Osteochondropathy of the patella refers to a group of diseases in which aseptic necrosis of bone tissue occurs. Destructive processes most often occur due to mechanical damage. The disease is quite rare and occurs in 3% of patients visiting orthopedic doctors. The pathology affects children, adolescents and men under 30 years of age. With timely treatment, the disease goes away without a trace, but can still lead to serious complications and even disability for the patient. Below we will take a closer look at the symptoms, treatment and causes of osteochondropathy of the patella.
What it is?
Osteochondropathy refers to several ailments that occur in the knee area. All diseases differ in location in the knee joint and symptoms. These include:
- Koenig's disease. Characterized by inflammation of cartilage tissue. Damaged pieces of cartilage separate or peel away from the bone. Their erratic movement along the joint capsule disrupts the movement of the joint itself. The inflammatory process occurs in cartilage tissue. In neglected form, its deeper parts die off. The pathology is common between the ages of 10 and 20 years. Moreover, it occurs 3 times more often in boys than in girls.
- Larsen-Johansson disease (osteochondropathy of the patella). With this disease, an improperly ossified patella causes pain, causes swelling, leads to hydroarthrosis, and limits mobility. The affected area is fragmentation of the patella. The risk group includes teenagers involved in sports between the ages of 10 and 15 years.
- Osgood-Schlatter disease. Characterized by pathological changes in the tibia. A growth appears in the tuberosity, which causes pain in the area of the kneecap. The disease causes microtrauma to the bones. It occurs in children and adolescents aged 8 to 16 years. Like Larsen's disease (osteochondropathy of the patella), it most often affects boys.
- Leuven's disease. Causes negative changes in the knee joint. Over time, the disease develops into intractable synovitis. In the early stages it is characterized by intermittent pain of moderate strength. Movements in the joint are preserved in full, but they are painless. Usually the process is one-way. Leuven's disease (osteochondropathy of the patella) develops between the ages of 12 and 14 years.
LiveInternetLiveInternet
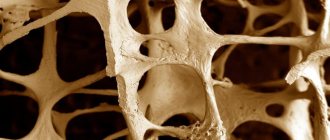
Osteochondropathy is a group of diseases characterized by the development of aseptic necrosis of the spongy substance of various skeletal bones subject to heavy mechanical load. In the area of the knee joint from this group, the following diseases occur in childhood and adolescence: • Koenig's disease (osteochondritis dissecans) - osteochondropathy of the articular surfaces of the knee and patellofemoral joint • Osgood-Schlatter disease - osteochondropathy of the tibial tuberosity • Sinding-Larsen-Johanson disease — osteochondropathy of the lower or upper pole of the patella. 1. Osteochondritis dissecans is a disease characterized by limited subchondral necrosis of the articular surface of the bone with the formation of an osteochondral fragment and its further migration into the joint cavity. The term “osteochondritis dissecans” was proposed by König (1887). The incidence of Koenig's disease ranges from 15 to 30 cases per 100,000 population. The average age of patients is from 10 to 20 years, cases have also been described in children 5 years of age. Boys get sick three to four times more often than girls. The location of the pathological focus in 75-85% of cases is the medial condyle of the femur, 6-13% of cases - the lateral condyle, 1-6% - the articular surface of the patella and less than 1% - the articular surface of the tibia. Bilateral damage to the knee joints is also possible - 20-30% of cases. To date, there is no consensus on the causes of osteochondritis dissecans. Existing theories can be combined into two main groups: the first is a theory supporting traumatic and the second is ischemic etiology. Osteochondritis dissecans is an intra-articular lesion, and Osgood-Schlatter and Sinding-Larsen-Johansson diseases are considered apophysitis.
Rice. 1. Localization of the pathological process in Osgood-Schlatter disease and Sinding-Larsen-Johansson disease.
2. Osgood-Schlatter disease - aseptic necrosis of the tibial tuberosity. The disease was described in 1903 by two surgeons: the American Robert Bayley Osgood (1873-1956) and, a few months later, the Swiss Carl Schlatter (1864-1934), after whom it was named. The disease is typical for childhood and adolescence. In 25-50% of cases, bilateral damage is observed. Boys get sick between the ages of 11 and 15, girls from 8 to 13 years. Among the cases, there is a predominance of boys, which is explained by more active behavior and greater involvement in sports. The etiology of the disease is unknown, but there are a large number of theories: avascular necrosis, endocrinopathy, structural changes in the patellar ligament and many others. In 1975, Ogden and Southwick, based on long-term histological studies, suggested that the cause of the development of Osgood-Schlatter disease is the formation of a secondary point of ossification due to the separation of a section of bone tissue from the center of ossification of the tibial tuberosity. Currently, the most accepted theory is repetitive microtrauma of the tibial tuberosity due to increased function of the quadriceps muscle.
3. Sinding-Larsen-Johanson disease is a disease characterized by pain in the anterior part of the knee joint and fragmentation of the lower or upper pole of the patella detected by radiography. In 1921 and 1922, Sinding-Larsen and Johansson independently described this pathology. The disease occurs in children and adolescents, with an average age of 10 to 14 years. The etiology of this disease is not completely known, however, it is assumed that Sinding-Larsen-Johansson disease has a similar etiology to Osgood-Schlatter disease . This assumption is confirmed by the description of these diseases in one patient. Due to the increased function of the quadriceps muscle, a rupture and separation of a section of bone tissue from the center of ossification of the patella occurs, which causes the development of avascular necrosis. The classical description of Sinding-Larsen-Johansson disease is considered as an apophysitis, and it is assumed that the focus of avascular necrosis occurs in the bone tissue directly at the insertion of the patellar tendon. Later, it was suggested that the pathological focus is localized in the proximal part of the patellar tendon, which causes calcification or ossification of this area, based on this, the disease is considered tendinitis. It should be noted that the diseases in question are more common in males who are actively involved in sports. Osgood-Schlatter and Sinding-Larsen-Johansson disease are observed only in childhood and adolescence, with the peak incidence occurring during puberty and due to rapid growth rates.
Clinic. The clinical picture of the diseases is similar in the absence of obvious symptoms in the initial stages of the disease, which requires caution from pediatricians, rheumatologists, pediatric surgeons, orthopedists and doctors of other specialties. The primary manifestations of osteochondropathy in the knee joint area are the appearance of pain. Pain occurs during physical activity, pain is not noted at rest, and the pain intensity is initially low. Some patients may only notice discomfort in the knee joint. Gradually, the pain becomes more intense and localized. With osteochondritis dissecans, pain is most often localized in the area of the medial condyle. Localization of pain in the anterior region of the knee joint is characteristic of osteochondritis dissecans of the patella, Osgood-Schlatter disease and Sinding-Larsen-Johansson disease. With the further development of the pathological process, the pain syndrome can become permanent, patients develop lameness, and develop limitation of active movements in the knee joint. The consequences of long-term pain syndrome in these diseases may be the development of hypotrophy of the quadriceps femoris muscle. The characteristics of the pain syndrome in Osgood-Schlatter and Sinding-Larsen-Johansson disease include a direct relationship between the appearance of pain and contraction of the quadriceps femoris muscle (climbing stairs, running). Patients note the inability to stand on the affected knee due to a sharp increase in pain. Upon objective examination, osteochondritis dissecans is characterized by an increase in the volume of the affected joint due to the development of synovitis. An increase in volume, or rather a change in the configuration of the affected joint, can also be observed with Osgood-Schlatter and Sinding-Larsen-Johansson disease , but in this case it will be caused by the development of bursitis and local changes: swelling and hyperemia in the area of the tibial tuberosity or the lower pole patella, respectively. By palpation, local pain can be detected; the pain point will correspond to the localization of the process
Rice. 2. Localization of the pain point in Osgood-Schlatter (left) and Sinding-Larsen-Johansson (right) disease.
At the terminal stages of diseases, conditions arise that can only be resolved surgically: joint blockade ( osteochondritis dissecans) and apophyseal avulsions. The insidiousness of these diseases lies in the fact that they can be asymptomatic and manifest themselves only in the terminal stages. The duration of the pain syndrome can range from several days to several years. Often, the disease manifests itself after a traumatic episode; here it is necessary to pay attention to the discrepancy between the traumatic factor and the developed consequences. Such conditions, in the absence of special studies, are interpreted as banal post-traumatic conditions (hemarthrosis, subchondral fractures, avulsion fractures, etc.). Diagnostics. During a physical examination of a patient with osteochondritis dissecans, a Wilson test can be performed, which is characteristic of a standard lesion of the medial condyle. Methodology: the patient sits on the edge of the table with his legs down, rotates the tibia inward (Fig. 3a) and extends the leg at the knee joint (Fig. 3b), bends the leg, with the next extension stops in a position of about 300 from full extension, rotates the tibia the bone outwards (Fig. 3c) and extends the leg (Fig. 3d). A positive Wilson's sign is the occurrence of pain in the knee joint in a position of about 300 from full extension, and a decrease in pain in this position with external rotation of the tibia. At stages 1-2 of the disease, the information content of the test is 62%
Rice. 3. Method of performing Wilson's symptom
Osgood-Schlatter disease is characterized by the appearance of pain or its intensification in the area of the tibial tuberosity when the tendon of the quadriceps femoris is pulled, for Sinding-Larsen-Johansson disease in the area of the lower pole of the patella with the same action (maximum flexion in the knee joint, creating resistance during extension in the knee joint). The X-ray method makes it possible to identify these diseases, however, when using it, it is necessary to take into account some features of the X-ray picture of the knee joint in children and adolescents and the possibilities for visualizing various structures. Osteochondritis dissecans: the ability to diagnose the disease from the 2nd stage (the radiograph shows an area of compaction in the subchondral zone of the epiphysis of the bone in the shape of a wedge, separated from the mother by a clearing strip). At stage 3, the lesion is clearly separated from neighboring sections by a stripe of clearing, which, depending on the duration of the disease and the degree of bone tissue resorption, has a different shape and width. There is a sclerotic border around the sequestrum. Stage 4 - X-ray reveals a defect in the articular surface and a fragment of bone tissue in the joint cavity
Rice. 4. Defect of the medial condyle of the femur with osteochondritis dissecans.
Osgood-Schlatter disease on X-ray examination is characterized by rarefaction or fragmentation of the trunk-shaped process of the anterior epiphysis of the tibia; some fragments may be shifted upward and forward; periosteal layers are possible. In the outcome stage there may be complete restoration of normal bone structure. Since there is a similarity between normal variants of ossification and the pathological process, it is impossible to establish a diagnosis only from the X-ray picture, without clinical data
Rice. 5. The tibial tuberosity is normal (left) and with Osgood-Schlatter disease (right).
Sinding-Larsen-Johansson disease. A lateral radiograph shows usuration of the anteroinferior contour and fragmentation of the lower pole of the patella (Fig. 6). When analyzing the radiograph, it is necessary to remember about the variants of the anatomy of the patella patellae bipartite and patellae tripartite.
Rice. 6. X-ray of an 11-year-old boy with Sinding-Larsen-Johansson disease.
CT scan. The method provides more accurate visualization of the pathological process in the diseases under consideration, but does not allow recognizing osteochondritis dissecans at the 1st stage, and difficulties arise in determining the condition of the soft tissues. The principles of analyzing the obtained data are similar to the x-ray method.
Fig.7. Computed tomogram for osteochondritis dissecans of the patella.
Magnetic resonance imaging. In the diagnosis of osteochondritis dissecans, the method is highly informative, allows diagnosing the disease in the initial stages, and makes it possible to visualize and assess the condition of the articular cartilage. In the diagnosis of Osgood-Schlatter and Sinding-Larsen-Johansson disease, there are no problems with recognizing anatomical variants and pathology, since the method is able to visualize the area of inflammatory infiltration, and it is also possible to determine the involvement of articular capsules and tendons in the pathological process. Ultrasonography. Ultrasound diagnostic capabilities osteochondropathy in the knee joint area with great accuracy, and it is also possible to assess the condition of X-ray negative structures of the knee joint. All the possibilities of this method can only be realized with a highly qualified specialist. Scintigraphy. The method is applicable for diagnosing this group of diseases at various stages, however, it is rarely used in pediatric practice. Arthroscopy. It is used in the diagnosis of osteochondritis dissecans , has a high diagnostic value at all stages of the disease, and also makes it possible to assess the condition of the articular cartilage, which is important in choosing treatment tactics. Another advantage is the possibility of simultaneous implementation of therapeutic measures in one complex with diagnostic ones. Differential diagnosis. The need for differential diagnosis between osteochondropathy of the knee joint is especially relevant in the initial stages of the disease. Osteochondritis dissecans, Osgood-Schlatter disease and Sinding-Larsen-Johansson disease are predominantly found in an identical group of patients - children aged 10 to 15 years, most often male and leading an active lifestyle, or professional athletes. It must be taken into account that osteochondritis dissecans can develop over a wider age range, in contrast to osteochondropathy of the tibial tuberosity and patella, which occur mainly during puberty. The disease begins with the appearance of pain in the knee joint, associated with physical activity and passing with rest. Osgood-Schlatter disease and Sinding-Larsen-Johansson disease manifest themselves as pain in the anterior part of the knee joint; the same localization of pain is characteristic of osteochondritis dissecans of the patella and the surface of the patella of the femur. The most characteristic site of pain for König's disease is the area of the medial condyle of the femur. Distinctive signs of osteochondritis dissecans will be the phenomena of synovitis, “mini-hemarthrosis.” In terms of differential diagnosis, a manual examination of the knee joint is quite informative: with osteochondritis dissecans, pain on palpation of the medial condyle; Osgood-Schlatter disease - local pain and swelling in the area of the tibial tuberosity; Sinding-Larsen-Johansson disease - pain occurs on palpation of the lower, less often the upper pole of the patella. Wilson's symptom and the load on the quadriceps tendon also help to navigate the pathology A fairly good information content of an X-ray examination allows one to definitively exclude or confirm the disease. An exception is osteochondritis dissecans , especially when the pathological focus is localized in the articular surface of the patella; in this case, additional diagnostic methods are justified.
Treatment. There are both conservative and surgical methods for treating these diseases. The approach to choosing treatment depends primarily on the stage of the disease, as well as the presence of complications. Conservative treatment of osteochondritis dissecans consists of limiting activity and unloading the joint; this can most optimally be achieved in childhood by immobilizing the limb. If the symptoms of the disease disappear and there are positive dynamics in diagnostic studies, a gradual increase in the load on the joint is allowed. In the absence of positive dynamics within 3 months, surgical treatment is indicated. In the treatment of osteochondritis dissecans, a more active use of surgical methods in the early stages has recently been introduced, as they are more effective. Surgical treatment is carried out using arthroscopic equipment and consists of osteoperforation, microfracture, fragment fixation, removal of the free osteochondral body, followed by abrasive mechanical chondroplasty. The absolute indication for surgical treatment is the presence of a free osteochondral body in the joint cavity. Treatment of Osgood-Schlatter disease and Sinding-Larsen-Johansson disease is similar, and in most cases is limited to conservative measures. Patients need to reduce activity in the knee joint: all movements that cause tension in the quadriceps and pain are excluded. In cases of severe pain, immobilization is used for a short period of time. To relieve pain and inflammation, analgesics and non-steroidal anti-inflammatory drugs are prescribed. Indications for surgical treatment are apophyseal avulsions and repeated exacerbations during conservative treatment. Also, in rare cases, removal of a separated bone fragment or resection of the tibial tuberosity is used if pain persists and for cosmetic purposes. Forecast. With osteochondritis dissecans, the younger the patient, the more favorable the outcome of the disease. The prognosis also depends on the stage of the disease and the size of the pathological focus. In children, when the disease is identified and adequately treated in the initial stages, complete recovery is observed. The formation of large defects of the articular surface in adolescence leads to the rapid development of gonarthrosis. The prognosis for Osgood-Schlatter disease and Sinding-Larsen-Johansson disease is favorable, the symptoms of the disease resolve within a year with complete restoration of knee joint function. There may be discomfort in the knee joint for about 2 to 3 years. In rare cases, when separating a bone fragment and fixing it in the patellar tendon, pain and discomfort may bother the patient for quite a long time
Causes
The most common causes of knee pain are overuse and knee injuries. That is why active children and adolescents most often suffer from ACP. In addition, this pathology can occur in men under 30 years of age. ACP is much less common in older people. Symptoms of patellar osteochondropathy may also occur for other reasons:
- Flat feet.
- Scoliosis and other forms of spinal curvature.
- Hereditary predisposition.
- Improper metabolism.
- Obesity.
- Poor circulation in the legs.
Reasons for the development of the disease
The onset of the disease usually occurs between the ages of 2 and 12 years, although it can occur up to 19 years of age.
Children aged 4-8 years are most often affected, with boys getting sick 3-5 times more often than girls.
Presumably, the following factors may be triggering factors in the occurrence of Perthes disease:
- small, so small that it can go unnoticed, mechanical injury (bruise, sprain, awkward movement, etc.);
- inflammation of the hip joint (transient synovitis) due to past infections (sore throat, flu, etc.);
- metabolic disorders that are involved in the formation of bones (phosphorus, calcium and other minerals).
A tendency to myelodysplasia, genetically determined structural features of the hip joint are a hereditary predisposition to the development of this disease.
Symptoms
Usually at the very beginning of the disease there are no obvious signs. The first sign is the appearance of short-term painful sensations during physical activity. In a calm state, the patient, as a rule, does not experience any discomfort. After some time, the pain intensifies and a focus appears.
Painful sensations in the kneecap may indicate that the patient suffers from Larsen-Johansson disease. If the lesion is in the area of the medial condyle, then it is osteochondritis dissecans of the patella.
Pathology appears more often in children than in adults. In the first and second stages of the disease, the patient experiences a dull aching pain in the knee. This period is characterized by the destruction of articular cartilage. It becomes difficult to bend and straighten it, and discomfort arises. The muscle corset becomes weak, swelling appears.
Over time, osteochondropathy of the lower pole of the patella, as well as the upper one, causes a peculiar crunch and the person begins to limp. At the third stage, the course of the disease worsens: bone and cartilage tissues are destroyed, pain becomes very strong, the joint becomes inflamed and deformed, swelling of the knee can be seen with the naked eye, muscle tissue atrophies.
While walking, the patient limps very strongly, and a constant crunching sound is heard when bending the knee.
Development of the pathological process
The course of all osteochondropathy is characterized by 5 successive stages:
- Aseptic necrosis. This stage lasts up to several months and is manifested by pain in the affected area. The onset of the disease is not accompanied by changes on x-ray, but at 2-3 months of progress a weak local compaction of the bone substance is revealed.
- Impression fracture. It is characterized by further disruption of the structure of the bone area and its compaction. The expansion of the joint space begins. The stage lasts on average until the end of the 6th or beginning of the 7th month of the disease.
- Resorption. The dead area of bone is divided into small fragments. The articular surface of the bone is deformed. The duration of the stage is from six months to 2-3 years.
- Reparative (restorative), during which dead bone tissue is replaced by newly formed rough bone substance. This process takes from 6 months to 2 years.
- At the final stage, the affected area is completely replaced by altered tissue.
The development of aseptic necrosis is usually preceded by either mechanical trauma or prolonged ischemia (lack of blood supply). As compensation, an inflammatory process occurs. But if the traumatic effect continues, as for example in the case of high sports loads, or ischemia persists, and even more so if it is aggravated by taking anti-inflammatory drugs that block compensatory inflammation, the stage of necrosis occurs. In other words, the death of bone or cartilage tissue occurs.
The pathological process often ends with deformation of the affected area, the severity of which will depend on the correct choice of therapy and complete unloading of the joint during the illness. Lack of treatment or incorrect patient management tactics can lead to the development of persistent bone deformation and secondary osteoarthritis in the child.
Diagnostics
You cannot make a diagnosis yourself. Only an experienced doctor, depending on the symptoms and severity of the disease, can select the appropriate type of diagnosis. The five most commonly used methods are:
- Ultrasonography. It can only be done by a highly qualified specialist. He is able to see a reliable clinical picture of the disease. Ultrasound accurately determines the diagnosis and stage of the disease.
- Scintigraphy. Another highly effective method. Unfortunately, it only applies to children. Osteochondropathy of the patella using this method is determined at any stage.
- Magnetic resonance imaging helps to clearly examine the joint affected by Koenig's disease. With the help of MRI, pathology is determined even at the initial stage. An objective assessment of the state of the affected area at a given time is given. ACON is diagnosed by magnetic resonance imaging in all four types of the disease.
- In the early stages, differential diagnosis is relevant.
- Arthroscopy. Mainly used to recognize Koenig's disease. It is effective at all stages of the disease and helps to make a diagnosis with high accuracy, as well as choose an effective method of treatment in the future.
In some cases, pathology is determined using x-rays. Osteochondropathy of the patella is diagnosed using the method that the doctor considers most suitable for each individual patient.
Conservative treatment
Treatment of osteochondropathy of the patella is carried out according to one principle and generally gives a positive result with drug therapy. To relieve swelling and pain, ointments and analgesics with anti-inflammatory effects are prescribed: Ibuprofen, Diclofenac. In this case, the patient is recommended to reduce the load on the sore knee as much as possible and eliminate any movements in the joint.
A cast may be applied for up to two months. To activate the processes of restoration of cartilage tissue, chondroprotective drugs are used. You can find many ointments with glucosamine and chondroitin on the open market: “Chondroitin sulfate”, “Glucosamine Maximum” and others. During treatment, physiotherapy is also carried out - electrophoresis, paraffin applications. In addition, Neuromultivit vitamins are prescribed. If all recommendations are followed, OCP can be cured within one year. If there are no positive results after three months from the start of therapy, the issue of surgical intervention is discussed.
Patellofemoral arthrosis of the knee joint
In addition to the femur and tibia, the patella (patella) is another component of the knee joint.
It performs the main function in flexion and extension of the leg. When you bend your leg, the kneecap moves up and down like a groove in the bone of the upper leg between the two condyles. © Istockphoto.com / MedicalArtInc Patellofemoral arthrosis of the knee is caused by degenerative changes at the back of the patella (kneecap). Due to retropatellar arthrosis, arthrosis pain occurs primarily when a person descends from stairs or from a mountainous surface. In addition to the femur (Femur) and tibia (Tibia) bones, the patella is another component of the complex knee joint. The functionality of the knee joint also depends on the condition of the patella. Retropatellar arthrosis occurs most often in masons, tilers - people who do their work mainly on their knees, or in people whose work involves physical activity. Patellofemoral arthrosis can also occur due to unsuccessful surgery or deformation of the kneecap (knee dysplasia). Patellofemoral arthrosis of the knee joint is also observed in runners. Women suffer from this disease more often than men.
With arthrosis, the articular cartilage between the kneecap and the femur wears away due to pressure and inflammation (articular cartilage wear).
The condition of the patella is of great importance for the extensor movement of the knee joint during walking or standing. When a person bends his leg, the patella slides along the patellar groove of the femur, and when he straightens it, it moves forward. At this moment, patients feel a “failure” in the joint, but in reality, dislocation rarely occurs. Full functionality of the patella is also very important after knee surgery. Immediately after surgery, our knee specialists recommend restoring movement in the joint and foot, as this improves blood supply to the muscles of the lower limb and prevents swelling and blood clots. When the leg is flexed or extended, the kneecap moves up and down along the grooves of the tibia and femur, preventing their displacement. Additional fixation is provided by the patellar meniscus ligament and the quadriceps femoris tendon.
Patellofemoral arthrosis, x-ray: In this image, the patient lies on his back, legs bent at the knees. The image shows the condition of the joint space with two femoropatellar joints. On the left you can see the satisfactory condition of the joint space. The kneecap (patella) and the patella surface of the femur are located at a distance of more than 3 mm. from each other. Patellofemoral arthrosis is visible on the right: The patella and femur touch each other, the cartilaginous layer is completely worn out.© Gelenk-Klinik.de Anatomical image of a healthy knee and patella, lateral and cruciate ligaments, as well as the meniscus. Patellofemoral arthrosis is observed between the two condyles of the femur, the so-called femoropatellar sliding groove. Each person's kneecap and patellar surface of the femur are formed differently. In some patients, the structure of these elements leads to instability of the femoropatellar joint. In this case, there is a high position of the patella (patella alta) or its slight protrusion. The above factors can cause retropatellar arthrosis. © Istockphoto.com/MedicalArtInc
The onset of degenerative changes in the patellofemoral joint is marked by softening of the articular cartilage. This pathology is called “Chondromalacia,” during which morphological changes are observed in the cartilage of the patella. The onset of the disease can be acute injuries to the knee, but most often the disease is based on chronic overload of the patellofemoral joint.
Patellofemoral arthrosis is often accompanied by tibiofemoral (tibiofemoral) arthrosis of the knee joint. Often, arthrosis also damages the lateral (outer) part of the knee joint. Thus, patellofemoral arthrosis is often accompanied by an X-shaped (valgus) deformity of the external tibiofemoral part of the knee joint.
In 5-10% of patients, arthrosis behind the patella appears in an isolated form, without affecting the important components of the knee joint. In this case, patellofemoral arthrosis must be treated with special attention to prevent damage to the entire knee joint.
Surgical method
Surgical treatment involves the use of arthroscopic equipment to surgically restore the joint. During the operation, the cartilage formation is removed and new cartilage is grafted. The reason for surgery may be a recurrence of the disease. In some cases, surgery may be performed to remove the broken joint elements. Often, such treatment is the only way to maintain the shape of the knee and its full functioning.
After the operation, you must remain calm and avoid any physical activity. Violation of the doctor’s recommendations can lead to joint deformation and complications in the form of secondary osteochondrosis of the patella.
How is patellofemoral arthrosis of the knee joint diagnosed?
History of the disease
- Is there bilateral knee pain?
- Are there any knee injuries?
- Is there swelling of the knee?
- Does your knee hurt when you start to move your leg?
- Do you feel knee stiffness in the morning?
- Does knee pain get worse when walking?
- Is there general weakness in the knee?
- Is knee pain reducing your maximum walking distance?
- Are there any restrictions in the movement of the knee?
When taking a medical history, the patient tells the doctor about his pain and symptoms. For the effectiveness of the examination and correct diagnosis, the doctor determines whether the patient has experienced repeated pain in the anterior part of the knee and dislocation of the patella.
The patient is also asked questions regarding accidents in which a patella bruise could occur. In addition, factors such as physical activity during work and patellar subluxation play an important role in making the diagnosis. First, a clinical examination is performed, during which the specialist checks the mobility and stability of the knee joint and observes the patient's gait. At the same time, the doctor pays special attention to the mobility of the patella during flexion. Also, a qualified orthopedist at our Gelenk-Klinik in Fribourg determines the degree of swelling of the knee and checks whether the temperature of the knee has increased due to arthrosis caused by the inflammatory process.
Diagnosis of patellofemoral arthrosis depends on the symptoms of the disease. During preventive medical examinations of patients without any complaints of pain in the patella, specialists still note a crunching sound or excessive mobility of the patella. These patients had never seen a doctor for knee pain and therefore did not require medical intervention.
Exercise therapy for osteochondropathy of the patella
Physical therapy is indicated during the period of immobilization. While the affected limb is fixed in a splint, the patient should use general developmental exercises. It can be:
- dynamic movements (extensor, flexion, rotation) of a healthy limb;
- rhythmic contraction of the muscles of the injured leg;
- holding the leg with the cast suspended;
- ideomotor exercises – visualization of movement in a joint.
It is necessary to start exercises a few days after surgery and plaster application, but only with the permission of the doctor. Use your healthy leg to perform any movements - move it to the side, lift it, do circular rotations, swings, statically tense the muscles.
The load on the torso muscles is also performed - the shoulders and head are raised, the position is fixed for several seconds. A few days after the operation, the patient is recommended to briefly lower the sore leg from the bed, and then raise it above the body. Walking around the ward is allowed on crutches, without support on the operated leg.
Complications
As mentioned above, most often children and adolescents are exposed to ACN, who are characterized by increased load on the legs and knee injuries. Treatment of this disease takes a long time. Sometimes it lasts for more than one year. Most often, the disease resolves without any complications for patients. Children's cartilage and bones are quickly renewed and restored. In older people, osteochondropathy is more difficult to treat and takes longer. In advanced cases, the following complications may occur:
- Arthrosis of the knee joint.
- One leg may become shorter than the other by a couple of centimeters.
- Due to the difference in the length of the limbs, the spine can be deformed and scoliosis can develop.
Without surgical intervention, lameness may remain for the rest of your life. If a child, after a bruise or other joint injury, remains at rest and does not load the joint, osteochondropathy of the patella may go away on its own. But this happens very rarely.
Patellofemoral arthrosis: causes
Causes of patellofemoral arthrosis
- Dysplasia of the patella and patella of the femur (47%)
- Injuries: Fractures, osteochondral lesions (8%)
- Idiopathic factors: Excess weight, excessive exercise (41%)
- Patella hypermobility, muscle imbalance (4%)
Very often, patellofemoral arthrosis occurs due to instability of the patella, which causes insufficient tension in the ligaments that fix and support it. Violation of the natural functions and shapes of the kneecap is also the cause of this disease. Changes in the shape of the patella can cause it to move out of its normal position and become dislodged from its sliding support. Such disorders are often accompanied by instability and dislocation of the patella.
Osteoarthritis of the knee joint: internal and external damage. Patella with obvious damage to the cartilage of the femoropatellar joint. Characteristic at the progressive stage of arthrosis is the formation of bone growths (osteophytes). © Viewmedica
Well-known factors such as excess weight put stress on the patellofemoral joint, especially in older people.
In younger patients, patellofemoral arthrosis is caused mainly by deformation of the knee joint or deformation of the patellar surface, overload and deformation of the patella. Another cause of this disease is injury.
Reconstruction of the anterior cruciate ligament after a fracture using part of the patella tendon can also cause patellofemoral arthrosis of the knee.
Isolated patellofemoral pathology without disruption of the forms and functions of other parts of the knee joint is very often accompanied by an O-shaped curvature of the legs (varus deformity).
Prevention
It is impossible to prevent knee injury, but you can reduce the risk of developing pathological processes. It is necessary to follow simple rules in relation to all family members:
- If you have knee pain, be sure to visit an orthopedic surgeon.
- The child must know the safety rules and the dangers of severe bruises and falls.
- To identify the disease at an early stage, you should undergo regular medical examinations.
- Excessive physical activity should be avoided.
In addition, preventive measures that prevent the occurrence of osteochondropathy are exercises in the pool and therapeutic massage. To avoid Osgood-Schlatter disease, athletes are recommended to use knee pads with soft inserts during training, or sew foam pads onto sportswear.
Patellofemoral arthrosis: Symptoms
Symptoms of patellofemoral arthrosis
- Pain in the front of the knee.
- Pain when climbing stairs.
- Pain when rising from a chair after a long sitting position.
- Swelling and hyperthermia.
- Pain when squatting.
- Crunching sounds in the joints.
Patients with patellofemoral syndrome typically have pain in the front of the knee, primarily after walking down stairs, rising from a chair, bending their knees, or squatting. Often patients feel a certain crunch in the joint behind the patella or numbness. Sometimes the knee seems to be completely motionless, especially when there is bone-on-bone friction at the joint between the patella and the femur. Inflammatory diseases cause increased temperature in the patellofemoral joint and effusion of the knee joint.