Perthes disease (full name Legg-Calvé-Perthes disease) is a fairly common pathology of the hip joint in children aged 3 to 15 years and is an aseptic necrosis of the femoral head and impaired blood supply to the cartilage tissue of the joint. Necrosis is aseptic and not associated with infection. Perthes disease is more common in boys, but in girls the disease is more severe. As a rule, one joint is affected, but in a certain percentage of cases there is bilateral joint damage.
The causes of this disease are not fully understood, but certain mechanisms of pathogenesis have become clear in recent years.
First of all, a certain genetic determination is required (that is, the presence of myelodysplasia). Myelodysplasia means underdevelopment of the spinal cord. As a rule, myelodyspasia is moderate and manifests itself only as a disturbance in the development of innervation of the hip joint, which is manifested by various orthopedic diseases (including Perthes disease). Underdevelopment of innervation is accompanied by underdevelopment of the vascular network, which is responsible for the blood supply to the joint and a decrease in vascular tone. But for the development of aseptic necrosis, a complete cessation of blood flow to the head of the hip bone is necessary. Such conditions occur when a joint becomes inflamed or a joint is injured.
The inflammatory process in the joint can be reactive in nature to previous infections (acute respiratory infections, ENT diseases). As a rule, the symptoms of Perthes disease are associated with minor injuries or viral diseases, which is noted by the parents of patients. As a result of a combination of genetic underdevelopment of innervation and blood supply and in the presence of provoking factors (trauma or infection), the circulation of the femoral head is impaired, which leads to partial or complete necrosis of the area with impaired blood supply. First, necrosis occurs in the ossification core of the femoral head, then a compression fracture is possible in this part of the femur and then resorption of necrotic tissue and replacement of bone tissue with connective tissue, which in turn calcifies after some time. All this leads to shortening of the femoral neck, disruption of the structure of the acetabulum, and these anatomical disorders lead to disruption of the biomechanics of movements in the hip joint.
Causes
The disease is still being studied, since the main cause of its manifestation has not yet been identified.
There are such theories of the occurrence of pathology:
- Traumatic - the root cause is damage to the head of the hip bone and its displacement.
- Hormonal – the main trigger is hormonal imbalance at certain periods in children’s lives
- Infectious - a reaction to damage to the joint by viruses, infectious agents and the corresponding response of the immune system to their vital activity.
- Metabolic - a failure in the metabolism of various minerals (calcium, phosphorus), which take an active part in the formation of bone tissue.
- Genetic predisposition.
It is noted that the following groups of children are at risk:
- with weakened immunity;
- after suffering from rickets;
- with congenital myelodysplasia of the lumbar spinal cord;
- with frequent diseases of infectious and allergic origin;
- with nutritional deficiency.
The combination of several causes of the development of Perthes disease and the child being at risk increases the likelihood of developing the pathology.
Symptoms
Symptoms vary depending on the stage of the pathology. There is a connection between progression after infections and inflammation in the throat and nasopharynx - sinusitis, sore throat.
Characteristic features:
- Pain when moving. Dull, not severe pain in the area of the affected joint, knee, or along the entire length of the limb.
- Changes in gait - lameness, dragging of the leg or falling on it.
- Swelling in the joint area.
- Motor limitation - in the affected area it is difficult to turn, bend, or turn outward.
- Low-grade fever.
- Autonomic symptoms: severe sweating of the foot, pallor of the skin, wrinkling, decreased pulse in the foot and toes, and hypothermia.
- Weakness of the gluteal muscles.
A laboratory blood test reveals an increase in lymphocytes and an increase in ESR with leukocytosis.
Severe pain and other signs that cause severe discomfort indicate deformation of the head of the bone and a fracture, and therefore require immediate treatment.
Classification
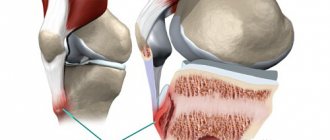
Aseptic necrosis, which is the mechanism of development of Perthes disease, consists of necrosis of bone tissue in the upper hemisphere of the head of the bone.
Necrotic process of non-infectious etiology - the lesion develops without pus and microorganisms.
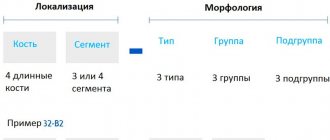
The current classification has been in use since 1928. There are 5 stages of the disease:
- Stage 1 - primary subchondral-aseptic necrosis of the bone marrow and spongy substance of the femoral head;
- Stage 2 - impression syndrome - secondary depressed fracture of the head;
- Stage 3 - fragmentation - resorption of dead areas, accompanied by shortening of the bone;;
- Stage 4 - proliferation of connective tissue;
- Stage 5 - restoration of the structure of the spongy substance.
Gradual changes lead to deformation, shortening of the bone with the development of lameness and motor limitations. If left untreated, the disease leads to disability.
What are the outcomes of the disease?
The main circumstances for determining the outcome of Perthes disease are the age of children in the initial period of the pathological process, the location and size of necrosis in the head of the femur, timely diagnosis and correct implementation of therapeutic measures.
The prognosis of the disease is no less influenced by the conscientiousness of the child and his parents following the recommendations for further treatment given by the orthopedic doctor. The main ones are: eliminating excess physical activity (jumping, running, lifting weights, etc.) and reducing excess body weight throughout subsequent life. In this regard, the child is not allowed to participate in almost all types of sports and physical education at school - at best, he is allowed to attend a special group without passing the standards. The physical activity of such children should be manifested in the form of some acceptable types of exercise - swimming in the pool, therapeutic exercises to maintain a normal range of motion in the joint, exercise on an exercise bike and a sports bike. Otherwise, developing physical inactivity almost always leads to excess weight, which becomes a serious additional problem for the patient.
Diagnostics
To determine the disease and prescribe therapy, you must seek help from an orthopedist.
The main method that allows you to obtain complete information about the stage of the lesion and the location of the damage is an x-ray of the hip joint in different projections.
Diagnosis of stage 1 is difficult; at stages 2-5, changes are obvious. To complement the clinical picture at the initial stage of development of the disease, an ultrasound of the joint or CT may be needed.
Are there any measures to prevent this disease?
There are currently no specific measures to prevent Perthes disease.
The appearance of pain in the hip, knee or hip joints, as well as gait disturbances, is a signal for parents to consult an orthopedic doctor, especially if the above symptoms appeared after suffering “colds” and injuries.
Regular preventive examinations in preschool institutions and schools can detect early symptoms of Perthes disease, which will allow starting complex treatment with a higher probability of a favorable outcome.
Treatment
Initially, Legg-Calvé-Perthes disease requires removal of the load from the leg - cuff traction, movement on crutches, as well as the active use of physiotherapeutic techniques.
More serious manifestations require surgery with further rehabilitation.
Conservative treatment
Non-surgical treatment is aimed at reducing the load on the affected joint and stimulating the resorption of dying tissue, as well as maintaining muscle tone during the period of forced motor limitation.
Apply:
- plastering;
- application of immobilizing orthopedic structures;
- medicinal and non-medicinal methods of activating blood flow in the affected area.
The peculiarity of therapy is its duration - at least a year of treatment in a hospital setting.
Active load can be prescribed from the 4th stage, and from the 5th stage exercises are introduced to restore the functioning of the joint and muscles.
Surgical intervention
Surgery is rarely required - in especially advanced cases.
There are 3 types of surgical interventions:
- Joint endoprosthetics.
- Tunneling. It consists of drilling several channels in the femoral neck, which are subsequently filled with granulation tissue, densely permeated with blood vessels. This improves blood flow and eliminates the problem.
- Elimination of mutual pressure between joint surfaces (arising from cramps) and muscle contractures.
The rehabilitation period after surgery or treatment without surgery is aimed at preventing infection, tissue necrosis, and restoring the functioning of the joint and muscles.
Physiotherapy
At various stages of restoration of bone structure, joint and muscle function, various types of physiotherapeutic techniques are used.
Shown:
- Shock wave therapy effectively restores blood flow, relieves pain, and improves metabolic processes.
- Diathermy - heating with high-frequency currents is used to relieve pain, improve blood and lymph circulation, and activate the work of macrophages and leukocytes.
- Electrophoresis (with calcium and phosphorus) - improves blood flow and metabolic processes.
- Thermal procedures are aimed at increasing blood flow.
- Diet food. The diet includes foods rich in fat-soluble vitamins, protein, and calcium.
Loading the joint after treatment is possible only during a control ultrasound, CT scan or radiography.
Surgery
If conservative treatment is not effective, then surgery is indicated.
Perthes disease is treated surgically in severe cases: with early, complete and bilateral necrosis. Children are selected for surgery when they reach 6–7 years of age and have symptoms of developing subluxation of the femoral head. With this disease, plastic surgery is performed, aimed at both correcting the head and “turning” the acetabulum.
If the operation is performed according to indications, then with a favorable outcome and timely intervention, the patient is able to move without the help of crutches, a cane, and even without lameness (or with a slight limp). But physical activities like running and carrying heavy objects are prohibited.
Forecasts
Perthes disease is not life-threatening, but advanced stages of joint damage can cause disability. The development of deforming arthrosis, lameness, and limited mobility is likely.
With complete relief from the disease, some restrictions remain for life, namely, you need to avoid:
- overloads;
- heavy physical work;
- sprains in the joint area;
- traumatic sports.
If discomfort in the joint area recurs, you should consult an orthopedist.
Legg-Calvé-Perthes disease can be successfully treated without the use of complex surgical operations if it is detected at the initial stage of development. To do this, it is necessary to promptly respond to symptoms - lameness, complaints of pain, and also be sure to consult with an orthopedist after injuries suffered by the child.
X-RAY SIGNS.
During osteochondropathy of the femoral head in children, five successively developing stages are distinguished, each of which has its own pathomorphological and radiological features. I, the initial stage, is characterized by necrosis of the spongy bone of the epiphysis and bone marrow, stage II - an impression fracture, stage III - fragmentation of the epiphysis, stage IV - reparation, stage V - final restoration of the bone.
The greatest difficulties in radiological diagnosis are experienced precisely at the initial (I) stage of the disease. Therefore, to diagnose this stage, three groups of signs are distinguished: changes in soft tissues (capsule and muscles), projection changes in the bones of the pelvis and hip joint, direct signs of the disease.
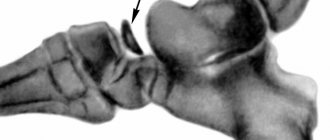
On a soft radiograph of both hip joints in stage I, it is possible to detect an increase in intensity and expansion of the shadow of the capsule of the hip joint due to synovitis, expansion of the intermuscular spaces between the medius, gluteus minimus and iliopsoas muscles due to edema [Shitova N.K., 1961; Kapitanaki A.L., 1964]. Direct signs of stage I of the disease are osteoporosis of the bones of the hip joint and the corresponding half of the pelvis, especially the upper-outer part of the glenoid cavity [Gerasimova N. A., 1925]; heterogeneity, spotting of the paraepiphyseal zone of the femoral neck, simulating its expansion; tortuosity and unevenness of the cartilaginous epiphyseal plate, the presence of a marginal pattern and protrusion on the adjacent surfaces of the epiphysis of the head and neck in the area of the epiphyseal zone, flattening of the spherical contour of the epiphysis, the appearance of a convex outer contour of the femoral neck, an increase in the height of the joint space [Reinberg S. A., 1925 ; Priezzheva V.N., 1971].
Projection signs can be identified only if the patient is positioned correctly and symmetrically and x-rays of the pelvic bones and both joints are taken. These signs include different projections of the wing of the ilium, the obturator foramen on the right and left [Petukhova L.I., Volkova V.V.], expansion of the figure of the tear [Halkier, 1956].
X-rays have been proposed as early indirect signs of Perthes disease: displacement of the sacrum to the healthy side; changing the shape of the Shenton line from arcuate to square; increase in the epiphyseal-diaphyseal angle of Alsberg; an increase in the angle formed by the intersection of the femoral axis with the plane of entry into the glenoid cavity; decreasing the angle formed by the intersection of the Hilgenreiner line with the continuation of the epiphyseal cartilage line; displacement of the apex and increase in the angle formed by the intersection of the sagittal axis of the pelvis with the continuation of the plane of entry into the glenoid cavity [Abalmasova E. A., Kryukova I. N., 1979].
At the end of stage I, in the paraepiphyseal zone of the femoral neck, foci of destruction may be detected, in the area of which racemose lucencies later form; the neck shortens and becomes wider. The first stage lasts up to 6 months [Reinberg S.A., 1964].
In stage II - an impression fracture, in which necrotic bone beams, losing strength under the influence of static and dynamic loads, break and are impressed. X-ray at this stage, the shadow of the epiphysis becomes denser; its structure is lost, its height decreases, and the joint space expands accordingly. From this stage, diagnosing the disease is not difficult. Stage II lasts from 3 to 6-8 months.
In stage III of epiphysis fragmentation, in which revascularization of the epiphysis occurs from the periosteum of the femoral neck, cartilage of the head, and cancellous bone of the neck. Connective tissue grows deep into the necrotic bone of the epiphysis, and along with it, blood vessels. They divide the head into separate fragments, and cysts of various sizes form in the neck. This stage lasts from 1 to 1.5 years. At the same time, the resorption of the old bone is followed by the process of formation of new bone, which occurs more actively from the inside, and in the center of the head dense sequester-like shadows can persist for a long time.
In stage IV - reparations; with it, sequestration-like shadows disappear, the epiphysis is completely replaced by newly formed bone with areas of clearing in the center.
In stage V - the final stage, corresponding to the restoration of the shape of the head and structure characteristic of a mature bone. Head restoration can be twofold; with favorable outcomes, the height of the epiphysis of the head approaches its height in a normal joint. However, with the most ideal outcomes, the height of the head is restored to no more than 85%. With less favorable outcomes, the head has a mushroom shape; it is 30-70% not overlapped by the depression, in 75% of patients the depression is flattened and extended upward [Redulescu A., 1967]. The neck of the femur shortens and widens. In these cases, hip subluxation may occur.
In children with subluxation, conditions are created for the early development of deforming arthrosis, which V. M. Ermolaev and P. D. Mitskevich observed already in patients aged 15-20 years. M. D. Krylova (1971) described a localized form of osteochondropathy in the upper-outer quadrant of the head, and A. L. Limin, N. I. Khvisyuk (1970) observed a subcapital form in 19% - with a more favorable course.