Currently, such a pathology as osteochondropathy of the tibial tuberosity is quite common. Young people suffer from this disease. The disease is often diagnosed in individuals involved in a certain type of activity (football players, basketball players, track and field athletes and other athletes).
The second name for this pathology is Schlatter's disease. The disease is dangerous because it has a chronic, progressive course and, in the absence of proper therapy, can cause a person to lose their ability to work. What are the etiology, clinical picture and treatment of Schlatter's disease?
Features of Schlatter's disease
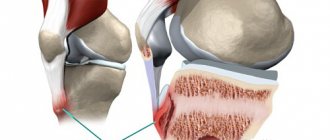
Osteochondropathy of the tibial tuberosity is a disease of non-inflammatory origin, characterized by destruction (necrosis) of the bone tuberosity. The tibia forms the skeleton of the lower limbs. It is located in the lower leg area (between the knee and foot). This is one of the largest bones in the human body. Next to it is the fibula. The tuberosity is located at the top of the anterior edge of the bone. The quadriceps femoris muscle is attached to it. This disease has been known for about a century and is part of a special group of diseases called osteochondropathy.
Schlatter's disease is most often diagnosed in people aged 10 to 18 years. Boys suffer from this disease much more often than girls.
This is due to a more active lifestyle of people, an addiction to sports games, which often leads to bone trauma.
The process most often affects both bones. Unilateral lesions are less common. Often there is a combined lesion of the tibia and spine. The disease occurs in a chronic form. At the same time, the percentage of benign course of the disease is high.
Etiological factors
Osteochondropathy of the tibial tuberosity most often develops against the background of trauma. The latter may be due to:
- playing sports (football, volleyball, hockey, basketball);
- choreography classes;
- regular blows to the shin area.
The risk group includes children and adolescents who actively engage in sports. About 20% of all teenage athletes suffer from this pathology. Schlatter's disease can also occur in children who do not lead a similar lifestyle. The cause in this case may be domestic injuries.
In recent years, girls have increasingly become interested in gymnastics, figure skating, choreography, and fitness. Therefore, they are also at risk.
Permanent injuries lead to disruption of the nutrition of the tuberosity of the tibia. This is facilitated by contraction of the quadriceps muscle. All tubular bones have so-called growth zones. Children experience active growth of bones that are not yet fully developed. Regular injuries can cause avulsion fractures. These fractures soon heal, and a bone growth forms in this place. Over time, this causes characteristic symptoms in children and adolescents.
Clinical manifestations
Schlatter's disease has rather sparse symptoms. In the early stages, patients may not present any complaints. The most common symptom is pain. It has the following features:
- localized in the area of the tibia closer to the knee;
- weak at first, but gradually intensifies;
- becomes more intense with active movements;
- worsens when kneeling;
- subsides at rest;
- often combined with swelling in the knee area.
Objective signs of the disease include severe tissue swelling at the site of the lesion and bone tenderness on palpation. The disease is non-infectious, so general symptoms such as increased body temperature are not observed. Unlike a fracture or bruise, there is no pronounced hyperemia at the site of bone damage. In some patients, the disease progresses in waves. In this case, an exacerbation in the form of pain can be provoked by intense physical activity (jumping, running, squats).
Department of Traumatology and Orthopedics
article in PDF format
QUOTE LINK:
A. V. ANTONOV, V. E. VOLOVIK
KGBOU DPO "Institute for Advanced Training of Health Care Specialists" MHHC, Khabarovsk
Information about the authors:
Antonov Alexander Vadimovich – Postgraduate student of the Department of Traumatology and Orthopedics of the KGBOU DPO "Institute for Advanced Training of Healthcare Specialists" of the Ministry of Health of the Khabarovsk Territory, e-mail
Volovik Valery Evgenievich - Head of the Department of Traumatology and Orthopedics of the KGBOU DPO "Institute for Advanced Training of Healthcare Specialists" of the Ministry of Health of the Khabarovsk Territory, Honored Worker of Science and Education, Honored Health Worker of the Russian Federation, Doctor of Medical Sciences, Prof., Corresponding Member. RAE, e-mail
Aseptic necrosis of the femoral head is a common multifactorial, polyetiological disease, representing a complex medical and social problem, affecting people of working age and accounting for 1.2–4.7% of all degenerative-dystrophic diseases of the musculoskeletal system according to various authors. The lack of timely diagnosis and the inappropriateness of conservative treatment when citizens present late lead to their disability, and subsequently to a complete joint replacement. Endoprosthetics as a method of choice for surgical treatment is associated with both long-term rehabilitation of patients and the risks of developing instability of components, and with the onset of 2021, many economic aspects. This problem remains relevant and requires further study, improvement of methods of conservative and surgical treatment in order to achieve stable long-term remission, and possibly complete recovery of the patient.
Key words: aseptic; ANGBK; necrosis; idiopathic necrosis; necrosis of the femoral head.
Aseptic necrosis of the femoral head (AFH) is a severe chronic common pathology, which accounts for 1.2–4.7% of all degenerative diseases of the musculoskeletal system according to various authors. The problem of early diagnosis due to the absence of obvious symptoms during the onset of the disease, the similarity of clinical signs with other pathological conditions and the rapid development of the disease lead to characteristic degenerative processes. Changes in the usual rhythm of life and the inability to receive medical care due to the lack of effective treatment methods sooner or later lead to persistent impairment and disability of patients [1].
The risk group for the development of this pathology is predominantly the male population aged 20–50 years, exposed to various harmful factors (alcoholism, smoking, use of corticosteroids, radiation), as well as a number of serious diseases: sickle cell anemia, coagulopathies, vasculitis, hyperlipidemia, decompression sickness, Gaucher disease, bleeding disorders, chronic liver and kidney diseases, etc., requiring the use of aggressive treatment methods such as hemodialysis, chemotherapy, etc.
The nature of the changes occurring in the femoral head is not fully understood, but the traumatic etiology of the disease remains undoubted. According to S. Delaunay, depending on the severity of the injury, 10–50% of patients with various injuries to the hip joint (HJ) develop aseptic necrosis in the immediate or long term [2]. A number of foreign authors [3, 4], having studied modern methods of surgical treatment for fractures and their long-term consequences, believe that the development of ANFH is influenced by the patient’s age and delay of surgery, but not by the method of treatment [5]. Along with these conclusions, there are non-traumatic theories of origin associated with insufficient blood supply (including atypical variants of the development of the topographic-anatomical picture of the branches of the deep femoral artery) [6], increased intraosseous pressure, functional inferiority of the hip joint, the toxic effect of drugs (protein tyrosine kinase inhibitors, hormone-induced ANFH) [7, 8], with metabolic (lipid metabolism disorders) [9], neurogenic disorders [10]. Considering the many theories of the origin of the pathological process, today there are no suitable experimental models to find the cause of the disease [11].
The study of the pathogenesis of the disease over the last century has not yielded fruitful results of the same type, making this problem, from the point of view of many specialists, unsolvable. For example, M.G. Proves (1938) determined that the arteries of the femoral head do not end blindly, suggesting the possibility of a thromboembolic mechanism. Gratsiansky (1955) believed that ANFH is a secondary pathology that occurs after a fracture of bone beams, representing the trigger mechanism as microtraumatization or overload of the joint, activating the processes of fatigue. In this case, pathological impulses directed from the lesion to the cerebral cortex contribute to the formation of a reverse signal, causing vasospasm, stagnation of blood and lymph, metabolic disorders, accumulation of decay products, changes in the physicochemical properties of bone tissue, and subsequently destruction of bone beams with difficulty in local blood circulation and, accordingly, necrosis. For the first time, A.L. spoke about the possible participation of the parasympathetic nervous system in the development of the pathological process. Gimmelfarb, who argued that pathological impulses from the focus contribute to the development of reflex vascular spasm, disrupting the blood supply. Focusing on the presence of vascular disorders, a number of researchers examined separately the arterial, venous and mixed components (L. Solomon, N.F. Moroz); at the same time, Leriche, believing that the root cause may be a disorder of lipid metabolism, refers to the need to revise the ischemic theory of pathogenesis.
The historically recognized foundations of ischemic disorders were also confirmed and expanded by O.P. Bolshakov, who determined the possibility of atypical variants of development of the topographic-anatomical picture of the branches of the deep femoral artery in the form of an increase in the angle of departure of the circumflex arteries or the complete absence of the medial circumflex artery.
Over the past 10 years, thanks to many foreign experimental models, the number of assumptions regarding the pathogenesis of the disease has increased significantly. Changes occurring in the head of the femur are primarily due to local disturbances in blood flow, decreased perfusion due to the anatomical features of the feeding vessels [12], which leads to the development of ischemic phenomena. As a result of changes in blood supply and the hydrodynamic influence of elastic deformations, redistribution disorders, perimedullary venous congestion, disruption of tissue metabolism, increased osteoclastic resorption, thinning and sponging of the compact substance, an increase in bone marrow spaces and the development of necrosis occur. Lipid disorders, including those resulting from increased levels of steroids, play an important role in joint nutrition and are most likely one of the causes of vascular disorders [13]. H. Kantor believes that approximately 45% of patients have a triad of metabolic disorders - lipid metabolism disorders, liver diseases and chronic alcoholism. But despite the harmony of the alcohol-induced theory, according to D. Orlic, the incidence of pathology in alcohol abusers is 3.9%. This indicates the participation of other processes in pathogenesis, in addition to lipid metabolism disorders [2]. The study of the genetic aspects of the pathology has shown the important role of oxidative damage to the DNA of hematopoietic bone marrow cells [14], polymorphism of various genes and endothelial synthase [15, 16].
Proponents of molecular studies conclude that there is a causal relationship with osteoprotegerin synthesis [17], fibroblast growth factors [18], leptin levels in the bone marrow [19] and proteoglycan loss, compared with inflammatory changes in arthritis [20], considering that ANFH may be preceded by an inflammatory response [21]. In any case, an important pathomorphological link in the development of the disease is: violation of the conditions of transcapillary exchange, inhibition of mineralization, degeneration of the red bone marrow. A pathological type of blood circulation is formed with the development of ischemia, and subsequently the death of bone cells with the formation of a zone of bone tissue decay [11] and microcrystallization of cartilage [23]. If the load-bearing capacity of the necrotic bone decreases, the subsequent disruption of the distribution of contact stress leads to the collapse of the femoral head and its complete destruction [24].
Among all theories of pathogenesis, the concept of deposition of calcium-containing crystals in articular cartilage and para-articular tissues occupies a special position. In this case, certain types of crystals are detected, such as calcium pyrophosphate, hydroxyapatite, tri-octacalcium phosphates. This phenomenon is called “microcrystalline stress” and, according to A.I. Dubikov, occurs in all patients with aseptic necrosis, which indicates the need to revise existing theories of pathogenesis [23].
Changes that occur in the head of the femur are usually accompanied by changes in the color, structure and shape of the surface; tuberosity or roughness of the cartilaginous cover appears, while hyaline cartilage remains of dense consistency, gray, less often brown, with additional inclusions. Dystrophic changes in cartilage and bone tissue are accompanied by thinning of the cortical layer, expansion of the interbeam spaces, angiomatosis, as well as cicatricial degeneration of the joint capsule. There are signs of fatty degeneration of the bone marrow, fibrous tissue, resorption, necrobiosis, lymphoid-plasmacytic and histocytic infiltration of the stroma, and in some cases, an inflammatory reaction.
Classifications of this disease are quite rare and are represented mainly by the x-ray picture and symptoms, not counting the form of the process. There are 4 types of ANFH: peripheral, which consists of localizing the pathological focus in the outer part of the femoral head under the articular cartilage; central, with the formation of a necrosis zone in the center of the femoral head; segmental, in the form of a small area of necrosis in the shape of a cone in the upper or upper-outer part; complete defeat.
The expansion of radiological diagnostic capabilities in recent years has made it possible to make a significant step forward in the examination of patients in the early stages of the development of ANFH. The sensitivity and specificity of magnetic resonance imaging (MRI) [25] in the differential diagnosis of this disease is 98%, making it possible to identify the pathological process at the initial stage (grade I) [26], computed tomography (grade II), and radiographic methods (grade III). –IV century) according to the international classifications Ficat and Arlet [27]. Pre-radiological stages of the pathological process, not diagnosed by MRI, include circulatory disorders, manifested only on angiography and scintigraphy [28] in the form of increased intraosseous pressure and histological changes. V. Packialakshmi, conducting a series of experimental studies, isolated a number of low-molecular proteins specific for ANGBC, suggesting their use as biomarkers [29].
The effectiveness of conservative treatment depends primarily on the location and severity of the process, as well as on the age and general health of the patient, the outcome of which correlates with the stage of the disease and should take an integrated approach. Conservative therapy traditionally includes: compliance with the optimal orthopedic regimen (with dosed load on the affected joint), therapeutic exercises, medication and physical therapy (extracorporeal shock wave therapy, electropulse therapy, hyperbaric oxygenation) [30]. Pharmacotherapy includes the use of bisphosphonates [31], low molecular weight heparins [32], ossein-hydroxyapatite complex, vasodilators, antiplatelet agents, calcium and vitamin D preparations, using intra-articular administration of dimexide, chondroitin, perfluoran [33], hydrogen-enriched saline [34] , platelet-rich plasma [35] – with positive dynamics at stages I–II. Some authors note positive dynamics with oral use of imatinib with hydroxyurea [36]. J. Pak, isolating stem cells from adipose tissue and using platelet-rich plasma together with hyaluronic acid, reports complete recovery of a patient with stage I necrosis of the femoral head [37]. Despite the many proposed methods, treatment of ANFH is possible only in the early stages of the disease, in which, as a rule, standard research methods do not provide timely recognition of the pathological condition.
Existing surgical methods are used with varying success rates, and no one method can be considered the best. Classic surgical treatment options, such as tunnelization [38], have been repeatedly revised and are used together with transplantation of bone marrow mesenchymal cells [39], recombinant human bone morphogenetic proteins [40], replacement of the tunnel with an autograft of the ilium [41], fibula [ 42], a vascularized graft on a nutrient pedicle [43], and a porous tantalum rod. Multiple tunneling techniques have been developed to maximize revascularization of the femoral head [44], with replacement with calcium phosphate composite, decalcified bone matrix, bone cement, biphasic ceramic implants, and even in combination with partial synovectomy of the hip joint. But despite this, M. Olsen, according to his latest research, came to the conclusion that complete removal of the tantalum rod after tunneling poses a problem due to the destruction of the metal structure during use, and osteoplastic operations using fibula autograft are complicated in 23% cases (T. Fang), which does not exclude a similar percentage of complications with other methods of autotransplantation.
Various corrective osteotomies proposed recently: detorsion-variation, anterior rotation, transtrochanteric, valgus (Y. Nakashima), double subtrochanteric transverse osteotomies [45], changing the point of maximum load on the femoral head, do not allow to restore the configuration of the articular surface in case of advanced destructive process, creating technical difficulties for subsequent arthroplasty [46]. The above methods, used individually, provide only minor dynamics, making it possible to delay radical surgery for a short time.
In modern literature, there has recently been increasing evidence of positive results of arthroscopic methods of treating ANFH in the early stages, using arthroscopic curettage of the necrotic area with the introduction of autogenous bone cylinders. Endoscopic navigation, which allows for detailed assessment of the accuracy and effectiveness of surgical procedures, is comparable in its effectiveness only to decompressive treatment methods [47] and will have a number of advantages in the future [48]. One of the approaches to the possibilities of revascularization of the femoral head is considered by R.M. Rasulov, which consists of incomplete ligature occlusion of the femoral artery [49]. Total hip arthroplasty is the main method of modern treatment, which is used everywhere in stages III–IV of the disease and has relatively good medium-term clinical results, but is not recommended due to the high risk of revision interventions [22].
Effective prevention of aseptic necrosis of the femoral head is a difficult task, including early clinical examination of risk groups, a strict sequence of patient management with the earliest diagnosis of the corresponding stage of the process, compliance with the complexity of rehabilitation measures, and is practically not found in modern literature.
Aseptic necrosis of the femoral head is a common multifactorial polyetiological disease, affecting mainly men of working age, the initial link of the pathogenesis of which has not been precisely studied. Diagnosis of ANFH presents significant difficulties due to both the late presentation of patients for medical help and the lack of clear diagnostic signs, expressed only by bone marrow edema in the initial stage of the pathological process on MRI. Traditional conservative treatment is not effective enough and provides only short-term improvement only in the early stages of the process due to the use of drugs with low or unproven effectiveness, which make it possible to delay complete joint replacement only for a short period of time. Surgical methods, as a rule, are traumatic and require long-term rehabilitation, without providing stable long-term remission, and endoprosthetics are associated with high risks of component instability. This problem is relevant and requires further study of individual factors for each patient, health status, concomitant diseases (endocrine and immunological status) and the level of activity of patients, improving methods of conservative and surgical treatment in order to achieve stable long-term remission, and possibly complete recovery of the patient .
Conflict of interest
The authors of this article have confirmed that there are no conflicts of interest to disclose.
Bibliography
1. Bashkova, I.B. Multiple non-traumatic osteonecrosis of large joints in a young man, provoked by short-term treatment with glucocorticoids / I.B. Bashkova, I.V. Madyanov // Russian. honey. magazine Rheumatology. – 2021. – No. 2. – P. 125–128.
Bashkova, IB Mnozhestvennye netravmaticheskie osteonekrozy krupnykh sustavov u molodogo cheloveka, sprovotsirovannye neprodolzhitel'nym lecheniem glyukokortikoidami / IB Bashkova, IV Madyanov // Rus. med. zhurn. Revmatologiya. – 2021. – No. 2. – P. 125–128.
2. Blishch, O.Yu. Pain in the hip joint: modern ideas about the capabilities and role of various methods of radiation diagnostics in determining the causes of pain // Radiation diagnostics and therapy. – 2014. – No. 2 (5). – pp. 37–44.
Blishch, O. Yu. Bol' v tazobedrennom sustave: sovremennye predstavleniya o vozmozhnostyakh i roli razlichnykh metodov luchevoi diagnostiki v opredelenii prichin bolevogo sindroma // Luchevaya diagnostika i terapiya. – 2014. – No. 2 (5). – P. 37–44.
3. Bolshakov, O.P. The importance of functional and anatomical factors in the choice of treatment method for adult patients with aseptic necrosis of the femoral head and children with Legg-Calvé-Perthes disease / O.P. Bolshakov, N.V. Kornilov, R.M. Rasulov // Vestn. traumatology and orthopedics named after. N.N. Priorova. – 2007. – No. 2. – P. 27–31.
Bol'shakov, OP Znachenie funktsional'nykh i anatomicheskikh faktorov v vybore metoda lecheniya vzroslykh bol'nykh s asepticheskim nekrozom golovki bedrennoi kosti i detei s bolezn'yu Legga–Kal've–Pertesa / OP Bol'shakov, NV Kornilov, RM Rasulov // Vestn. travmatologii i ortopedii im. NN Priorova. – 2007. – No. 2. – P. 27–31.
4. Volkov, E.E. Microcirculation parameters in the area of the hip joints in healthy volunteers: orig. research / E.E. Volkov, A.M. Vasilenko, S.E. Mezhov // Thrombosis, hemostasis and rheology. – 2021. – No. 2 (66): June. – pp. 43–46.
Volkov, EE Parametry mikrotsirkulyatsii v zone tazobedrennykh sustavov u zdorovykh dobrovol'tsev : orig. issledovaniya / EE Volkov, AM Vasilenko, SE Mezhov // Tromboz, gemostaz i reologiya. – 2021. – No. 2 (66). – P. 43–46.
5. Guryev, V.V. Revascularization of the hip joint in persons with post-traumatic coxarthrosis of the initial stage / V.V. Guryev, V.I. Zorya, E.D. Sklyanchuk // Moscow. surgeon. magazine – 2011. – No. 2 (18). – pp. 44–48.
Gur'ev, VV Revaskulyarizatsiya tazobedrennogo sustava u lits s posttravmaticheskim koksartrozom nachal'noi stadii / VV Gur'ev, VI Zorya, ED Sklyanchuk // Mosk. khirurg. zhurn. –
2011. – No. 2 (18). – P. 44–48. 6. Dubikov, A.I. The phenomenon of microcrystallization of cartilage during
coxarthrosis and aseptic necrosis of the femoral head (original research) / A.I. Dubikov, M.A. Kabalyk, T.Yu. Petrikeeva // Scientific and practical rheumatology. – 2012. – No. 54 (5). – pp. 37–41.
Dubikov, AI Fenomen mikrokristallizatsii khryashcha pri koksartroze i asepticheskom nekroze golovki bedrennoi kosti (orig. issledovaniya) / AI Dubikov, MA Kabalyk, T.Yu. Petrikeeva // Nauchno-prakticheskaya revmatologiya. – 2012. – No. 54 (5). – P. 37–41.
7. Kovalenko, A.N. Etiology and pathogenesis of aseptic necrosis of the femoral head / A.N. Kovalenko, I.F. Akhtyamov // Genius of orthopedics. – 2010. – No. 2. – P. 138–144.
Kovalenko, AN Etiologiya i patogenez asepticheskogo nekroza golovki bedrennoi kosti / AN Kovalenko, IF Akhtyamov // Genii ortopedii. – 2010. – No. 2. – S. 138–144.
8. Mustafin, R.N. Aseptic necrosis of the femoral head // Lecheb. case. – 2015. – No. 4. – P. 7–20.
Musta n, RN Asepticheskii nekroz golovki bedrennoi kosti // Lecheb. business – 2015. – No. 4. – P. 7–20.
9. Prokhorenko, V.M. The use of perftoran in the conservative treatment of the initial stages of aseptic necrosis of the femoral head / V.M. Prokhorenko, A.G. Shusharin, M.P. Half // Vestn. traumatology and orthopedics named after. N.N. Priorova. – 2015. – No. 4. – P. 26–31.
Prokhorenko, VM Ispol'zovanie per orana pri konservativnom lechenii nachal'nykh stadii asepticheskogo nekroza golovki bedrennoi kosti / VM Prokhorenko, AG Shusharin, MP Polovinka // Vestn. travmatologii i ortopedii im. NN Priorova. – 2015. – No. 4. – P. 26–31.
10. Rasulov, R.M. The influence of redistribution of arterial blood flow in the femoral vessels on the restitution of the femoral head during its necrosis in an experiment // Clinical Medicine. Medical academic journal. – 2004. – T. 4, No. 4. – P. 89–95.
Rasulov, R.M. Meditsinskii akademicheskii zhurnal. – 2004. – T. 4, No. 4. – P. 89–95.
11. Rempel, D.P. Possibility of methods for radiological diagnosis of damage to a symmetrical joint with diagnosed aseptic necrosis of the femur / D.P. Rempel, A.V. Bryukhanov, Yu.M. Farmhand // RADIOLOGY – practice. – 2013. – No. 6. – P. 24–32.
Rempel', DP Vozmozhnost' metodov luchevoi diagnostiki porazheniya simmetrichnogo sustava pri diagnostirovannom asepticheskom nekroze bedrennoi kosti / DP Rempel', AV Bryukhanov, Yu.M. Batrak // RADIOLOGIYa – praktika. – 2013. – No. 6. – P. 24–32.
12. Fedorov, V.G. Medium-term monitoring of the results of bone grafting in aseptic necrosis of the femoral head // International. butt magazine and foundation. research. – 2015. – No. 11. – P. 689–693.
Fedorov, VG Srednesrochnyi monitoring rezul'tatov kostnoi plastiki pri asepticheskom nekroze golovki bedrennoi kosti // Mezhdunar. zhurnal priklad. i fundament. researched. – 2015. – No. 11. – P. 689–693.
13. Shusharin, A.G. Aseptic necrosis of the femoral head: options for conservative treatment and results / A.G. Shusharin, M.P. Half, V.M. Prokhorenko // Scienti c reviews. Fundamental research. – 2014. – No. 10. – P. 428–435.
Shusharin, AG Asepticheskii nekroz golovki bedrennoi kosti: varianty konservativnogo lecheniya i rezul'taty / AG Shusharin, MP Polovinka, VM Prokhorenko // Scienti c reviews. Fundamental research. – 2014. – No. 10. – P. 428–435.
14. A comparative study on the measurement of femoral head necrosis lesions using ultra-thin layer slicing and computer aided identification / SD Li, SB Xu, C. Xu et al. // Zhongguo Gu Shang. – 2021. – No. 29 (2) : Feb. – P. 131–135.
15.Arthroscopic management and platelet-rich plasma therapy for avascular necrosis of the hip / J. Guadilla, N. Fiz, I. Andia, M. Sánchez // Knee Surgery, Sports Traumatology, Arthroscopy: o c. J. of e ESSKA. – 2012. – Vol. 20 (2) : Feb. – P. 393–398. DOI: 10.1007/s00167-011-1587-9
16. Avascular necrosis of femoral head as the initial manifestation of CML. Informa Healthcare / S. Kumar, D. Bansal, M. Prakash, P. Sharma // J. of Pediatric, Hematology/Oncology. – 2014. – No. 31 (6): Sep. – P. 568–573. DOI: 10.3109/08880018.2013.831961
17. Bergh, C. Increased risk of revision in patients with non-traumatic femoral head necrosis // Acta Orthopaedica. – 2014. – Vol. 85 (1): Feb. – P. 11–17. DOI: 10.3109/17453674.2013.874927
18. Chang, T. Treatment of early avascular necrosis of femoral head by core decompression combined with autologous bone marrow mesenchymal stem cells transplantation // Chinese J. of Reparative and Reconstructive Surgery. – 2010. – Vol. 24 (6): Jun. – P. 739–743.
19. Daniel, M. Contact stress in hips with osteonecrosis of the femoral head / M. Daniel, S. Herman, D. Dolinar // Clinical Orthopedics and Related Research. – 2006. – Vol. 447 : Jun. – P. 92–99. DOI: 10.1097/01.blo.0000203472.88926.c8
20. Deleanu, B. Avascular necrosis of the femoral head at 2 years a er pertrochanteric fracture surgery / B. Deleanu, R. Prejbeanu, D. Vermesan et al. // Annals of Medicine and Surgery (Lond). – 2015. – No. 5: Dec. – P. 106–109. DOI: 10.1016/j.amsu.2015.12.053
21. Downregulation of basic broblast growth factor is associated with femoral head necrosis in broilers / PE Li, ZL Zhou, CY Shi, JF Hou // Poultry Science J. – 2015. – Vol. 94 (5) : May. – P. 1052–1059. DOI: 10.3382/ps/pev071
22. Drilling decompression for femoral head necrosis at collapse stage / M. Wei, ZG Wang, YJ Liu, ZL Li // Zhongguo Gu Shang. – 2015. – No. 28 (6): Jun. – P. 562–566.
23. E ects of leucocyte and platelet-rich plasma on osteogenic di erentiation of bone marrow mesenchymal stem cells in treating avascular necrosis of femoral head in rabbits / J. Fang, Z. Yin, W. Wang et al. // Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. – 2015. – No. 29 (2): Feb. – P. 227–233. https://dx.doi. org/10.1155/2016/9458396
24.E ects of osteoprotegerin, RANK and RANKL on bone destruction and collapse in avascular necrosis femoral head / MY Xiong, LO Liu, SQ Liu SQ et al. // Amer. J. of Transl. Research. – 2021. – No. 8 (7): Jul. 15. – P. 3133–3140. PMCID: PMC4969450
25. F-18 uoride positron emission tomography/computed tomography in the diagnosis of avascular necrosis of the femoral head: Comparison with magnetic resonance imaging / S. Gayana, A. Bhattacharya, RK Sen et al. //Ind. J. of Nuclear Medicine. – 2016. – No. 31 (1) : Jan.-Mar. – P. 3–8. DOI: 10.4103/09723919.172337
26. Femoral Head Avascular Necrosis Is Not Caused by Arthroscopic Posterolateral Femoroplasty / R. Stoner, F. Strambi, I. Bohacek, T. Smoljanovic // Orthopedics. – 2021. – No. 39 (6): Nov. 1. – P. 330. DOI: 10.3928/01477447-20161020-01
27. Govaers, K. Endoscopically assisted core decompression in avascular necrosis of the femoral head // Acta Orthopaedica Belgica. – 2009. – Vol. 75 (5) : Oct. – P. 631–636.
28. Huang, SL Hydrogen-rich saline attenuates steroid-associated femoral head necrosis through inhibition of oxidative stress in a rabbit model / SL Huang, J. Jiao, HW Yan // Experimental and eraprutic Medicine. – 2021. – No. 11(1) : Jan. – P. 177–182. DOI: 10.3892/etm.2015.2883
29. Kawai, K. Steroid – induced accumulation of lipid in the osteocytes of the rabbit femoral head. A histochemical and electron microscopic study / K. Kawai, A. Tamaki, K. Hirohata. // Surg. – 1985. – Vol. 67-A, No. 5. – P. 755–763.
30.Li, D. Alterations of sympathetic nerve bers in avascular necrosis of the femoral head // Intern. J. of Clinical and Experimental Pathology. – 2015. – Vol. 8 (9): Sep, 01. – P. 10947–10952. PMCID: PMC4637627
31.Li, Z. BCB1 gene polymorphisms and glucocorticoid-induced avascular necrosis of the femoral head susceptibility: a meta-analysis // Intern. Medical J. of Experimental and Clinical Research. – 2014. – Vol. 20 : Dec. 29. – P. 2811–2816. DOI: 10.12659/MSM.891286
32.Liu, T. Correlation between local microenvironment leptin expression and avascular necrosis of the femoral head // Chinese J. of Reparative and Reconstructive Surgery. – 2012. – Vol. 26 (11): Nov. – P. 13–19.
33. Mohanty, SP Management of non-traumatic avascular necrosis of the femoral head-a comparative analysis of the outcome of multiple small diameter drilling and core decompression with bular gra ing // Musculoskeletal Surgery. – 2021. – Oct. DOI: 10.1007/s12306-016-0431-2
34. Packialakshmi, B. Poultry Femoral Head Separation and Necrosis: A Review // Avian Diseases. – 2015. – Vol. 59 (3): Ser. – P. 349–354. DOI: 10.1637/11082-040715-Review.1
35. Pak, J. Complete resolution of avascular necrosis of the human femoral head treated with adipose tissue-derived stem cells and platelet-rich plasma // e J. of Intern. Med. Research. – 2014. – Vol. 42 (6): Dec. – P. 1353–1362. DOI: 10.1177/0300060514546940
36. Pan, ZX E ect of recombinant human bone morphogenetic protein 2/poly-lactide-co-glycolic acid (rhBMP-2/PLGA) with core decompression on repair of rabbit femoral head necrosis // Asian Paci c J. of Tropical Medicine . – 2014. – Vol. 7 (11): Nov. –
P. 895–899. DOI: 10.1016/S1995-7645(14)60156-5 37. Proteomic Changes in the Plasma of Broiler Chickens with Femoral Head Necrosis / B. Packialakshmi, R. Liyanage, Jr. Lay JO et al. // Biomarker Insights. – 2021. – No. 11 : Apr. 27. –
P. 55–62. DOI: 10.4137/BMI.S38291 38. Roles of oxidative DNA damage of bone marrow hematopoietic
cells in steroid-induced avascular necrosis of the femoral head / ZQ Zhao, R. Bai, WL Liu et al. // Genetics and Molecular Research. – 2021. – No. 15 (1) : Mar. 24. DOI: 10.4238/gmr.15017706
39. S3 guideline. Part 2: Non-Traumatic Avascular Femoral Head Necrosis in Adults – Untreated Course and Conservative Treatment / A. Roth, J. Beckmann, U. Smolenski et al. // Zeitschri fur Orthopadie und Unfallchirurgie. – 2015. – No. 153(5) : Oct. – P. 488–497. DOI: 10.1055/s-0035-1545903
40. Should thorough Debridement be used in Fibular Allogra with impaction bone grafting to treat Femoral Head Necrosis: a biomechanical evaluation / G. Zhou, Y. Zhang, L. Zeng et al. // BMC Musculoskeletal Disorders. – 2015. – No. 16 : Jun 10. – P. 140. DOI: 10.1186/s12891-015-0593-3
41. Steroid-induced ischemic bone necrosis of femoral head: Treatment strategies. Professional Medical Publications / B. Wu, Z. Dong, S. Li, H. Song // Pakistan J. Med. Sciences. – 2015. – No. 31(2) : Mar.-Apr. – P. 471–476.
42. Total hip arthroplasty a er failed curved intertrochanteric varus osteotomy for avascular necrosis of the femoral head / Y. Takegami, D. Komatsu, T. Seki et al. ; Nagoya University School Of Medicine // Nagoya J. Med. Science. – 2021. – No. 78 (1): Feb. – P. 89–97. PMCID: PMC4767517
43. Treatment of bilateral avascular necrosis of femoral head by free vascularized bula gra ing with unilateral bula as donor. Publisher: China NLM ID: 9425194 Publication Model: Print Cited Medium: Print ISSN: 1002-1892 / X. Liu, J. Sheng, C. Zhang et al. // Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. – 2011. – No. 25 (6): Jun. – P. 641–645.
44. Tribological changes in the articular cartilage of a human femoral head with avascular necrosis / EM Seo, SK Shrestha, CT Duong // Biointerphases. – 2015. – No. 10 (20): Jun. 29. – P. 021004. DOI: 10.1116/1.4919020
45. Wang, L. Study on e ect of sensory neuropeptide in steroid-induced avascular necrosis of femoral head // Chinese J. of Reparative and Reconstructive Surgery. – 2010. – Vol. 24 (9): Sep. – P. 1078–1081.
46. Wang, T. Analysis of risk factors for femoral head necrosis a er internal xation in femoral neck fractures // Orthopedics. – 2014. – Vol. 37 (12) : Dec. – P. e1117–23. DOI: 10.3928/0147744720141124-60
47.Wang, W. Study on the relationship between osteoporosis and mRNA expressions of vascular endothelial growth factor and bone morphogenetic protein 2 in nontraumatic avascular necrosis of femoral head // Chinese J. of Reparative and Reconstructive Surgery. – 2010. – Vol. 24 (9) : Sep. – P. 1072–1077. DOI: 10.3928/01477447-20141124-60
48. Yassin, MA Dasatinib Induced Avascular Necrosis of Femoral Head in Adult Patient with Chronic Myeloid Leukemia // Blood Disorders. – 2015. – Vol. 8:Jul. 23. – P. 19–23. DOI: 10.4137/CMBD.S24628
49. Zhang, GP Correlation between polymorphism of endothelial nitric oxide synthase and avascular necrosis of femoral head // Intern. J. of Clinical and Experimental Medicine. – 2015. – Vol. 8 (10) : Oct. 15. – P. 18849–18854. PMCID: PMC4694406
ASEPTIC NECROSIS OF THE FEMORAL HEAD (LITERATURE REVIEW)
AV ANTONOV, VE VOLOVIK
Postgraduate Institute for Public Health Workers, Khabarovsk
Degenerative diseases of a hip joint (for example aseptic necrosis of the femoral head), one of modern problems of the orthopedics which appears at working-age people. ANFH as multifactory pathology with not clear etiology and the beginning, high risk of development at young age and lack of e cient methods of treatment requires the greatest attention and studying.
Key words: necrosis, ANFH; aseptic necrosis; femoral necrosis; avascular necrosis.
Diagnostic measures
Osteochondropathy of the tibial tuberosity can be identified on the basis of an external examination, characteristic clinical data and an x-ray picture. Patient information is of no small importance in making a diagnosis. The age and gender of the patient are taken into account. Diagnostics includes:
- collection of anamnesis of illness and life;
- examination of the lower extremities;
- palpation;
- X-ray examination;
- Ultrasound;
- general and biochemical blood tests.
Currently, computed tomography and magnetic resonance imaging are increasingly used to detect pathology of the skeletal system. It is advisable to carry out instrumental research several times to determine whether the disease is progressing or not. In the early stages, X-ray examination can reveal flattening of the soft cover in the area of the tuberosity of the bone, as well as signs of enlargement of the knee joint bursa. As the disease progresses, a spine-like protrusion is identified.
As for laboratory testing, it is necessary to exclude other diseases, in particular rheumatoid arthritis. With the latter, rheumatoid factor is detected in the blood. As a diagnostic test, a PCR study can be performed to exclude joint damage of infectious origin. The doctor must carry out a differential diagnosis with other diseases (osteomyelitis, rheumatoid arthritis, fractures, bone tuberculosis, syphilis).
Diagnostics
The examination plan includes the following imaging methods:
- X-ray of the hip joint. To increase the information content, special layouts according to Launstein are used. Initially, the images show areas of reduced density under the subchondral bone, giving the superficial parts of the head an “eggshell” appearance. Then the deformation of the head and the necrotic focus become visible in the form of a dense shadow surrounded by a lighter rim. The outcome visualizes changes characteristic of deforming arthrosis.
- CT scan of the hip joint . At the initial stage, when performing a diagnostic procedure, violations of the structure and density of bone matter are determined. Subsequently, a necrotic defect is discovered. The method allows you to clarify the size and exact location of the focus of bone destruction identified on x-rays.
- Scintigraphy . When conducting a static study, hyperfixation of the radiopharmaceutical in the lesion is noted. The intensity of accumulation depends on the activity of the process and the degree of blood supply disturbances. Dynamic scintigraphy at the initial stages indicates an increase, and at later stages a decrease in all phases of blood flow.
Treatment of Schlatter's disease
Treatment of osteochondropathy of the tibial tuberosity includes providing the affected limbs with rest, physiotherapy, exercise therapy, spa treatment, and the use of medications.
https://www.youtube.com/watch?v=6p3xX4DyC5s
Conservative treatment can be carried out on an outpatient basis. Treatment is carried out by a traumatologist, orthopedist or surgeon. Ensuring peace is achieved in the following ways:
- excluding physical stress on the body as a whole;
- refusal to engage in active sports;
- applying a fixing bandage or plaster cuff.
Since the main symptom of the disease is pain, the prescription of painkillers from the NSAID group is often required. Physiotherapy is indicated for a speedy recovery. In this situation, UHF therapy, magnetic therapy, and paraffin treatment can be performed. To normalize blood flow and reduce pain, massage of the lower extremities is often performed. Shock wave therapy is often performed to improve the condition of patients. Calcium electrophoresis provides a good therapeutic effect. Physical therapy is of great importance. It allows you to stretch the tendons in the knee area and the muscles themselves. After a full course of therapy, the patient is recommended to undergo sanatorium treatment. During it, hydrotherapy and mud treatment are carried out. During the rehabilitation period, it is necessary to limit the load on the knee joints.
In rare cases, if conservative treatment is ineffective, surgical intervention is performed. It is indicated for constant severe pain and fragmentation (crushing of bone structures). Surgical treatment is rarely performed. Thus, Schlatter's disease develops mainly in young people. Prevention of this pathology includes the use of protective equipment (knee pads), avoidance of permanent injuries, strengthening of the ligamentous apparatus, and a balanced diet.
Share link:
Causes
Necrosis of the femoral head occurs when this area is insufficiently supplied with blood. And most often, problems with blood supply occur with injuries, fractures, dislocations in the hip joint. As a result, due to lack of oxygen and nutrients, bone cells die. However, necrosis in the hip joint can begin without vascular damage. Factors that provoke non-traumatic avascular necrosis of the femoral head include: radiation and chemotherapy; taking corticosteroid hormones; vascular diseases and blood diseases; rheumatoid arthritis; osteoporosis; alcohol abuse and smoking; excessive stress on the joint; disturbance of mineral metabolism; diseases of the liver, adrenal glands.
Physical examination
When palpating the anterior surface of the leg, local pain is noted. With concomitant trauma to intra-articular structures, effusion or blood accumulates in the joint. Extension of the limb at the knee joint is limited or impossible. Tear of the tuberosity is often combined with other injuries, so when examining the knee joint, you need to pay special attention to pain on palpation of the joint space or instability of the joint - these symptoms indicate a meniscus tear or rupture of intra-articular ligaments, respectively. {banner_st-d-1}