Classification
In traumatology and orthopedics, there are five stages of Perthes disease:
- Termination of blood supply, formation of a focus of aseptic necrosis.
- Secondary depressed (impression) fracture of the femoral head in the destroyed area.
- Resorption of necrotic tissue, accompanied by shortening of the femoral neck.
- Overgrowth of connective tissue at the site of necrosis.
- Replacement of connective tissue with new bone, fracture healing.
The outcome of Perthes disease depends on the size and location of the area of necrosis. With a small lesion, full recovery is possible. With extensive destruction, the head breaks up into several separate fragments and after fusion can acquire an irregular shape: flatten, protrude beyond the edge of the articular cavity, etc. Violation of the normal anatomical relationships between the head and the acetabulum in such cases causes further aggravation of pathological changes: the formation of contractures , limited support and rapid development of severe coxarthrosis.
Osteochondropathy of the femoral head[edit | edit code]
Osteochondropathy of the femoral head
(Perthes-Legg-Calvé disease) was first described in 1909-1910. independently of each other by Waldenström in Sweden, Legg in the USA, Calvet in France and Perthes in Germany.
The pathology is considered common - among orthopedic patients it occurs in 0.17-1.9% of cases. Among diseases of the hip joint in childhood, osteochondropathy of the femoral head accounts for up to 25.3%.
Children are mainly affected between the ages of 4 and 12 years, but cases of the disease are known at earlier and later ages. Boys suffer more often than girls (4-5 times). The left hip joint is affected somewhat more often than the right. Bilateral localization of the process is observed in 7-10% of cases. Osteochondropathy of the femoral head is characterized by a long course (on average 2-4 years, and sometimes up to 5-6 years).
The disease occurs as a primary aseptic necrosis and occurs as a result of vascular disorders in the subchondral cancellous substance of the femoral head. Microtrauma, overload due to a constitutional predisposition, disruption of the normal process of ossification of the epiphysis of the femoral head at the age of 3-8 years (Perthes age), associated with its subcritical blood supply due to congenital underdevelopment of the local vascular network, are considered as etiological factors. A hereditary factor in the development of the disease, as well as the influence of foci of chronic infection, cannot be ruled out. In recent decades, an opinion has been expressed about the dysplastic nature of the pathology, according to which the cause of vascular disorders and necrosis of the head is the pathological orientation of the components of the hip joint.
Currently, with the help of modern research methods (radioisotope, capillaroscopic, thermometric, etc.), it has been established that disorders of arterial and venous circulation are present throughout the lower limb, and not just in the area of the hip joint. In addition, according to the modern understanding of the pathogenesis of Perthes disease, there is damage not only to the femoral head, but also to all elements of the hip joint - the acetabulum with articular cartilage, epiphyseal cartilage, femoral neck along with the entire metaphysis of the proximal femur, and joint capsule. That is why, according to many authors, there is every reason to call Perthes disease osteochondropathy of the hip joint.
Clinical picture[edit | edit code]
Osteochondropathy of the femoral head develops slowly, unnoticeably at first, which makes it difficult to diagnose the disease in the early stages of the development of the process. The first symptoms of the disease are pain and mild lameness. The pain is often paroxysmal, alternating with light intervals. Moreover, in the initial stage, in 75% of children, pain sensations are not only localized in the hip joint, but also radiate to the knee area (so-called referred pain). Fatigue occurs when walking, gentle lameness. Sometimes children complain of a feeling of tightness in the area of the greater trochanter, where pronounced dense limited swelling is detected.
Over time, there is a limitation of movements, especially abduction and internal rotation, and somewhat less often - a limitation of external rotation, flexion and adduction. Half of the children develop flexion and external rotation contracture.
Muscle atrophy is considered an early and persistent symptom. It is most noticeable in the area of the thigh muscles and buttocks. In some cases, against the background of lymphostasis, thickening of the skin and subcutaneous tissue, it may be subtle. Alexandrov's symptom, as a rule, is positive. Severe autonomic-vascular disorders may be present, which are more noticeable with a unilateral process. These include pallor and coldness of the foot, a decrease in the temperature of the extremity by 0.5-2.0? C, less pronounced capillary pulse in the area of the toes, wrinkled skin of the sole (washerwoman’s skin), slowdown of the biological and hydrophilic test, asymmetry of the sweating reaction according to Minor , circulatory disorders in the entire limb in comparison with a healthy one, detected by radioisotope research.
Shortening of the limb occurs, initially apparent (due to flexion-adduction contracture in the hip joint). With the progression of the process and flattening of the head of the femur, as well as in connection with its developing subluxation, a true shortening of the femur occurs by 2-3 cm. The greater trochanter on the affected side moves above the Roser-Nelaton line. Sometimes a positive Trendelenburg sign is determined. If treated incorrectly, the pathological process ends with deformation of the head and the development of osteoarthritis with persistent pain and dysfunction of the hip joint.
Sometimes the onset of Perthes disease is acute, with a rise in temperature and an inflammatory shift in the blood. However, in children with a normal course, subfebrile temperature is often observed, an increase in ESR to 23-34 mm/h, leukocytes - up to 109/l, lymphocytes - up to 45-54%.
X-ray examination[edit | edit code]
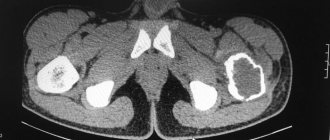
X-ray examination helps in making a diagnosis. For comparative analysis, X-rays of both hip joints are taken, as well as an X-ray in the Lauenstein position. The most complete information about the localization and extent of pathological changes in the femoral head is provided by CT and MRI of the hip joints. Radioisotope testing (scintigraphy) is highly effective in early diagnosis of the disease.
Changes in radiographs depend on the stage of the process.
In stage I (aseptic necrosis of the cancellous bone of the epiphysis and bone marrow) changes are absent or minor in the form of:
- osteoporosis of the bones forming the hip joint;
- tortuosity and unevenness of the cartilaginous epiphyseal plate;
- heterogeneity and spotting of the femoral neck;
- some expansion of the joint gap.
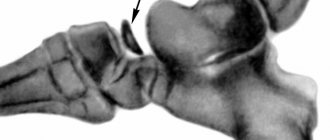
In stage II (impression fracture), the head of the femur loses its characteristic trabecular structure, and the femoral neck becomes more osteoporotic. The joint space clearly widens compared to a healthy hip joint. The epiphysis of the head becomes denser, sclerosed and deformed (due to continued load).
In stage III (fragmentation of the epiphysis), the joint space is still widened, the head is flattened and, as it were, divided into separate lumps or small-focal fragments of irregular shape. Usually 2 to 5 such fragments are identified, and sometimes more. The acetabulum becomes flattened.
In stage IV (reparation), the formation of new bone beams is determined, the epiphysis is completely replaced by newly formed bone with areas of clearing in the center.
In stage V (final), the structural restructuring and restoration of the shape of the femoral head and neck are completed. The joint space narrows and approaches normal in size. If the treatment was correct, the shape of the restored head differs slightly from spherical. Otherwise, a mushroom-shaped head with a shortened, widened neck is formed. In this case, the acetabulum does not completely cover the enlarged deformed head, which subsequently leads to the development of secondary coxarthrosis.
The greatest difficulties in radiological diagnosis are experienced at the initial (I) stage of the disease. That is why, to diagnose this stage, three groups of signs are distinguished: changes in soft tissues (capsule and muscles), projection changes in the bones of the pelvis and hip joint, direct signs of the disease.
Treatment[edit | edit code]
Treatment for Perthes disease must begin as early as possible to prevent the development of morphological changes and dysfunction of the joint.
Conservative treatment is based on early and long-term unloading of the limb, which allows maintaining the shape of the femoral head. Bed rest with cutaneous or skeletal traction on the affected leg and walking on crutches without putting any weight on the affected limb are prescribed. A special loop is used to suspend the leg, bent at the knee joint, by the lower third of the lower leg. Abduction splints with hinges at the level of the joints or orthopedic devices are used, which provide a significant reduction in excess pressure on the femoral head. Unloading should not exclude movement in the joint, therefore, to strengthen the muscles of the hip joint and the entire lower limb, exercise therapy, swimming in the pool, and massage are prescribed.
In order to improve reparative processes, drug treatment and physiotherapeutic procedures are prescribed. Depending on the stage of the disease, drugs are used that improve blood circulation [pentoxifylline (trental), nicotinic acid, nikoshpan] and stimulate reparative processes (methandienone, trifosadenine, B vitamins). Electrical procedures are used (UHF, electrophoresis, ultrasound, diathermy), which promote the resorption of necrotic tissue and the process of bone formation, as well as thermal procedures (paraffin, ozokerite, mud therapy, thermal baths), which improve blood flow in the affected area. The best conditions for conservative treatment are created in specialized sanatoriums. The average duration of conservative therapy is 2-3 years.
Surgical interventions for osteochondropathy of the femoral head can reduce the treatment time for the disease by 1.5 times and help reduce disability in this category of patients.
Admission to sports is prohibited.
Symptoms of Perthes disease
In the early stages, mild dull pain appears when walking. Usually the pain is localized in the hip joint, but in some cases pain may occur in the knee joint or throughout the leg. The child begins to limp slightly, falls on the sore leg or drags it. As a rule, during this period, clinical manifestations are so mild that parents do not even think of contacting an orthopedic doctor, and explain the symptoms of the disease as a bruise, increased stress, a consequence of an infectious disease, etc.
With further destruction of the head and the occurrence of an impression fracture, the pain sharply intensifies, and lameness becomes pronounced. The soft tissues in the joint area swell. A limitation of movements is detected: the patient cannot turn the leg outward, rotation, flexion and extension in the hip joint are limited. Walking is difficult. Autonomic disorders are noted in the distal parts of the diseased limb - the foot is cold, pale, and sweating is increased. Body temperature may rise to subfebrile levels. Subsequently, the pain becomes less intense, support on the leg is restored, but lameness and limited movement may persist. In some cases, shortening of the limb is detected. Over time, a clinical picture of progressive arthrosis appears.
Children and adolescents are characterized by certain diseases of the musculoskeletal system, which should be remembered when allowing them to play sports and organize them. This group of diseases includes osteochondropathy.
Osteochondropathy is a chronic bone disease that leads to frequent microfractures and fractures. The bone crossbars affected by the disease gradually lose their strength and begin to be damaged at the slightest load.
Osteochondropathy is observed most often in adolescence and childhood. It is a consequence of circulatory disorders, which occurs as a result of various causes: metabolic, congenital, traumatic, etc. A hereditary predisposition to the disease is likely, various bone tissue defects, changes in hormonal levels and metabolism are important. Also predisposing factors for the development of the disease are microtraumas, prolonged incorrect position of the spine or limb during sports and professional activities.
The most common osteochondropathy include Osgood-Schlatter disease (tibia tuberosity), Schinz disease (calcaneal tuberosity), Scheuermann-Mau disease (juvenile kyphosis).
At an appointment with an orthopedic traumatologist in our dispensary, osteochondropathy is detected in more than 3% of cases of examined young athletes.
Schlatter's disease is more often diagnosed in boys. There are complaints of swelling and pain in the area of the tibial tuberosity; patients can often hear that “... a new kneecap is growing”
Scheuermann-Mau disease or juvenile kyphosis is more common in young men during the growth period of 11-18 years. Clinical manifestations appear at the second stage of development of the disease and are characterized by the appearance of back pain, especially with prolonged walking and sitting, and severe deformation occurs.
But Schinz's disease, or osteochondropathy of the calcaneal tuberosity, is more common in girls aged 12-16 years. The disease begins with acute or constantly increasing pain in the area of the tubercle of the heel bone, and swelling is noted at the site of attachment of the Achilles tendon. Running, jumping, and playing sports become impossible.
As a rule, osteochondropathy is most often encountered in team sports: football, basketball, volleyball, athletics, etc.
Osteochondropathy is quite difficult to detect in the early stages of its development and therefore, over time, the disease can lead to unpleasant consequences. The weakened structures of the patient’s skeletal structure may begin to break down not only due to injuries, but also due to muscle cramps, muscle overstrain, and also under the influence of the gravity of one’s own body.
The diagnosis of osteochondropathy is established using x-ray examination. As a rule, X-rays of the affected area are taken in standard projections, and in some cases, computed tomography and MRI.
When osteochondropathy is detected, conservative treatment is generally indicated. Treatment is primarily aimed at unloading the affected part of the skeleton. They prescribe a gentle regimen, physical therapy, massage, physiotherapy, restorative therapy, spa treatment, orthopedic shoes, orthoses, taping. Physical education and sports with osteochondropathy are strictly contraindicated.
Residual effects of the disease - contractures and deformities - are treated conservatively, but in exceptional cases, with persistent and serious dysfunction, surgery is performed.
With timely detection of the disease and its treatment, it is quite easy to prevent the occurrence of severe complications - contractures and deformities.
Despite the fact that most osteochondropathy has a favorable outcome, self-healing is rare. Therefore, the sooner you contact a specialist and begin treatment, the sooner recovery will occur. Complex therapy of osteochondropathy significantly reduces the duration of the stages of the pathological process and avoids complications. And it is also very important to have constant monitoring by a traumatologist-orthopedist at least once every 3 months.
Our dispensary has created all the necessary conditions for the treatment of this group of diseases.
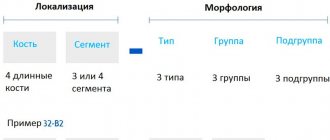
Diagnostics
The most important study that is decisive in making a diagnosis of Perthes disease is radiography of the hip joint. If this disease is suspected, not only images in standard projections are taken, but also radiographs in the Lauenstein projection. The X-ray picture depends on the stage and severity of the disease. There are various radiological classifications, the most popular of which are the Catterall and Salter-Thomson classifications.
Catterall classification: