfaces of the shoulders, with the formation of synostoses between each other in the form of a “bridge” (Fig. 3). In young children, this localization was primary. Single or multiple exostoses were also common.
Rice. 3. Ossification on the lateral surfaces of the chest in the form of a bridge in a 2-year-old child
Basic laboratory parameters, including general and biochemical blood and urine tests (including enzymes and mineral metabolism indicators), levels of thyroid and parathyroid hormones, remained normal.
Treatment was carried out with corticosteroid hormones (prednisolone or methylprednisolone at a dose of 0.5–1 mg/kg per day) in short courses, non-steroidal anti-inflammatory drugs (NSAIDs), intravenous administration of a 5% solution of disodium salt of ethylenediaminetetraacetic acid (Na2 EDTA), 10% solution of Xidifon orally and/or locally by electrophoresis or ointment with Xidifon. In recent years, new generation bisphosphonates (disodium pamidronate or Aredia, Bonefos, Bonviva, etc.), antileukotriene drugs (montelukast) and mast cell blockers (cromolyn sodium) have been used.
We present interesting observations of two patients examined genetically in 2010.
Patient 1, aged 14, came to the clinic in June 2010.
The mother's pregnancy proceeded normally, but at the end swelling of the legs appeared, A/D - 150/100 mm Hg. Art., weight gain 10 kg. Due to the baby's head tilting, a cesarean section was performed (12-hour anhydrous period). Birth weight 3200 grams, length 53 cm, head circumference 36 cm. He grew and developed satisfactorily. He has been sitting since he was 6 months old, started walking at 10 months old, and his first tooth erupted at 4 months old. Weight at one year 11 kg, speech from 1 year 3 months. Breastfeeding for 2 months, then artificial, mild anemia was diagnosed.
For all vaccinations, except for the Mantoux reaction, a rise in temperature to 39–40 °C was noted. During DPT, the buttock became swollen (like “glass”).
Illnesses suffered before school - chicken pox, mononucleosis, later - ARVI.
At the age of two, a diagnosis of congenital valgus deformity of the big toes was made, and an operation was performed to straighten the subluxation of the first toe of the left foot (a pin was inserted).
At the age of 5 he was diagnosed with Perthes disease, an exostotic disease.
At the age of 6, an operation was performed to remove “growths” (exostoses) on both sides on the back surface of the knee joints. But a relapse occurred, and new lesions appeared in the front.
At the age of 9, due to a bruise (falling from a bicycle), my left leg began to bend poorly at the knee and I began to limp.
Bilateral sensorineural hearing loss was diagnosed at the age of 11.
At the age of 14 (April 2010), a lump appeared on the left side of the neck. During surgery, a strand of cartilaginous density was identified in the sternocleidomastoid muscle. The biopsy material was consulted at the Russian Cancer Research Center of the Academy of Medical Sciences of the Russian Federation: there is no evidence of a tumor.
Consulted at CITO in May 2010, exostoses and limitation of movements in the left sternocleidomastoid muscle were determined.
Ultrasound of the left sternocleidomastoid muscle (05/21/2010) - in its middle sections, an area of altered structure is identified, covering the entire thickness of the muscle over 5.2 cm with compaction, decreased echogenicity, and without a characteristic fibrous structure; higher and lower in the muscle tissue there are areas of hyperechoic muscle inclusions (postoperative changes against the background of specific myositis). On the right are similar inclusions.
Ultrasound of the anterior surface of the right thigh - at the level of the upper third - ossification (2.8 × 0.3 cm in thickness), in the soft tissues of the back on the right, at the level of the lower thoracic vertebrae - ossification, similar in structure.
Upon completion of the examination and face-to-face consultation at the Russian Cancer Research Center. N. N. Blokhin in May 2010, progressive myositis ossificans was suspected.
During a consultation with a geneticist, a diagnosis was made: “fibrodysplasia ossificans progressiva with an autosomal dominant type of inheritance in the pedigree “de novo.” The phenotype includes thickening of the muscles in the neck, back, and right thigh, from the age of 9 years, osteochondral exostoses in the upper third of the tibia and the lower third of the left thigh, congenital anomaly of the first fingers and toes (shortening, stiffness in the interphalangeal joints), shortening and expansion of the neck of the femur.
He was examined on an outpatient basis at the clinic of children's diseases (06/15–17/2010).
On examination, the boy is of good height and well-nourished (height 160 cm, weight 60 kg). Complains of difficulty turning the neck and bending the body forward. Feels awkwardness in the back and pelvis when walking and feeling, limps on the right leg.
The skin is clean with traces of tan. Shortening of the big toes and hands with subluxation on the legs - halux valgus (Fig. 4). There is a lump on the neck in the area of the left sternocleidomastoid muscle with a scar in the center. Turning left is difficult. Tilt the torso forward only to a horizontal level. On the right side of the front thigh there is a thickening of the muscle. On the back on the right, at the level of the 6th thoracic vertebra, a bone cord about 5–7 cm long is identified, without connection with the spine. Lymph nodes are not enlarged. From the lungs, heart, abdominal organs without pathology.
On the R-gram of the feet: on the right - hallux valgus deformity of the first toe, the main phalanx is significantly shortened, thickened, and displaced laterally (subluxation). On the left - deformation of the head of the metatarsal bone and the proximal phalanx of the first toe (after surgery). The joint space is unevenly narrowed (Fig. 4).
On the left – deformation of the head of the first metatarsal bone and the main phalanx of the first toe after surgery at the age of 2 years. On the right, shortening and subluxation of the main phalanx of the first toe (Halux valgus)
Rice. 4. Patient 14 years old. Shortening of big toes
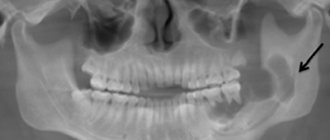
On an x-ray of the hip joints with coverage of 2/3 of the femurs, the heads of the femurs are flattened, the left one is displaced laterally. On the left, the roof of the acetabulum is sloping. Thickening of the cortex in the femurs. In the projection of the neck and upper half of the diaphysis of the femur on the left, shadows of bone density are determined in the soft tissues. On the right - single shadows in the projection of the femoral neck (
).
On radiographs of the hands, the relationship of the bones is not disturbed. Metaepiphyseal osteoporosis is noted. The metacarpal bones are shortened. On the left, the main phalanx of the first finger is shortened, hypoplasia of the epiphysis. The middle phalanges of the fifth fingers are curved.
EchoCG (06/17/2010). The dimensions of the heart cavities and myocardial thickness are within normal limits. Systolic and diastolic functions of the left ventricle are not impaired. Pulmonary artery pressure is normal. Along the anterior wall of the right ventricle, the minimum divergence of the pericardial layers in diastole is 1.3–1.5 mm. MARS: accessory basal chords and trabeculae in the cavity of the left ventricle. The Eustachian valve is lengthened.
Clinical diagnosis: “Fibrodysplasia ossificans progressive. Classic shape. Late stage. Congenital anomalies of the big toes: shortening and thickening of the main phalanges with subluxation (Halux valgus) and hands (shortening of the metacarpal bones and the main phalanx of the first finger on the left with hypoplasia of the epiphysis. Curvature of the middle phalanges of the fifth fingers). Osteochondral exostoses on the left at the level of the lower and upper thirds of the femur. Shortening and widening of the neck of the femur. Multiple extraskeletal bone formations (ossifications) in the thickness of the muscles of the back, hips, and neck.
MARS: accessory basal chords and trabecula in the cavity of the left ventricle, elongation of the eustachian valve. Bilateral sensorineural hearing loss.
In the DNA diagnostics laboratory: the Arg206 His mutation was found in the ACVR1 gene.”
Conclusion. The child was observed for a long time with diagnoses of congenital hallux valgus, exostotic disease, Perthes disease, suspected neck tumor with a biopsy of a changed area of the sternocleidomastoid muscle; received all vaccinations and vaccinations, despite a high fever for each administration of vaccines, did not comply with the necessary gentle motor regimen, was repeatedly injured, underwent numerous radiation studies, operations, and only after 14 years the diagnosis of FOP was verified and confirmed genetically.
Currently, he is recommended a gentle motor regimen, avoidance of all intramuscular injections, manipulations in the lower jaw, prevention of acute respiratory viral infections (Arbidol, sanitation of the nasal cavity - rinsing with sea water, drops - Marimer, vaccination during an influenza epidemic subcutaneously or intranasally), swimming in the pool with sea water or at sea, the use of prednisolone (2 mg/kg for 5–7 days) and bisphosphonates (Aredia) if new ossifications occur, registration of disability and dynamic observation in a specialized hospital.
The second patient has been under clinical supervision since 1 year 3 months.
History: mother, 27 years old, healthy, father, 39 years old, suffers from bronchial asthma and alcohol addiction. At the 18th week of pregnancy, the mother suffered from influenza and was subsequently hospitalized in the pregnancy pathology department due to disproportionate development of the head. Childbirth on time, physiological. The child's weight is 2530 g, length is 48 cm. Apgar score is 8–9. He screamed right away. Breastfeeding for 8 months, hypogalactia was noted. From early childhood, holding the head in a position on the stomach, at 3 months - massage due to hypertonicity of the neck muscles. Sits from 7 months, walks from 12 months, teeth from 5 months.
At the age of 5 months, he fell off the couch without consequences. Later, at 12 months, he fell again and hit his forehead. At the site of the injury there was swelling the size of a chicken egg. I received hydrocortisone and topical lotions with effect.
X-ray and tomography revealed a congenital anomaly of C1–C2 - deformation of the vertebral bodies in the form of platyspondylia, nonfusion at the level of the posterior sections (spina difida posterior), hypoplasia of the odontoid process of C2.
When echocardiography shows, the size of the heart chambers is higher than the age norm (high-nutrition boy: weight 15 kg at 1 year 2 months). Additional chord in the left ventricle.
At the initial examination, the child is in good physical development, has increased nutrition, is mobile, and sociable. There is “stiffness” and elevation in the shoulder girdle, tension and tightening of the neck muscles, limitation in turning the head and bending back. Movements in the joints of the limbs are not limited, there are no deformities. Squats, walks, runs freely. The skin and mucous membranes are clean. Teeth 10/8. The internal organs showed no pathology, hypospadias was detected.
There are diagnostic signs of the classic form of FOP - shortened big toes with subluxation (Fig. 6), as well as congenital pathology of the cervical vertebrae and hypospadias.
Rice. 6. Shortening and valgus deformity of the first toes in a 1.5-year-old patient
General blood and urine tests, biochemical blood tests are within normal limits.
Genetic examination revealed the presence of the Arg206His mutation in the ACVR1 gene, characteristic of the classic variant of FOP.
Clinical diagnosis: “Fibrodysplasia ossificans progressive. Classic shape. Early stage. Initial phase of the disease. Recurrent tumor-like formations on the head and neck. Cartilage-like elements in the form of longitudinal elastic cords (shadows on radiographs) in the soft tissues of the shoulder girdles and along the spine. Congenital bone abnormalities: shortening of the big toes. Underdevelopment of the odontoid process of the 2nd cervical vertebra. Platyspondyly and nonfusion of the posterior parts of the C1–C2 bodies. Hypospadias. Mutation Arg206 His in the ACVR1 gene."
The child is observed for a year. The disease does not progress. From time to time, elastic “tumors” appear on the head due to minor injuries, which quickly disappear when using ointment with Xydifon. A waiver has been given from all intramuscular vaccinations and vaccinations. A protective motor home regime is recommended. For falls and the formation of soft tumors on the head - ointment with Xidifon, NSAIDs orally, antileukotrienes. Dynamic observation in the clinic for therapy correction. Registration of childhood disability.
Thus, our observations indicate insufficient familiarity with FOP among doctors of various specialties - pediatricians, surgeons, orthopedists, which leads to lengthy verification of the diagnosis, unnecessary interventions and soft tissue injuries (surgeries, biopsies, intramuscular administration of drugs, vaccinations).
Summarizing the literature and our own data, the main factors for diagnosis should be considered to be the presence of congenital pathology of the big toes (often in combination with pathology of the fingers) and extraskeletal ossifications. In preschool children, as a rule, they appear on the neck, shoulder girdle and gradually spread downwards. In older children, ossification can appear in any area of soft tissue (muscles, tendons, etc.), more often as a result of injuries of any origin or against the background of influenza and ARVI. If FOP is suspected, a search for mutations in the ACVR1 gene is necessary.
Unfortunately, the prognosis of the disease is unsatisfactory. It is very important to follow all preventive measures to avoid any soft tissue injuries and to prevent acute respiratory viral infections and influenza, which can accelerate the progression of the disease and provoke pulmonary heart failure.
Currently, a community of scientists is actively developing and testing (in experiments and on animals) drugs that have the ability to block mutations in the ACVR1 gene, which will prevent or interrupt heterogeneous ossification and improve the condition of patients.
Literature
- Mc Kusick VA Heritable Disorders in Connective Tissue. St. Louis C. V. Mosby (pub) (4th ed.), 1972.
- Kaplan FS, Le Merrer M., Glaser DL, Pignolo RJ, Goldsby RE, Kitterman JA, Groppe J., Shore EM Fibrodysplasia ossificans progressiva // Best Pract Res Clin Rheumatol. 2008, 22: 191–205.
- Shore EM, Xu M., Feidman GJ et al. A recurrent mutation in the BMP type 1 receptor ACVR1 causes inherited and sporadic fibrodisplasia ossificans progressive // Nature Genetics. 2006, 38: 525–527.
- Koster B., Pauli RM, Reardon W., Zaidi S., Zasloff M., Morhart R., Mundios S., Groppe J., Shore EM Classic and atypical fibrodysplasia ossificans progressiva (FOP) phenotypes are caused by mutations in the bone morphogenetic protein (BMP) type I receptor ACVR1 // Hum Mutat. 2009, 303: 79–90.
- Kaplan FS, Glaser DL, Shore EM, Deimengian GK, Gupta R., Delai P., Morhart R., Smith R., Le Merrer M., Rogers JG, Connor M., Kitterman JA The phenotype of fibrodysplasia ossificans progressiva // Clin Rev Bone Miner Metab. 2005, 3–4: 183–188.
- Borisova T. S., Ryabova T. V., Ivanova K. V. On the issue of progressive dermatomyositis ossificans in children // Vestn. dermatol. and venerol. 1966, no. 12, 15–19.
- Lozhbanidze T. B., Antelava O. A., Nikishina I. P. et al. Progressive fibrodysplasia ossificans // Breast cancer. 2005, no. 8: 560–564.
- Ryabova T.V., Bayandina G.N., Utyusheva M.G., Geppe N.A. et al. Progressive polymyositis ossificans in children. In the book: Complex patient in the practice of a pediatric rheumatologist. M.: MIA. 2008. pp. 86–104.
T. V. Ryabova, Candidate of Medical Sciences N. A. Geppe , Doctor of Medical Sciences, Professor G. V. Mikhaleva I. G. Sermyagina First Moscow State Medical University named after. I. M. Sechenova, Medical Genetic Research Center of the Russian Academy of Medical Sciences, Moscow
Contact information for authors for correspondence