Forestier's disease, or ligamentosis ossificans, has been known for a long time, but only in 1950, after a detailed description of it by J. Forestier and J. Rots, it began to be called Forestier's disease , although the authors of the description themselves proposed calling it senile ankylosing hyperostosis of the spine. This is due to the fact that the disease is non-inflammatory, but slowly progressive in nature and is externally similar to spondylosis. But unlike the latter, it is not based on excess production of bone tissue, and at the same time, the concept of “ligamentosis” does not accurately reflect the pathomorphology, since it is not based on dystrophic damage to the longitudinal ligaments of the spine.
Since the 70s, the concept of Forestier's disease has not been limited only to local damage to the anterior longitudinal ligament of the spine, but has begun to be interpreted as a more generalized pathological process that also affects the peripheral parts of the skeleton. In this case, a gradual metaplasia of the elements of the connective tissue (ligaments) itself into cartilaginous tissue occurs, this process is accompanied by the phenomena of cystic degeneration, mainly in the places of fixation of tendons and ligaments to the bones with the deposition of calcium there and the subsequent formation of osteophytes, widely known as “spurs” (calcaneal “ spurs” osteophytes of the patellar ligament, osteophytes in places where muscles are attached to the iliac crests, etc.)
Introduction
Back pain is an interdisciplinary medical problem, however, such patients primarily turn to internists and general practitioners, who are responsible for timely differential diagnosis and prescription of a complex of therapy in cases where back pain is not a manifestation of a serious or life-threatening disease .
However, the prescribed therapy is not always successful, which may be due to an insufficient diagnostic search [1]. Thus, osteochondrosis or a disc herniation detected during magnetic resonance imaging (MRI) can mask diseases of an inflammatory, infectious, metabolic, or oncological nature. Assessing “threat symptoms,” or “red flags,” will allow the physician to identify the presence of a disease that requires a slightly different approach to therapeutic interventions.
This article presents a description of a clinical case - management of a comorbid patient with chronic pain syndrome.
Causes
The initiating factors for the development of hyperostosis are considered to be:
- neuroendocrine disorders;
- frequent intoxication;
- age-related changes in connective tissue;
- chronic infectious diseases.
Causes of Forestier's disease
Pain syndrome and ankylosis can be observed in people after 45-50 years of age, and most often such changes were observed in their parents. It is believed that genetic factors are of greatest importance in the development of pathology. Studies have shown that a third of patients had the following antigen: human leucocyte antigen - HLA B27 , the gene of which is responsible for bone formation.
Clinical observation
Patient E., 61 years old, complained of pain in the lumbar and thoracic spine, which appeared and intensified after physical activity, stiffness of the spine after physical activity or prolonged stay in one position, and a decrease in height by 7 cm over her life. The patient also noted pain in the joints of the lower extremities, mainly of a mechanical nature, and pain in the arch of the left foot.
From the anamnesis it is known that episodes of pain in the lower back have been bothering me since the age of 50. At the onset, the pain was acute, lasting up to 1–2 weeks. She was observed by a neurologist at her place of residence with a diagnosis of osteochondrosis; during exacerbations, short courses of therapy with nonsteroidal anti-inflammatory drugs (NSAIDs) and B vitamins were administered, which helped relieve back pain.
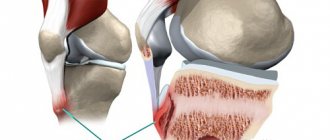
Over the past 8–10 years, I have been experiencing aching pain in the knee and hip joints, provoked by physical activity. Swelling of the knee joints was repeatedly noted, accompanied by morning stiffness for up to 30–60 minutes; symptoms of synovitis were relieved by taking NSAIDs. Damage to large joints of the lower extremities was regarded as osteoarthritis of the knee joints in combination with reactive synovitis.
The patient suffers from arterial hypertension and angina pectoris, for which she takes antihypertensive and antianginal drugs.
Due to pain in the spine and recurrent synovitis of the knee joints, she was sent for consultation to a rheumatologist with a referral diagnosis of “unspecified spondyloarthritis.”
During the examination, attention was drawn to excess body weight (body mass index 40.7 kg/m2), varicose veins of the lower extremities, pronounced thoracic kyphosis, limitation of movements in all parts of the spine (rotation in the cervical spine within 30° in both directions , distance “back of the head - wall” - 5 cm, chest excursion - 2 cm, Schober test - 2 cm). When assessing the local status - deformation in the area of the interphalangeal joints of the hands with the formation of Heberden and Bouchard's nodes, slight swelling of the knee joints, as well as in the area of the tarsal joints of the left foot, without signs of local hyperemia and hyperthermia.
Taking into account the presence of back pain, swelling of the knee joints and tarsal joints, further examination was carried out to exclude the disease from the group of spondyloarthritis. According to laboratory research methods: ESR - 33 mm/h (according to Westergren), C-reactive protein - 8 mg/l, rheumatoid factor - 2.0 U/l, HLA B27 - not detected. A general urine test and a biochemical blood test were unremarkable, with the exception of an increase in serum creatinine to 120 µmol/l.
An X-ray of the pelvic bones including the hip joints (Fig. 1) revealed subchondral osteosclerosis of the articular surfaces of the sacrum and ilium, narrowing of the joint spaces of the sacroiliac joints (SIJ), initial signs of bilateral coxarthrosis, ossification of the greater and lesser trochanters of the femurs, periostosis (enthesophytes ) tuberosities of the ischial bones, wings of the ilium.
Radiographs of the cervical (Fig. 2), thoracic (Fig. 3), lumbar (Fig. 4) spine revealed straightening of the cervical lordosis, pronounced subchondral sclerosis of the endplates of the vertebral bodies in the midthoracic region, a decrease in the height of the intervertebral discs, wedge-shaped deformation of the vertebral bodies in mid-thoracic region, massive marginal bone growths of the anterior corners of the bodies of the cervical, thoracic and lumbar vertebrae with massive calcification of the anterior longitudinal ligament in all parts of the spine along the entire length with coracoid growths in the cervical and mid-thoracic, lower thoracic regions, arthrosis of the facet joints. An ultrasound examination of the knee joints revealed only signs of suprapatellar bursitis on both sides.
Old age, evidence of back pain, the inability to remain in an upright position for a long time, and a decrease in height by 7 cm over a lifetime required caution regarding the exclusion of postmenopausal osteoporosis. According to a biochemical blood test: calcium - 2.19 mmol/l, phosphorus - 0.98 mmol/l, alkaline phosphatase - 219 U/l. The protein profile is unremarkable. X-ray densitometry of the central parts of the skeleton revealed a significant increase in mineral density (BMD) both in the lumbar spine (BMDL1-L4–1.908 g/cm2, T-criterion - 5.8 standard deviations) and in the proximal femur (BMD - 1.340 g/cm2, T-criterion - 2.6 standard deviations). Thus, no laboratory and instrumental data indicating osteoporosis were obtained.
Taking into account the absence of complaints of inflammatory pain in the spine, increased acute-phase blood parameters, arthritis of the knee joints, identified degenerative-dystrophic changes in the SIJ, ossification of the anterior longitudinal ligament of the spine in all parts of the spine, multiple peripheral hyperostoses, according to radiographic examination, it seemed most likely diagnosis of ankylosing diffuse idiopathic skeletal hyperostosis (Forestier disease).
In 1950, the French rheumatologist J. Forestier (in collaboration with J. Rotés-Querol) described in detail not only the radiological changes characteristic of ankylosing hyperostosis of the spine, but also the clinical picture of the disease, which is now called “Forestier disease”. A quarter of a century later, American radiologist D. Resnick published an article in which he showed that ankylosing hyperostosis of the spine is only one of the manifestations of systemic (generalized) ectopic ossification of ligaments, tendons and other connective tissue structures of the musculoskeletal system, and proposed a new term to designate this pathology - “diffuse idiopathic skeletal hyperostosis” [2]. D. Resnick and G. Niwayama in 1982 presented diagnostic signs of diffuse idiopathic skeletal hyperostosis, which were based on radiological data [3]. To make a diagnosis of this disease, all 3 signs must be present:
continuity of ossification of the anterior longitudinal ligament over at least 4 adjacent spinal segments;
absence (or weak severity) of signs of degenerative changes in the intervertebral discs, such as preservation of their height, absence of the vacuum phenomenon and marginal sclerosis of the vertebral bodies in those segments where the anterior longitudinal ligament of the spine is ossified;
absence of radiological signs of ankylosis of the facet joints and sacroiliitis.
Despite quite pronounced radiographic changes, complaints and objective examination data from the spine in diffuse idiopathic skeletal hyperostosis are nonspecific and are observed no more often than in elderly people of the same age, but without ossification of the anterior longitudinal ligament of the spine [4]. Thus, there is no direct relationship between the clinic and the x-ray picture.
Patients may complain of discomfort, stiffness, and, less commonly, pain in the thoracic spine, which intensifies in the morning after sleep, at the end of the working day, after physical activity, prolonged stay in one position, or in the cold. If the process spreads to the cervical and lumbar spine, these sensations may also be noted in these sections. The severity of pain ranges from mild to severe. Often, especially in old age, there may be no complaints [5].
Back fatigue, changes in posture, i.e. a rather poor clinical picture, allow one to suspect osteoporosis, which requires additional research. Therefore, if the disease seems asymptomatic, special attention should be paid to the significant thickening of the anterior and posterior longitudinal ligaments in the cervical spine. Severe ossification of the anterior longitudinal ligament can lead to compression of the esophagus, larynx, trachea and the development of dysphagia and dysphonia [6–8], paresthesia or a sensation of “lump in the throat” [9], and the posterior longitudinal ligament can lead to the threat of compression of the spinal cord with the development of myelopathy , paresis and paralysis [4].
In Forestier disease, ossification of the anterior longitudinal ligament always begins in the thoracic region (and in 99% of cases - in the middle and lower thoracic regions and on the right), as a result of which, to identify such changes, it is enough to perform an x-ray of the thoracic spine in a lateral projection. This will allow one to clearly see the rough ossification of predominantly the anterior longitudinal ligament. Later, the lumbar and cervical spine are involved in the process.
According to N.V. Bunchuk, X-ray changes in the spine in diffuse idiopathic skeletal hyperostosis are often interpreted as a picture of a “bamboo stick”, typical of ankylosing spondylitis [4]. Previously, it was mistakenly assumed that syndesmophytes in ankylosing spondylitis are formed due to ossification of the anterior longitudinal ligament. It has now been established that the formation of syndesmophyte in ankylosing spondylitis begins with inflammation of the attachment sites of the fibers of the fibrous ring of the intervertebral disc to the bodies of the above and underlying vertebrae, i.e., with enthesitis. Subsequently, chondroid metaplasia and ossification of the outer layers of the fibrous disc occurs, the front of which gradually spreads from the vertebral bodies to the middle of the disc. Thus, syndesmophytes typical for ankylosing spondylitis are located inside the disc and usually do not protrude beyond the lateral contours of the vertebrae (Fig. 5).
Ossification of the ligaments located in the posterior parts of the SIJ, as well as their capsule, can simulate partial ankylosis of these joints on a radiograph. Ossification of the SIJ ligaments in degenerative pathology (like arthrosis) up to ankylosis is observed only in the anterior sections.
The main differential diagnostic signs of diffuse idiopathic skeletal hyperostosis and ankylosing spondylitis are presented in Table 1.
In the treatment of spondyloalgia resulting from ankylosing hyperostosis of the spine, local thermal procedures and massage of the back muscles are usually effective. Regular exercise is helpful to maintain adequate mobility of the spine. The use of NSAIDs, effective for ankylosing spondylitis, in diffuse idiopathic skeletal hyperostosis leads to only a moderate reduction in pain [10]. Knowing this will allow you to avoid uncontrolled use of NSAIDs, given the likelihood of side effects. For the treatment of “peripheral” manifestations of the disease, the cause of which is reactive inflammation of structures undergoing calcification and ossification (enthesopathies, tendonitis, ligamentitis), according to N.V. Bunchuk, local methods of influence should be used, for example, injection of glucocorticoids under the control of ultrasound navigation [4].
Diet for Forestier hyperostosis
Hypocaloric diet
- Efficiency: 3-6 kg in 30 days
- Terms: 14-30 days
- Cost of products: 1500-1600 rubles. in Week
The fundamental factor in improving the condition of patients with hyperostosis is weight normalization, which can be achieved through a lifelong diet. Most often, a hypocaloric diet is prescribed, which can reduce the number of calories consumed, but at the same time provide the body with all the necessary substances and vitamins. It is recommended to add more to your diet:
- fresh vegetable and fruit salads;
- light soups;
- flour products made from whole grain or wholemeal flour;
- porridge;
- seafood;
- teas and compotes.
It is advisable to completely eliminate alcohol, flour, sweets, fried and fatty foods, as well as harmful foods such as smoked meats, canned food, semi-finished products, fast food, etc.
Symptoms and signs of spinal stenosis
Spinal stenosis at the level of the lumbar, thoracic or cervical spine develops quite slowly. This process can take several years of a person's life. The main symptoms are gradually increasing pain in a certain location. Moreover, discomfort and unpleasant sensations make themselves felt not only in the back, but also in the legs. At first, the disease manifests itself only when walking, and then the pain is present at rest.
Painful sensations do not have a clear localization. When walking, weakness in the legs increases. The person wants to sit down or even lie down. Bend your legs slightly or bend your torso slightly forward to relieve symptoms. Typical sensory disorders with lumbar spinal canal stenosis are numbness, decreased sensitivity in the legs, and a sensation of “pins and needles.”
The function of the pelvic organs can often be impaired. This manifests itself in a decrease in potency in men, defecation, retention, or vice versa - a sudden urge to urinate. With prolonged compression of the nerve roots of the spinal cord, you can notice that the lower limbs begin to gradually lose weight. Symptoms of cervical or thoracic spinal canal stenosis also manifest themselves in increasing spasticity in the legs.
Often this disease goes unnoticed. It is usually diagnosed at later stages of development. Especially when it comes to damage to the cervical spine. Pain may gradually appear in the neck. It can be either one-sided or two-sided. Unpleasant and painful sensations appear in the shoulder blades, shoulders, back of the head and arms. With certain movements of the neck, these pains begin to intensify. There is a feeling of “cottonness” in the legs. Cervical spinal canal stenosis is characterized by constipation and urinary retention.
If compression occurs at the level of 3-4 vertebrae, then respiratory dysfunction is noticeable. Spastic phenomena appear in both the legs and arms.
These are the main symptoms of spinal canal stenosis.
Are you experiencing symptoms of spinal stenosis?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Pathogenesis
The mechanism of initiation and further development of the disease is observed in a certain location. It should be understood that the free (reserve) space around the spinal cord and nerve roots should remain normal, since the vessels are located here. If it decreases or completely disappears, then circulatory disturbances occur both in the spinal cord and in the nerve roots. The circulation of cerebrospinal fluid is also impaired. Pathological narrowing of the reserve space is caused by the introduction of soft tissue, cartilage and bone structures.
The vascular bed begins to experience chronic stagnation due to compression of blood vessels and nerve elements. The spinal cord and roots experience “starvation,” that is, oxygen deficiency and lack of blood supply. As a result of this process, the function of the nerve elements is seriously impaired.
If there is a long-term disruption of the nutrition of the spinal cord and nerve roots, then scar tissue begins to form and grow, and the formation of adhesions is noticeable. Spinal stenosis of the cervical, thoracic, and lumbar regions often causes severe pain. A person develops vegetative, motor, sensory and trophic disorders.
Ligamentosis ossificans of the cervical spine
What is it - ligamentosis of the cervical spine from the point of view of vertebrology? This is the inability to freely move the head to its full physiological extent. With the development of ligamentosis ossificans of the cervical spine, a feeling of stiffness occurs at the initial stage. The patient cannot touch the sternum with his chin when bending his head forward. When you try to throw your head back, pain occurs.
Another clinical sign characteristic of spinal ligamentosis ossificans is a crunch in the neck. It can occur with any head movement. The subsequent development of pathology is characterized by the following symptoms:
- disruption of the blood supply to the brain due to incorrect position of the cerebral arteries and their compression;
- frequent headaches and decreased mental performance;
- decreased visual and hearing acuity due to pinching of the radicular and cranial nerves;
- attacks of sudden increase and decrease in blood pressure.
Signs of impaired innervation of the upper extremities may appear. This is expressed in muscle weakness, rapid fatigue, the appearance of lumbago and nagging pain. With a long course of cervical ligamentosis, signs of dystrophy of the muscle tissue of the upper extremities appear.
When to see a doctor
At the first symptoms of spinal stenosis in the lumbar, cervical or thoracic region, you should consult a specialist. JSC "Medicine" (clinic of academician Roitberg), located in the center of Moscow (near Mayakovskaya metro station, Belorusskaya metro station, Novoslobodskaya metro station, Tverskaya metro station, Chekhovskaya metro station), offers the opportunity undergo professional diagnostics and effective treatment. The staff consists of highly qualified doctors. Treatment of spinal canal stenosis l4 l5 and other levels is carried out by:
- vertebrologist
- neurologist.
Specialists prescribe the optimal treatment method, taking into account the degree of development of the disease and the individual characteristics of the patient.